Hypophosphatemic Rickets: Causes, Symptoms, and Treatment
Hypophosphatemic rickets is characterized by short stature, bone deformities, and tooth decay due to low serum phosphorus levels. This condition is linked to elevated FGF23 levels causing renal phosphate wasting. Clinical features include delayed walking, growth retardation, and bone abnormalities. Associated diseases under 40 years old include hemochromatosis, hyperparathyroidism, and hypophosphatasia. Radiographs show linear calcifications in joints. Treatment may involve pharmacologic therapy for pseudofractures and bone pain. Learn more about hypophosphatemic rickets and its management.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
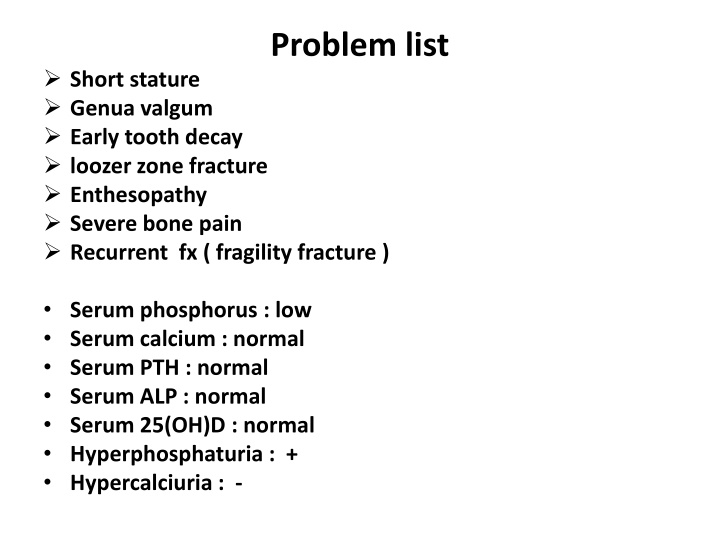
Problem list Short stature Genua valgum Early tooth decay loozer zone fracture Enthesopathy Severe bone pain Recurrent fx ( fragility fracture ) Serum phosphorus : low Serum calcium : normal Serum PTH : normal Serum ALP : normal Serum 25(OH)D : normal Hyperphosphaturia : + Hypercalciuria : -
Hypophosphatemic rickets (HR) Hypophosphatemia is due to elevated levels of FGF23 that result in renal phosphate wasting. J Pediatr Endocr Met 2015; 28(1-2): 211 216
Clinical features : Delay in walking in the first years of life Short stature Growth retardation Bone deformity (apparent after the age of 1 or 2 years) Femoral and tibia bowing, and genua vara and valga Females generally have less relevant bone involvement than males.
Diseases associated with CPPD under 40 yr old Disorder Probability of association Hemochromatosis Definite Hyperparathyroidism Definite Hypophosphatasia Definite Hypomagnesemia Definite Gitleman's syndrome Definite Hypothyroidism Probable Gout Possible X-linked hypophosphatemic rickets Possible Familial hypocalciuric hypercalcemia Possible Hemosiderosis Possible
CPPD Radiographs of the anterior-posterior views of right knees , the right shoulder and pelvis showing linear calcifications in the areas of the medial and lateral menisci of the knee, in the chondral cartilage of the proximal humerus and symphysis pubis and both hip joints respectively consistent with chondrocalcinosis (arrow).
Treatment The indicationsfor treatment of adult patients are more controversial. Affected adults are considered candidates for pharmacologic therapy: pseudofractures Bone pain, presumably due to osteomalacia After fractures or osteotomies Therapy is not recommended in asymptomatic patients who do not have pseudofractures. 2015
Treatment Once the decision is made to initiate therapy, it is best to start at a low dose of calcitriol and phosphate (to avoid diarrhea from phosphate) and gradually increase therapy over several months. Some clinicians maintain a highdose phase for up to 1 year: maximum calcitriol dose 25ng/kg/day Phosphate dose : 20 to 40 mg/kg four divided doses (up to a maximum of 2 g/day) . Serum calcium, phosphorus, and creatinine levels, urine calcium and creatinine, are routinely monitored on a monthly basis during dose escalation.
Treatment After 1 year on high-dose therapy, patients are switched to a long-term maintenance phase with 10 - 20 ng/kg/day of calcitriol and no change in the dose of phosphate. While patients are on maintenance therapy, we monitor serum and urine biochemistries at least every 3 to 4 months.
Treatment A 24-hour urine phosphorus measurement is often useful to gauge compliance with therapy. Serum PTH concentration should be measured at yearly intervals as appropriate.
Complications Diarrhea and gastrointestinal Nephrocalcinosis Tertiary hyperparathyroidism
Complications Factors that could influence the progression to tertiary hyperparathyroidism are an early age of treatment onset, longer duration of treatment, high doses of elementary phosphorus (100 mg/kg/day) and very high PTH plasma levels (around 400 pg/mL) .
Participants: Twenty-eight adults with XLH participated in a 4-month dose- escalation study (0.05 0.6 mg/kg); 22 entered a 12-month extension study (0.1 1 mg/kg). Intervention: KRN23 was injected sc every 28 days. Main Outcome Measure: The main outcome measure was the proportion of subjects attaining normal serum Pi and safety. Results: During dose escalation, TmP/GFR, Pi, and 1,25(OH)2D increased, peaking at 7 days for TmP/GFR and Pi and at 3 7 days for 1,25(OH)2D, remaining above (TmP/GFR, Pi) or near [1,25(OH)2D] pre-dose levels at trough. After each of the four escalating doses, peak Pi was between 2.5 and 4.5 mg/dL. Conclusions: Monthly KRN23 significantly increased serum Pi, TmP/GFR, and 1,25(OH)2D in all subjects.KRN23 has potential for effectively treating XLH.
