IAEA Series on Quality Management in Medical Radiological Practices
This content explores the importance of quality management in medical radiological practices, covering topics like roles and responsibilities, key performance indicators, drafting policies, and stakeholder involvement. It delves into understanding stakeholders, engaging with healthcare leadership, and strategies for ensuring quality and safety. The material highlights the involvement of patients, regulators, industry, and academia in healthcare quality and safety.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
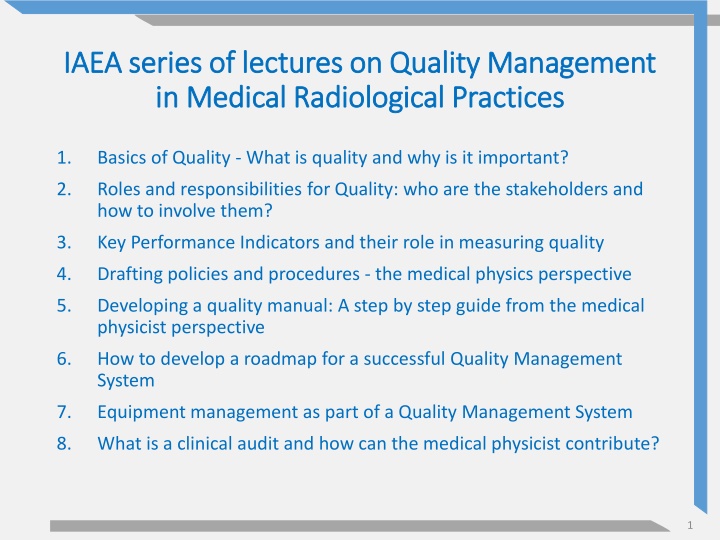
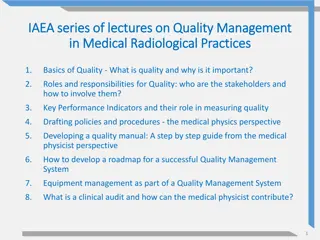
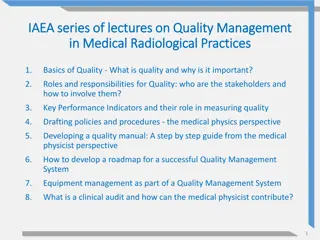
IAEA series of lectures on Quality Management IAEA series of lectures on Quality Management in Medical Radiological Practices in Medical Radiological Practices 1. Basics of Quality - What is quality and why is it important? 2. Roles and responsibilities for Quality: who are the stakeholders and how to involve them? 3. Key Performance Indicators and their role in measuring quality 4. Drafting policies and procedures - the medical physics perspective 5. Developing a quality manual: A step by step guide from the medical physicist perspective 6. How to develop a roadmap for a successful Quality Management System 7. Equipment management as part of a Quality Management System 8. What is a clinical audit and how can the medical physicist contribute? 1
Roles and responsibilities for quality : who are the stakeholders and how to involve them? Quality Management in Medical Radiological Practices (Diagnostic Radiology, Nuclear Medicine and Radiotherapy) 2
Objectives The objectives of this presentation are to: understand what responsibilities for quality within the hospital environment learn who are the stakeholders and how to involve them. are the roles and
Content Who are the external and internal stakeholders of quality and safety for medical radiological practices? What is the role of healthcare leadership in engaging with all stakeholders? What are the key strategies of involving stakeholders in quality and safety? 4
Stakeholder overview Quality and safety in healthcare involves a number of different stakeholders. On a large-scale level these are: Patients; Regulators and accreditation bodies; Industry and academia; Healthcare service. Each stakeholder has a different involvement and a different perspective of quality and safety. 5
Stakeholders: Large-scale level Healthcare service Industry and academia Quality and Safety Patients Regulators/ accreditation bodies 6
Patients Patients, including their families and caregivers, are the end recipients of the healthcare service. The quality and safety of the healthcare service directly impacts patients lives. Healthcare services are funded either directly or indirectly by patients. Online platforms enable patients to increase their awareness and to voice their opinions on healthcare services. hospital with user by Font Awesome Icons is licensed under CC BY 4.0 7
Patient engagement Patient engagement can be achieved by: Keeping them informed at every stage of their healthcare journey; Helping them understand the risks and managing their expectations; Involving them in decision making; Empowering them to ask and provide feedback. Patient engagement can be either on an individual level for a specific patient journey or on a community level by including patient focus groups and representatives. 8
Pause and Ponder How does your medical radiological practice collect patient feedback and how is it used? 9
Regulators and accreditation bodies Regulators set the quality and safety requirements for a healthcare service to be operational. Regulators can determine the allocation of central resources and can drive changes in legislation or in healthcare target prioritization. Regulators may also instigate improvements in clinical training and education or in the professional status of clinical craft groups. Healthcare accreditation and quality certification bodies may improve the visibility and peer status of a healthcare service provider, or may contribute additional resources, e.g. allow for private patients or research funding. 10
Engagement with regulator and accreditation bodies Regulators and accreditation bodies have vested interest in quality and safety. It is in the interest of the healthcare service to engage with regulator and accreditation bodies to help raise standards of quality and safety and provide feedback on their practical implementation. government by OSM Map Icons is licensed under CC0 1.0 11
Engagement with regulator and accreditation bodies The healthcare service must identify routes of engagement with them in the form of: Dialogue and feedback during inspections and audits; Communication from professional bodies (e.g. practice guidelines or position statements); Joint-interest conferences and working groups. handshake by Font Awesome Icons is licensed under CC BY 4.0 12
Pause and Ponder What regulators are involved in supervising your medical radiological practice? 13
Industry and academia Research and innovation from industry and academia can turn quality and safety concepts into clinical products. There can be improvements in the quality and safety of healthcare services on the basis of developments in: Equipment (e.g. CT scanners, personal protective equipment); Consumables (e.g. radionuclides for therapy or imaging); Informatics systems (e.g. picture display or treatment planning systems). Research also feeds into professional practice guidelines and initiates improvements of operational models. 14
Engagement with industry and academia The healthcare service should provide staff with protected time to engage in improvement projects on quality and safety as these can lead to research initiatives and grassroots innovations. Quality and safety should be highlighted as one of the key requirements and selection criteria for any products or services offered by industry. This will drive industry investment into quality and safety improvements. light bulb idea by Free Illustrations by Lukasz Adam is licensed under CC0 1.0 15
Engagement with industry and academia The healthcare service should collaborate with academia to ensure that the culture of quality and safety is embedded in academic curricula. New healthcare staff in-training (e.g. registrars and technologist students) should be immersed in a healthcare environment that equips them with the skills required to promote and engage with quality and safety. teach by Material Design Icons is licensed under Apache Licence 2.0 16
Pause and Ponder At your medical radiological practice, do all quality and safety stakeholders feed into the requirements for purchasing new equipment? 17
Healthcare leadership role External stakeholders (regulatory and accreditation bodies, patients, industry and academia) can incentivise and encourage healthcare leadership to engage with quality and safety. However, the success of the healthcare quality and safety framework will depend on leadership s commitment and culture. The starting point for healthcare leadership would be identifying the stakeholders of quality and safety for their medical radiological practice. 18
Healthcare stakeholders For a medical radiological service, stakeholders could be: Internal or external to the service; Clinical and non-clinical employees; Clinical staff of different disciplines; Staff at different organizational hierarchical levels. Quality and safety stakeholders can be identified on a granular level by looking at contributors at each step of the patient pathway. 19
Healthcare stakeholders Based on this, quality and safety stakeholders for medical radiological practices include: Referrers; Scheduling and registration team; Medical radiological physicians and practitioners; Related disciplines; Training and education specialists; Biomedical engineering and facility services; Healthcare Informatics team; Medical physicists. 20
Referrers Referrers may range from outpatient general practitioners to inpatient physicians of different disciplines, for example the departments of emergency, surgery, orthopaedics, obstetrics, speech therapy or cardiology. surgery by Medical Icon Set is licensed under MIT License 21
Referrers Referrers will input on a number of important issues regarding the patient journey, for example: Are waiting times for appointments appropriate for the types of exams or therapies requested? Are referral guidelines accessible and clear? Do report turnaround times and communication of critical findings meet the clinical need? Do images and reports relay the level of information required? 22
Pause and Ponder Who are the referrers for your medical radiological practice? 23
Scheduling and registration team Involving the scheduling and registration team can help address important issues of quality and safety, for example: Can appointment slots be used more efficiently and less disruptively for patients and staff? Are orders placed by referrers clear to action? Is the primary patient identification process effective? Are patient instructions and information on the exam or therapy readily available? registration by Medical Icon Set is licensed under MIT License 24
Scheduling and registration team Another important reason for including the scheduling and registration team is that in many cases it acts as the primary contact point for the majority of external stakeholders In this way, it may likely be the main recipient of feedback for the medical radiological service. feedback by Codicons is licensed under CC BY 4.0 25
Medical radiological practitioners Medical radiological practitioners include: Radiologists; Nuclear medicine physicians; Radiation oncologists. Radiological physicians are responsible for the justification of radiological exposures and are therefore key stakeholders of medical radiological quality and safety. People team by Fluent UI System Icons is licensed under MIT License 26
Medical radiation technologists Medical radiation technologists are staff planning and performing radiological exposures and are typically also technologists or technicians, for example: Radiographers; Nuclear medicine technologists; Radiation therapists. Medical radiation technologists are also primary stakeholders of medical radiological quality and safety. 27
Related disciplines Depending on their scope, medical radiological practices require the support of other disciplines, for example: Radiopharmacy; Nursing; Anaesthesiology; Pathology and pharmacy; Child life / play therapy. When appropriate, leadership should include representatives of these teams as stakeholders contributing to the quality and safety framework. 28
Related disciplines example 1 The child life specialist / play therapist can recommend ways that children can be more cooperative during an examination. This will improve patient experience and feedback but can also reduce safety risks coming from repeating or prolonging exams due to uncooperative patients. teddy bear by OpenMoji Emoji Set is licensed under CC BY 4.0 29
Related disciplines example 2 The anaesthesiologist can recommend workflow improvements to allow for early pre-operative alerts when a patient is found pregnant and there is planned use of radiological imaging. This will allow the radiology team to consent the patient and take any precautions required to maximize protection of the foetus. pregnant by Medical Icon Set is licensed under MIT License 30
Related disciplines example 3 The radiopharmacist can recommend ways to make the preparation of radiopharmaceuticals more efficient and reliable, for example by their feedback on supplier reliability or radiopharmacy storage and equipment improvements. This will ensure that the results and diagnoses of nuclear medicine studies are not compromised by the quality of radiopharmaceutical preparation. woman scientist by OpenMoji Emoji Set is licensed under CC BY 4.0 31
Pause and Ponder What are the related disciplines for your medical radiological practice? 32
Training and education specialists Training and education is an integral part of quality and safety. Clinical and non-clinical staff need to develop and maintain the knowledge, skills and competencies required to apply themselves to their roles and responsibilities in quality and safety. Quality and safety should involve departmental, organizational or external staff responsible for developing, delivering or overseeing training and education. 33
Biomedical engineering and facility services Staff responsible for the equipment, consumables and environment of medical radiological practices are also stakeholders of quality and safety. These may include: Internal or external biomedical engineers; Housekeeping and porters; Security and emergency response teams; Facility maintenance teams; Purchasing and supply teams. 34
Biomedical engineering and facility services example Facility maintenance and security teams can provide feedback on how to physically restrict access to radiation- controlled areas. This can ensure safety to staff and patients and can also reduce relying on administrative controls. stop sign by OpenMoji Emoji Set is licensed under CC BY 4.0 35
Healthcare informatics team Medical radiological practices rely on a number of informatics tools such as: Referral clinical support tools; Ordering and scheduling software; Radiology information systems; Image display, reporting and archiving systems; Advanced analysis and post processing workstations; Therapy planning and dosimetry software. 36
Healthcare informatics team The role of the healthcare informatics team in quality and safety is to ensure that medical informatics tools are seamlessly available and maintained/updated appropriately. The healthcare informatics team can also support automated extraction of quality and performance metrics e.g. report turnaround times. 37
Medical physicist The medical physicist is a key stakeholder of quality and safety in medical radiological practices. The role of the medical physicist involves quality and safety activities related to patient care, such as developing and implementing a quality assurance plan for radiological equipment, patient dosimetry evaluations and clinical audits. The medical physicist is responsible for overseeing and advising on radiation safety of personnel and public. The medical physicist also plays an important role in teaching and training programs on radiation safety and dose optimization. EUROPEAN COMMISSION, FOOD AND AGRICULTURE ORGANIZATION OF THE UNITED NATIONS, INTERNATIONAL ATOMIC ENERGY AGENCY, INTERNATIONAL LABOUR ORGANIZATION, OECD NUCLEAR ENERGY AGENCY, PAN AMERICAN HEALTH ORGANIZATION, UNITED NATIONS ENVIRONMENT PROGRAMME, WORLD HEALTH ORGANIZATION, RADIATION PROTECTION AND SAFETY OF RADIATION SOURCES: International Basic Safety Standards: General Safety Requirements Part 3, No. GSR Part 3, IAEA, Vienna, 2014. INTERNATIONAL ATOMIC ENERGY AGENCY, Roles and Responsibilities, and Education and Training Requirements for Clinically Qualified Medical Physicists, Human Health Series, IAEA, Vienna, 2013. 38
Pause and Ponder How can the medical physicist of your medical radiological practice contribute to both safety and quality? 39
Quality is everybodys job, but because it is everybody s job, it can become nobody s job without the proper leadership and organization Armand Feigenbaum 40
Engagement strategies The leadership of medical radiological practices must engage with all stakeholders by highlighting the importance of connecting around a common purpose: Quality and safety should be communicated as an interesting and relevant area for all stakeholders; Quality and safety goals should be mutually defined and developed; Stakeholders should be given a voice around the discussion and decision table. 41
Engagement strategies In addition, leadership and stakeholders should engage in a meaningful interaction and dialog: Communication should be continuous and seen as a two-way contribution rather than a top-down information push; All stakeholders should be included early in decision processes; Interactions between leadership and stakeholders should be sincere and transparent. 42
Healthcare leadership culture The culture of healthcare leadership will play a pivotal role in enabling and encouraging stakeholders to engage with quality and safety. By instilling a just and open working culture, leadership can empower staff to proactively monitor their own workplace and participate in quality and safety efforts within their work environment. Holding staff responsible and accountable for quality and safety will also foster innovation and improve communication within and across disciplines and hierarchies. 43
Pause and Ponder Is quality and safety mentioned as a responsibility in all job descriptions at your medical radiological practice? 44
Healthcare leadership role Leadership is responsible for laying the foundations of the quality and safety framework and enabling it to establish and grow. This would include: Formalizing the framework with an appropriate quality management system; Expecting quality and safety as performance outcomes for all staff and valuing individuals contributions; Providing financial and administrative resources to support the framework; Leading by example: adopting quality and safety as a key decision and management driver. 45
Quality and safety management team The engagement of stakeholders should be formalized by establishing a quality and safety management team. The management team should have representation or input from all quality and safety stakeholders. It is important that leadership empowers stakeholders to speak up across hierarchical gradients. The quality and safety management team should be provided with the resources and tools allowing it to make decisions and take meaningful action. 46
Quality and safety management team The quality and safety management team should not be seen as generating rules reactively and in a hierarchical manner. Instead, the role of the quality and safety management team should be incorporated in clinical operations, as a natural component of evolving clinical practice. collaboration by OpenMoji Emoji Set is licensed under CC BY 4.0 47
Hierarchical model Leadership Quality and Safety management team Policies Dictums Isolated bad event or complaint Clinical team 48
Collaborative model Leadership Quality and Safety management team Supports and celebrates quality and safety initiatives Nurtures culture of safety Empowers others to improve process Data from continuous monitoring of process measurements Integrating facilitators of quality/safety into routine workflow (e.g. peer review, checklists, standardization, learn assessments) Clinical team 49
Pause and Ponder How many safety and quality issues have been raised by junior staff at your medical radiological practice? Is this number proportional to their contribution to the patient journey? 50