Idiopathic Central Precocious Puberty in Children
Learn about the diagnosis and evaluation of idiopathic central precocious puberty in a 5-year-old girl presenting with early breast and pubic hair development. Understand the differences between true precocious puberty, premature adrenarche, and premature thelarche, along with delayed puberty conditions. Explore the importance of bone age assessments and the next steps in evaluating early puberty signs in children.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Precocious puberty A case D ra T r k MD, PhD
Parents bring their 5-year-old daughter to your clinic because she has developed breast and pubic hair over the past 3 months. Physical examination reveals a girl whose height and weight are above the 95th percentile, Tanner stage II breast and pubic hair development, oily skin, and facial acne.
Parents bring their 5-year-old daughter to your clinic because she has developed breast and pubic hair over the past 3 months. Physical examination reveals a girl whose height and weight are above the 95th percentile, Tanner stage II breast and pubic hair development, oily skin, and facial acne. * What is the most likely diagnosis? * What is the best next step in the evaluation?
* Most likely diagnosis: Idiopathic central precocious puberty. * Next step in the evaluation: Inquire about birth history, illnesses, hospitalizations, medications, siblings health status, and family history of early puberty and diseases. Serum follicle-stimulating hormone (FSH) and luteinizing hormone (LH) levels and bone age radiographs are helpful.
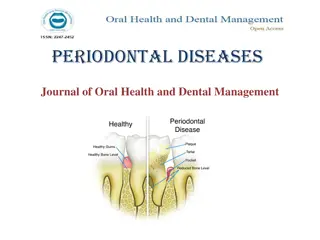
DELAYED PUBERTY: No signs of puberty in girls by age 13 years or in boys by age 14 years. May be caused by gonadal failure, chromosomal abnormalities (Turner syndrome, Klinefelter syndrome), hypopituitarism, chronic disease, or malnutrition. CLINICAL CASES 249 PRECOCIOUS PUBERTY: Secondary sexual characteristic onset before age 8 years in girls and 9 years in boys. Children in different ethnic groups undergo puberty differently; African-American girls often do so earlier than Caucasian girls. TRUE (CENTRAL) PRECOCIOUS PUBERTY: Gonadotropin-dependent. Hypothalamic-pituitary-gonadal activation leading to secondary sex characteristics. PRECOCIOUS PSEUDOPUBERTY: Gonadotropin-independent. No hypothalamic-pituitary-gonadal activation. Hormones usually are either exogenous (birth control pills, estrogen creams) or from adrenal/ovarian tumors. PREMATURE ADRENARCHE: Early activation of adrenal androgens (typically in girls ages 6 to 8 years), with gradually increasing pubic/axillary hair development and body odor. PREMATURE THELARCHE: Early breast development (typically in girls ages 1 to 4 years), without pubic/axillary hair development or linear growth acceleration.
More common in girls, true precocious puberty stems from secretion of hypothalamic GnRH with normal-appearing, but early, progression of pubertal events. Sexual precocity is idiopathic in more than 90% of girls, whereas a structural CNS abnormality is present in 25% to 75% of boys.
GnRH stimulation LH peak in puberty (3-10x) FSH peak in prepuberty (3-5x) Therapy: monthly GnRH Depot injection