Immunosuppressive Strategies and Infectious Risk in Hematopoietic Stem Cell Transplantation
This presentation discusses various immunosuppressive strategies and their impact on infectious risks in hematopoietic stem cell transplantation, presented by Andrea Bacigalupo from Fondazione Policlinico Universitario Gemelli. Topics covered include cyclosporin A, methotrexate, post-transplant cyclophosphamide, acute GvHD rates over different transplant years, GvHD prophylaxis approaches, and instances of bloodstream infections pre-engraftment. The slides examine tolerance mechanisms, patient outcomes, and prophylactic measures implemented from 2000 to 2018.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Immunosuppressive strategies and infectious risk in hematopoietic stem cell transplantation Andrea Bacigalupo Istituto di Ematologia Fondazione Policlinico Universitario Gemelli IRCCS Universita Cattolica del Sacro Cuore Roma Varese, 23 maggio 2019
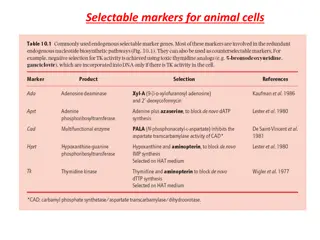
Cyclosporin A MTX PTCY CyA+MTX CyA + MMF FK+ Sirolimus TCD ex vivo ex vivoCD34 sel / CD19 dep T CD in vivo (ATG /CAMP) 1970 1980 1990 2000 2010 2017
Post-transplant CY: Three distinct and sequential mechanisms for induction and maintenance of tolerance 3 Intrathymic clonal deletion of donor-derived anti host T cells 1 1 anti-host and anti-donor T cells are destroyed in the periphery 2 development of peripheral tolerance Luznik, 2012
All patients and year of transplant: acute GvHD II P<0.000001 <2000, n=1062 40% 2001-2010, n=840 20% 12% >2010, n=914
All patients and year of transplant: acute GvHD III-IV P<0.000001 <2000, n=1238 13% 2001-2010, n=927 >2010, n=961 5% 4%
GvHD prophylaxis 2000-2018 HLA id.sibs UD 8/8 CB (4/6 5/6) HAPLO CyA MTX CyA MTX ATG 5 CyA MTX ATG 5 CyA MMF PT-CY
Pre-engr BSI G+ 19% 15% G- F N=166 (30%) at least 1 BSI Median int from SCT 8 days Year 2010-2012 =29% Year 2013-2016 =31% 18% 14% 20% 16% HLA id SIB UD CB HAPLO 7% 7% 26% 11% 26% 19% 4% 16%
Pre-engr BSI: 7 and 30 day mortality 7d 30d N=166 at least 1 BSI G+ G- Coli (4) Klebsiella (6) Pseudomonas (3) Multiple only G+ (8) G+G- (19) 5% 0% 6% 2% 33% 50% 33% 67% 8% 1% 11% 4% 0% 21% 26% 1%
Pre-engr BSI: Factors predicting IR mortal NRM D 60 BSI Etiology Engraftm Year YES G- no >2012 (2.5%) G-
1. Pre-engraftment infections # predicted by donor type HLA mismatch and/or GvHD proph ? # negative impact on 60-day NRM # caused mainly by carbapenem resistant Gram- pathogens, # particular attention should be given to appropriate empiric therapy and management of patients at high risk for Gram-negative BSI.
Post engraftment infections CMV EBV Aspergillus Bacteria
GvHD prophylaxis HLA id.sibs UD 8/8 CB (4/6 5/6) HAPLO CyA MTX CyA MTX ATG 5 CyA MTX ATG 5 CyA MMF PT-CY
CD4 recovery after HSCT median counts CsA+MTX CsA+MMF+PTCY CsA+MTX+ATG CsA+MTX+ATG
Chronic GvHD (moderate-severe) P= 0.02 Acute GvHD (grade II-IV) P= 0.003 SIBS ; 29% UD; 31% SIBS ; 31% UD; 21% UCB; 21% UCB; 19% HAPLO; 14% HAPLO; 14% 1,000 CMV infection Transplant Related Mortality P= 0.007 UD; 76% HAPLO; 75% 0,750 Cumulative Incidence UCB; 74% SIBS; 55% 0,500 UCB; 34% UD; 34% SIB ; 19% 0,250 HAPLO; 17% P< 0.001 0,000 Fig.2 0,0 300,0 600,0 900,0 1200,0 days from transplant
CMV infection after engraftment # higher risk with HLA mm donors And treatment?
Cumulative incidence of CMV response P=0.01 84% HAPLO and PT-CY, n=67 59% UD and ATG, n=30
Actuarial survival HAPLO and PT-CY, n=67 71% 51% UD and ATG, n=30 P=0.02
Rituximab 200 mg fixed dose Day +5
Infections: donor type/ diagnosis / ATG/ HLA mm / GvHD prophylaxis/ CD4 recovery Complex interplay
Infections related death and year of transplant N= 3126 allografted patients 10% 12% 7% AGE 32yy 42yy 52yy Alt Don 22% 51% 78% <2000 2000-2010 2011-2018 P=0.001
Infections related death and year of transplant N= 3126 allografted patients 10% 12% 7% AGE 32yy 42yy 52yy Alt Don 22% 51% 78% (PTCY 65%) <2000 2000-2010 2011-2018 P=0.001
Non Infection related death and year of transplant N= 3126 allografted patients <2000 2000-2010 2011-2018 44% 45% 38% P<0.00001
Non Infection related death and year of transplant N= 3126 allografted patients (ge-gem) <2000 2000-2010 (n=927) 2011-2018 (n=963) (n=1236) 45% 42% 54% P<0.00001
Conclusions # Better GvHD prophylaxis # Better CD4 recovery with PT-CY as compared to ATG # Improved survival What now?
GvHD proplylaxis 2019 CyA MMF PT-CY CyA MMF PT-CY CyA MMF PT-CY CyA MMF PT-CY <=2018 CyA MTX CyA MTX ATG 5 CyA MTX ATG 5 CyA MMF PT-CY HLA id.sibs UD 8/8 CB (4/6 5/6) HAPLO
Genova BMT Unit E Angelucci AM Raiola, F Gualandi, A Dominietto, R Varaldo, M T Van Lint , S Bregante, C di Grazia T Lamparelli Gemelli BMT Unit S Sica, L Laurenti, P Chiusolo, F sora , S Giammarco, E Metafuni, I Innocenti, F Autore A DiGiovanni E Alma ID Unit GE C Viscoli M Mikulska V del Bono Gemelli ID Unit R Cauda M Tumbarello Microbiology M Sanguinetti Commissione Infezioni Corrado Girmenia Data Manager R Oneto G Conti M Daneri Nursing team