Hypocalcemia: Causes, Management and Treatment Standards
Hypocalcemia is a common problem affecting serum calcium levels, with various causes including issues with PTH, vitamin D, and hyperphosphatemia. Learn about the etiology, common causes, and treatment standards for both acute and chronic cases of hypocalcemia.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Hypocalcemia Dr. Behrang Motamed Endocrinologist Assistant professor of Guilan university of medical science
RATIONALE Hypocalcemia is a common problem, treatable, but sometimes difficult to manage long-term. There are both acute and chronic situations associated with low blood calcium.
LEARNING OBJECTIVES Understand the causes of low calcium, either with low or high parathyroid hormone (PTH). Define treatment standards for acute and chronic hypocalcemia.
OVERVIEW The major factors that influence the serum calcium concentration are PTH vitamin D calcium ion phosphate.
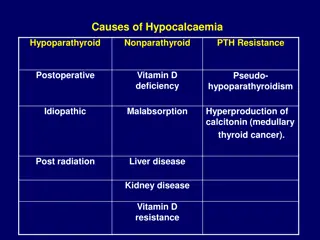
Low serum calcium concentrations are most often caused by disorders of : PTH Vitamin D. Hyperphosphatemia.
Serum calcium concentrations are normally maintained within the very narrow range that is required for the optimal activity of the many extracellular.
Total normal calcium range is between 8.5 and 10.5 mg/dL. The normal range of ionized calcium is 4.65 to 5.25 mg/dL .
Calcium in the blood is transported: bound to plasma proteins (45%) notably albumin bound to small anions such as phosphate and citrate (15%) free or ionized state (40%)
The Most Common Causes You Will See Low albumin: The serum total calcium concentration falls ;0.8 mg/dL for every 1 g/dL reduction in the serum albumin concentration. Changes in blood pH: Acidosis reducing the binding of Ca to Alb and alkalosis enhancing it.
CAUSES OF LOW CALCIUM AND LOW PTH Surgical hypoparathyroidism It may be transient, with recovery in days, weeks, or months, permanent, or even intermittent.(
Autoimmune: immune-mediated destruction of the parathyroid glands. Activating antibodies to the CaSR that decrease PTH secretion.
Other causes: Hypomagnesemia parathyroid gland destruction: irradiation infiltrative diseases of the parathyroid glands (hemochromatosis, Wilson disease, granulomas, or metastatic cancer).
CAUSES OF LOW CALCIUM AND HIGH PTH Vitamin D deficiency or resistance CKD PTH resistance Hyperphosphatemia Acute pancreatitis and sepsis
DRUGS THAT CAN CAUSE HYPOCALCEMIA Calcium chelators such as foscarnet, EDTA, and sodium citrate from plasma. Bisphosphonates Cinacalcet Chemotherapy Drugs like cisplatin
MANAGEMENT OF HYPOCALCEMIA Initially, intravenous (IV) calcium 1 to 2 g of calcium gluconate equivalent to 90 to 180 mg elemental calcium, in 50 mL of 5% dextrose) can be infused over 10 to 20 minutes. Note: The calcium should not be given more rapidly because of the risk of serious cardiac dysfunction, including cardiac arrest.
This dose of calcium gluconate will raise the serum calcium concentration for only 2 or 3 hours; as a result, it should be followed by a slow infusion of calcium in patients with persistent hypocalcemia.
An IV solution containing 1 mg/mL of elemental calcium is prepared by adding 11 g of calcium gluconate (equivalent to 990 mg elemental calcium) to normal saline or 5% dextrose water to provide a final volume of 1,000 mL.
This solution is administered at an initial infusion rate of 50 mL/h (equivalent to 50 mg/h).
The dose can be adjusted to maintain the serum calcium concentration at the lower end of the normal range.
Patients typically require 0.5 to 1.5 mg/kg of elemental calcium per hour.
IV calcium should be continued until the patient is receiving an effective regimen of oral calcium and vitamin D.
For patients with hypoparathyroidism, calcitriol (in a dose of 0.25 to 0.5 micg twice daily) and oral calcium (1 to 4 g of elemental calcium carbonate daily in divided doses) should be initiated as soon as possible.
Hypomagnesemia In patients with hypomagnesemia, hypocalcemia is difficult to correct without first normalizing the serum magnesium concentration.
If the serum magnesium concentration is low, 2 g (16 mEq) of magnesium sulfate should be infused as a 10% solution over 10 to 20 minutes, followed by 1 g (8 mEq) in 100 mL of fluid per hour.
Magnesium repletion should be continued as long as the serum magnesium concentration is ,0.8 mEq/L (1 mg/dL or 0.4 mmol/L).
More careful monitoring is required in patients who have impaired renal function who are at greater risk of developing hypermagnesemia.
Milder degrees of hypocalcemia In milder degrees of hypocalcemia (serum corrected calcium concentration of 7.5 to 8.0 mg/dL (oral calcium supplementation is preferred These patients are usually asymptomatic or at most mildly symptomatic (e.g., oral paresthesias)
They can be treated initially with 1,500 to 2,000 mg of elemental calcium given as calcium carbonate or calcium citrate daily, in divided doses.
For such patients with milder degrees of acute hypocalcemia and milder symptoms of neuromuscular irritability, who do not have symptomatic improvement with oral calcium supplementation, we switch to IV calcium.
IV calcium is also indicated to prevent acute hypocalcemia in patients with milder degrees of hypocalcemia or chronic hypocalcemia (due to hypo- parathyroidism) who become unable to take or absorb oral.
REFERENCES 1. Hannan FM, Thakker RV. Investigating hypocalcaemia. BMJ. 2013; 346:f2213. 2. Fitzpatrick LA, Arnold A. Hypoparathyroidism. In: De Groot LJ, ed. Endocrinology. 3rd ed. Philadelphia, PA: Saunders; 1995:1123. 3. Rosen CJ, Brown S. Severe hypocalcemia after intravenous bisphosphonate therapy in occult vitamin D deficiency. N Engl J Med. 2003;348(15):1503 1504. 4. Kearney T, Dang C. Diabetic and endocrine emergencies. Postgrad Med J. 2007;83(976):79 86. 5. Hannan FM, Thakker RV. Calcium-sensing receptor (CaSR) mutations and disorders of calcium, electrolyte and water metabolism. Best Pract Res Clin Endocrinol Metab. 2013;27(3):359 371