Immediate vs. Deferred Surgery for Symptomatic Epiretinal Membranes
This randomized trial protocol aims to compare the outcomes of immediate versus deferred surgery for symptomatic epiretinal membranes, evaluating visual acuity, visual function, OCT outcomes, and complication rates over 36 months.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Randomized Trial Comparing Immediate vs Deferred Surgery for Symptomatic Epiretinal Membranes (Protocol AM) Protocol Chairs: Darrell Baskin & Mathew MacCumber
Background Although vitrectomy with ERM peeling has a high success rate, some patients experience less than optimal VA improvement Patients with significant macular changes on OCT but relatively good vision are often advised to defer surgery until vision declines to 20/40 or worse It is unknown whether delaying surgery, which allows the foveal architecture to remain compromised and potentially to deteriorate, results in worse VA outcomes than if surgery is performed earlier There is a need to better understand predictors of outcomes when surgery is performed and predictors of progression when surgery is deferred 2
Study Objectives Primary Compare visual acuity outcomes at 36 months between eyes randomized to immediate versus deferred surgery Secondary - between group comparisons Compare changes in visual function (using M-CHARTS), reading speed (using MNREAD), and OCT outcomes from randomization at 36 months between eyes randomized to immediate versus deferred surgery Compare complication rates between eyes randomized to immediate versus deferred surgery 3
Study Objectives Secondary - within group comparisons Determine the rate of and time to progression of ERM to needing vitrectomy in eyes randomized to deferred surgery Determine if there are baseline or later variables (such as performance of cataract surgery or OCT findings) that predict ERM progression to needing vitrectomy in eyes randomized to deferred surgery 4
Study Objectives Other objectives Explore associations between participant factors and retinal anatomy with outcomes Assess how often lens removal is needed after phakic vitrectomy (among eyes receiving surgery during study) Collect natural history data for deferred surgery eyes Assess whether fundus autofluorescence (FAF) images are of value in assessing progression of ERM or improvement in macular anatomy after ERM removal (as part of an ancillary study among sites with machine capabilities) 5
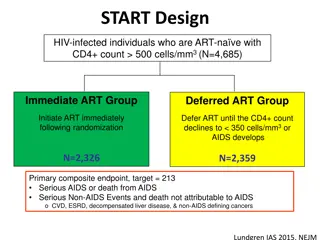
Study Design Multi-Center Randomized Clinical Trial (400 Eyes) At least 1 eye meeting all the following criteria E-ETDRS visual acuity 20/40 or better ( 69 letters) ERM must be thought to be the primary cause of vision loss ERM meeting the following criteria (no RC confirmation required) ERM is not secondary to another condition Symptoms of visual loss and/or distortion (and in the opinion of the investigator, the ERM is contributing to the participant s symptoms); either new or worsening in the past 24 months Epiretinal membrane involving or altering the central 3 mm of the macula on OCT Distortion within the central subfield by ERM on OCT Deferred Surgery (vitrectomy only if protocol criteria met) Immediate Surgery (within 4 weeks) Primary Outcome: Mean change in visual acuity letter score from baseline to 36 months 6
Major Patient Eligibility Criteria Age 45 years Blood pressure 160 systolic and 100 diastolic No known condition that, in the opinion of the investigator, would preclude participation in the study (e.g. unstable medical status that might preclude completion of follow-up) Immediate vitrectomy not required (investigator and participant are willing to wait at least 4 weeks to see if vision remains stable without having to proceed to vitrectomy) 7
Important Reminders The participant must be willing to accept the randomization assignment We do not want participants requesting surgery when they find out they are in the deferred group Participants should be comfortable with their level of visual function at baseline and should be willing to wait for surgery until vision or symptoms worsens 8
Major Exclusion Criteria History of retinal vascular disease History of vitreous hemorrhage if vitreous hemorrhage is thought to have caused the ERM History of vitreous hemorrhage is permitted provided the vitreous hemorrhage did not cause the ERM in the investigator s opinion History of inflammatory disease unless mild and completely resolved at least one year prior to randomization 9
Major Exclusion Criteria History of DME, RVO, or uveitis (except mild uveitis that resolved >1 year prior to randomization) Prior intraocular surgery (except uncomplicated cataract extraction) Cataract extraction within prior 3 months Laser or cryosurgical retinopexy within one month of randomization Current untreated retinal tear or detachment A previously treated retinal tear with up to one disc diameter radius of subretinal fluid is permitted 10
Major Exclusion Criteria Macular hole Degenerative lamellar macular hole ERM foveoschisis ( tractional lamellar hole) is permitted Vitreomacular traction within 1,500 microns of foveal center Central serous chorioretinopathy Nonproliferative diabetic retinopathy or worse (DR severity >20) 11
Schematic of Study Design Enrollment visit and Randomization Immediate Surgery Group Deferred Surgery Group Vitrectomy (within 1 month of randomization) Follow-up visits at 3, 6, 12, 18, 24, 30 (phone call), and 36 months post- randomization. Vitrectomy may be performed during follow-up if protocol criteria is met. Eyes receiving vitrectomy during study will complete a 1-month post- vitrectomy visit Follow-up visits at 1-month post- vitrectomy and 3, 6, 12, 18, 24, 30 (phone call) and 36 months post- randomization 12
Study Visits and Procedures Baseline Testing and Randomization* X 1-month post- vitrectomy visit a X 3, 6, 12, 18, 24, 36 months b X 30-month phone call b Pre-Vitrectomy Visit c X E-ETDRS BCVA in both eyes X X X X Eye exam in both eyes X X X X SD-OCTin study eye Visual function testing in study eye (M-CHARTS) Reading Speed in study eye (MNREAD) Blood Pressure X X X X X X X FAF in study eye (if site has Spectralis machine) Solicitation of vision changes and safety events *All baseline testing procedures must be completed within 21 days prior to randomization. a = Based on date of vitrectomy (applies to immediate surgery group eyes and eyes in deferred surgery group that receive vitrectomy during follow-up). b = Visit schedule is based on date of randomization. c = A pre-vitrectomy visit is an unscheduled visit for a participant in the deferred surgery group at which the decision to proceed to surgery is made X X X X 13
Criteria for Vitrectomy Vitrectomy may occur during follow-up for eyes in the deferred surgery group if one of the following criteria are met: 1. Decrease in E-ETDRS VA 10 letters from baseline at a single visit presumed to be from ERM 2. Decrease in E-ETDRS VA 5 letters from baseline at two consecutive visits (at least 1 month apart) presumed to be from ERM 3. Participant actively requests surgery due to worsening symptoms 4. Complication requires prompt surgical intervention (e.g. macular hole, retinal detachment) 14
Vitrectomy Procedures Vitrectomy will be performed according to the investigator s standard practice Investigators may use staining agents and peel the ILM if they typically do as part of their standard vitrectomy practice Combined cataract surgery is also permitted Details on the vitrectomy procedure will be collected on the Vitrectomy Form 15
Thank You 16