Impact of Care Coordination Across Providers
The Middlesex County Community Care Team focuses on building communities of care with various agency members to provide comprehensive services to patients. They track and measure impact metrics such as demographics, care planning, and patient distribution among different racial and gender categories.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
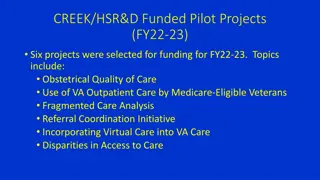
Middlesex County Community Care Team: The Impact of Care Coordination Across Providers Mobile Integrated Health Work Group November 7, 2017 Presented by Jim Santacroce, Emergency Medical Services Middlesex Hospital 1
Middlesex County CCT Agency Members Building Communities of Care as Partners in Practice Middlesex Hospital River Valley Services Connecticut Valley Hospital (Merritt Hall) Rushford Center, Inc. The Connection, Inc. St. Vincent de Paul Soup Kitchen Mercy Housing Columbus House Chrysalis Center, Inc. Community Health Center Gilead Community Services, Inc. Advanced Behavioral Health Beacon Health Options, Connecticut Community Health Network Mdsx County Community BH & Social Services Mdsx Hospital CCT Patients Case/care management agencies 2
Middlesex County CCT Process Step 3 Added to CCT Agenda: Once ROI is signed, patient is added to CCT agenda and hospital visit history is developed Patients are only removed from agenda due to 1) moving out of area/state or 2) death Step 1 - Patient Identification: ED visit threshold (# of visits & behavioral diagnoses) Daily ED discharge reports (5+ visits in 6 months) Chair of Emergency Services dictates ED Care Plan for ROI to be signed Health Promotion Advocate referral CCT member referral 5 Step 5 Follow-Up: Continued follow-up on after-care plans Rapid team intervention when exacerbation of illness occurs after a period of stabilization 4 Step 4 Weekly Meetings: Team meets on a weekly basis to discuss & care manage new/on-going patients 3 2 Step 2 - Patient Interaction with Hospital HPA: Relationship building with patient Referrals to treatment; on-going follow-up Assists with completion of Universal Housing Applications 1 3
What We Track & Measure Impact Metrics: Demographics: # of visits (ED & inpatient) pre- and post- intervention (snapshot in time) Cost/losses # of patients who have received care planning Diagnosis category Gender Race/Ethnicity Age distribution Insurance status Housing status # of patients who have received CCT care planning to-date: 334 4
What We Track & Measure Race/Ethnicity Gender 84% 100% 100% 80% 62% 80% 60% 60% 37% 40% 40% 12% 3% 1% 20% 20% 1% 0% 0% Caucasian African American Hispanic Asian Male Female Transgender 5
What We Track & Measure Age Distribution Payer 50% 100% 35% 40% 80% 60% 60% 30% 23% 35% 18% 40% 20% 14% 20% 3% 7% 2% 10% 2% 1% 0% 0% Medicaid Medicare Managed Care Self-pay no insurance 20-29 30-39 40-49 50-59 60-69 70-79 80-89 6
What We Track & Measure Diagnoses Chronic Mental Illness Dual Diagnosis Chronic Alcoholism Other Drug Dependence Most frequent dxs: bipolar; schizophrenia; schizoaffective; borderline personality Coexisting severe mental illness and substance abuse disorders (primarily alcohol) alcohol intoxication with/without suicidal ideation Opioids; cocaine with/without suicidal ideation 41% 31% 25% 3% In addition to behavioral health dxs, CCT patients oftentimes experience significant and complex medical conditions Dual: alcohol only 60% Dual: other drugs 33% Dual: alcohol & other drugs 7% - - - 7
What We Track & Measure 12% 12% 10% 8% 8% 5% 6% 4% 1% 2% 0% Homeless Permanent Supportive Housing Unstable Housing Incarcerated What we ve learned about housing status: Housing is an issue Stable housing is linked to better health outcomes, improved quality of life and reduced ED utilization It is critical to involve community partners who work with the homeless/marginally housed (St. Vincent de Paul, Mercy Housing, The Connection, Columbus House, Chrysalis Center) 8
Additional Benefits Patient Improved Quality of Life Mdsx County CCT Collaborative Patient Linkages to Care/Support Society Primary care physicians, psychiatrists, specialists, etc. Supportive housing Appropriate outpatient services Improved patient care Improved agency- specific care plans Improved inter-agency communication and relationships Sobriety Mental health stabilization Reduced homelessness Re-entry to workforce Re-connection with family Achievement of feelings of self-worth and respect Increase in safety to all Reduction in Medicaid & Medicare expense 9
What Have We Learned? 1) The CCT target population does not get better with the traditional model of care delivery 2) Behavioral health chronic diseases require care coordination and customized treatment plans 3) Individualized care plans must have the ability to be flexible and evolve Many agency providers were unaware of frequency of ED visits communication allows for agency-specific care plans (a major part of CCT s success) 4) 5) We have an effective system in place to identify those CCT patients who would have better health outcomes when provided supportive housing 6) The integration of the housing and medical communities is critical for addressing the social and medical needs of a shared population 10
Questions? Thank You! Jim Santacroce, Manager Emergency Medical Services Middlesex Hospital 28 Crescent Street Middletown, CT 06457 jim.santacroce@midhosp.org 11