Hypertension
Learn about hypertension, a condition where blood pressure in the arteries is elevated. Discover its definitions, pathophysiology, classification of blood pressure measurements, and guidelines for management. Explore the impact on cardiovascular health and ways to address this common health concern.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Blood pressure in the arteries is elevated. This requires the heart to work harder than normal to circulate blood through the blood vessels. Blood pressure is summarised by two measurements, systolic and diastolic, which depend on whether the heart muscle is contracting (systole) or relaxed between beats (diastole) .
DEFINITION SIR GEORGE PECKERING first formulated a concept that blood pressure in a population is distributed continuously as a bell shaped curve with no real separation between normotension and hypertension. As a consequence, the dividing line between normal and high blood pressure can be defined only in an operational way.
As intervention trials only included adults aged 18 years or older, definition and classification of hypertension refers to adults not taking anti- hypertensive drugs and not actually ill, based on average of two or more readings on two or more occasions
PATHOPHSIOLOGY OF HYPERTENSION Myocardial contractility Stroke volume Cardiac output Size of the vascular compartment Heart rate Arterial pressure Vascular structure Peripheral resistance Vascular function
JNC 7-Classification of blood pressure measurements Category Systolic blood pressure (mm of Hg) Diastolic blood pressure (mm of Hg) Normal <120 <80 Prehypertension 120-139 or 80-90 Hypertension Stage I 140-159 or 90-99 Stage II 160 or 100
In 2014, the Eighth Joint National Committee (JNC 8) published the evidence-based guideline for the management of high BP in adults. This new guideline was characterized by a systematic review of the literature with an emphasis on randomized, controlled clinical trials.
THE GUIDELINE ATTEMPTED TO ANSWER 3 KEY QUESTIONS. In adults with HTN, does initiating antihypertensive pharmacologic therapy at specific BP thresholds improve health outcomes? In adults with HTN, do attempts to reach specified BP goals with antihypertensive pharmacologic therapy lead to improvements in health outcomes? In adults with HTN, do various antihypertensive drugs or drug classes differ in regard to specific health outcomes?
The new guidelines emphasize control of systolic blood pressure (SBP) and diastolic blood pressure (DBP) with age- and co morbidity-specific treatment cut-offs. The new guidelines also introduce new recommendations designed to promote safer use of angiotensin converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs).
IMPORTANT CHANGES FROM THE JNC 7 GUIDELINES INCLUDE THE FOLLOWING: In patients 60 years of age or older who do not have diabetes or chronic kidney disease, the goal blood pressure level is now <150/90 mmHg In patients 18 to 59 years of age without major co- morbidities, and in patients 60 years of age or older who have diabetes, chronic kidney disease, or both conditions, the new goal blood pressure level is <140/90 mmHg
First-line and later-line treatments should now be limited to 4 classes of medications: 1) Thiazide-type diuretics, 2) Calcium channel blockers (CCBs), 3) ACEIs, and 4) ARBs Second- and third-line alternatives included higher doses or combinations of ACEIs, ARBs, thiazide- type diuretics, and CCBs
Several medications are now designated as later-line alternatives, including the following: Beta-blockers Alpha-blockers Alpha1/beta-blockers (eg, carvedilol) Vasodilating beta-blockers (eg, nebivolol) Central alpha2-adrenergic agonists (eg, clonidine) Direct vasodilators (eg, hydralazine) Loop diuretics (eg, furosemide) Aldosterone antagonists (eg, spironolactone) Peripherally acting adrenergic antagonists (eg, reserpine)
When initiating therapy, patients of African descent without chronic kidney disease should use CCBs and thiazides instead of ACEIs Use of ACEIs and ARBs is recommended in all patients with chronic kidney disease regardless of ethnic background, either as first-line therapy or in addition to first-line therapy ACEIs and ARBs should not be used in the same patient simultaneously
CCBs and thiazides-type diuretics should be used instead of ACEIs and ARBs in patients over the age of 75 with impaired kidney function due to the risk of hyperkalemia, increased creatinine, and further renal impairment The change to a more lenient systolic blood pressure goal may be confusing to many patients who are accustomed to the lower goals of JNC 7, including the <140/90 mmHg goal for most patients and <130/80 mmHg goal for patients with hypertension and major co morbidities.
Classification of blood pressure (WHO) Category Systolic blood pressure (mm of Hg) Diastolic blood pressure (mm of Hg) Normal < 130 < 85 High normal 130-140 85-90 Hypertension Mild (stage I) 140-159 90-99 Moderate (stage 2) 160-179 100-109 180 Severe (stage 3) >110
When systolic and diastolic blood pressure falls in different categories, the higher category should be selected to classify individual blood pressure. isolated systolic hypertension is defined as systolic blood pressure of 140 mm or more and diastolic blood pressure less than 90 mm of Hg.
BLOOD PRESSURE MEASUREMENT Accurate measurements are essential under standardized conditions for valid comparison between persons or groups over time. WHO study group recommended The sitting position than supine position for recording blood pressure. Uniform policy should be adopted either right or left arm.
BLOOD PRESSURE MEASUREMENT cont .. The pressure at which the sounds are first heard (phase I) is taken to indicate the systolic pressure. Near the diastolic pressure the sound first become muffled (phase IV) and than disappear (phase V). Most of studies used phase V to measure diastolic blood pressure.
BLOOD PRESSURE MEASUREMENT cont .. The systolic and diastolic blood pressure should be measured at least 3 times over a period of at least 3 minutes and lowest reading recorded. For comparability the data recorded everywhere in a uniform way.
Pulse pressure (the difference between systolic and diastolic blood pressure) is frequently increased in older people with hypertension. This can mean that systolic pressure is abnormally high, but diastolic pressure may be normal or low a condition termed isolated systolic hypertension. The high pulse pressure in elderly people with hypertension or isolated systolic hypertension is explained by increased arterial stiffness, which typically accompanies aging and may be exacerbated by high blood pressure.
Many mechanisms have been proposed to account for the rise in peripheral resistance in hypertension. Most evidence implicates either disturbances in renal salt and water handling (particularly abnormalities in the intra-renal renin-angiotensin system) and/or abnormalities of the sympathetic nervous system. These mechanisms are not mutually exclusive and it is likely that both contribute to some extent in most cases of essential hypertension.
It has also been suggested that endothelial dysfunction and vascular inflammation may also contribute to increased peripheral resistance and vascular damage in hypertension.
TYPES PRE HYPERTENSION: SBP: 120-139 mmHg DBP: 80-89 mmHg HYPERTENSION STAGE I: SBP: 140-159 mmHg DBP: 90-99 mmHg HYPERTENSION STAGE II: SBP: More or equal to 160 mmHg DBP: More or equal to 100 mmHg PREGNANCY INDUCED HTN: because of increased production of hormones and enzymes during pregnancy.
CLASSIFICATION Primary (essential) hypertension Secondary hypertension PRIMARY (ESSENTIAL) HYPERTENSION When causes are unknown Most prevalent form Accounting for 90% of all cases of hypertension.
SECONDARY HYPERTENSION When some other disease process or abnormality involved in its causation. Diseases of kidney (chronic glomerulo- nephritis and chronic pyelonephritis) tumors of account for only 10%.
In most people with established essential (primary) hypertension, increased resistance to blood flow (total peripheral resistance) accounting for the high pressure while cardiac output remains normal. There is evidence that some younger people with pre- hypertension or 'borderline hypertension' have high cardiac output, an elevated heart rate and normal peripheral resistance, termed hyperkinetic borderline hypertension. These individuals develop the typical features of established essential hypertension in later life as their cardiac output falls and peripheral resistance rises with age. Whether this pattern is typical of all people who ultimately develop hypertension is disputed. The increased peripheral resistance in established hypertension is mainly attributable to structural narrowing of small arteries and arterioles,
although a reduction in the number or density of capillaries may also contribute. Hypertension is also associated with decreased peripheral venous compliance which may increase venous return, increase cardiac preload and, ultimately, cause diastolic dysfunction. Whether increased active vasoconstriction plays a role in established essential hypertension is unclear.
MAGNITUDE OF THE PROBLEM Arterial hypertension is frequent, worldwide health disorder.
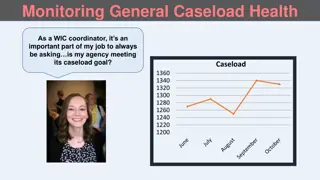
RULES OF HALVES Hypertension is an iceberg disease In early 1970s that only half of hypertensive subjects in general population in most developed countries were aware of the condition, only half of those aware were being treated, and those who were treated only half were considered adequately treated. This is situation in highly developed countries the proportion treated in developing countries would be far too less.
3 5 1 7 3 2 1233 5 7 4 9 6 8
RULES OF HALVES cont. Areas of the circles represent number wise as- 1-The whole community. 2-Normotensive subjects. 3-Hypertensive subjects. 4-Undiagnosed hypertension. 5-Diagnosed hypertension. 6-Diagnosed but untreated. 7-Diagnosed treated. 8-Inadequately treated. 9-Adequately treated.
INCIDENCE Worldwide raised blood pressure is estimated to cause 7.5 million deaths, About 12.8% of the total of annual deaths. Accounts for 57 million DALYs or 3.7% of total DALYs. Major risk factor for CHD and IHD as well as hemorrhagic stroke. Risk of CVD doubles with each increase of 20/10 mm of Hg
COMPLICATIONS OF RAISED BLOOD PRESSURE- Heart failure Peripheral vascular disease. Renal impairment. Retinal hemorrhage. Visual impairment. Treating systolic and diastolic blood pressure below 140/90 reduction in cardio-vascular complications.
Overall prevalence of raised blood pressure in adults aged 25 years and over was around 40% in 2008. Proportion with world s population with high blood pressure or uncontrolled hypertension, fell modestly between 1980 and 2008. However, because of population growth and ageing number of people with hypertension rose from 600 million in 1980 to 1 billion in2008.
Income groups of countries, the prevalence of raised blood pressure was consistently high, with low, lower-middle and upper-middle- income countries. All having rates around 40% Prevalence in high-income countries was lower, 35% for both sexes.
PEVALENCE IN INDIA- Community based survey by ICMR during 2007-08 to identify risk factor for non- communicable diseases under State based Integrated Disease Surveillance Project Phase I in A.P., Kerala, M.P., Maharashtra, Uttrakhand, T.N. and Mizoram. 17-21% prevalence in all States with marginal rural-urban difference
Overall pattern was found increasing with age groups in all States. High in high educational level of Uttrakhand, Mizoram and M.P. More prevalent among executive and service categories in all States.
TRACKING OF BLOOD PRESSURE If level of blood pressure is followed up over a period of years from early childhood to adult life, those whose blood pressure was initially high would probably continue in the same track as adults. This phenomenon called as tracking Applied to identifying children and adolescents at risk
Blood pressure Time
RISK FACTORS FOR HYPERTENSION NON-MODIFIABLE MODIFIABLE Age Obesity Sex Salt intake Genetic factors Saturated fat Ethnicity Dietary fibre Alcohol Heart rate Physical activity Environmenental stress Socio-economic status Other factors
NON-MODIFIABLE RISK FACTORS 1-Age- Blood pressure rises with age in both sexes. Rise is greater in those with higher initial blood pressure. Some population identified whose blood pressure does not rise with age. These communities are for the most part primitive societies with calorie often salt intake at subsistence level.
NON-MODIFIABLE RISK FACTORS CONT 2-Sex- Early in life there is little evidence of difference in blood pressure between sexes. In adolescence male with a higher average level. Late in life the difference narrowed and pattern may even reversed. Post-menopausal changes in women may be contributory factor.
NON-MODIFIABLE RISK FACTORS CONT 3-Genetic factors- Blood pressure levels in part determined by genetic factors. Inheritance is polygenic. Based on twin and family studies. Blood pressure of monozygotic twins usually more strongly correlated than those of zygotic twins. No significant correlation between husband and wives, between adopted children and adoptive parents.
NON-MODIFIABLE RISK FACTORS CONT Family studies showed that children of two normotensive have 3% possibility of developing hypertension, while this possibilities is 45% in children of two hypertensive parents. Blood pressure among first degree adults relatives also statistically significant. Genetic markers and mechanism of heredity not yet been conclusively elucidated.
NON-MODIFIABLE RISK FACTORS CONT 4-Ethnicity- Higher blood pressure levels in black community. Average difference between blood pressure of two groups vary less than 5 mm of Hg. In 2nd decade of life to 20 mm of Hg. In 6th decade. Black Americans of African origin have higher blood pressure level than whites.
MODIFIABLE RISK FACTORS 1-OBESITY- Obesity is risk factor for hypertension. The greater weight gain greater the risk of high blood pressure. Loss of weight decrease in blood pressure. Central obesity indicated by increased waist- hip ratio positively correlated with high blood pressure.
MODIFIABLE RISK FACTORS cont 2- Salt intake- High salt intake (7-8 gm./ day) increases blood pressure proportionately. Low salt intake lower blood pressure. Besides sodium other mineral elements potassium are determinants of blood pressure. Potassium antagonizes biological effect of sodium, there by reduces blood pressure. Other cations like calcium, cadmium, magnesium also reduces blood pressure.
MODIFIABLE RISK FACTORS cont 3-SATURATED FAT Saturated fat raises serum cholesterol that by blood pressure. Dietary fat should be limited 15-20% of total energy intake. Saturated fats contribute no more than 10p% of total energy intake. LDL and VLDL fractions are atherogenic and HDL exerts a protective effect against development of atherosclerosis.