Impact of HIV on Key and Vulnerable Populations
Explore the implications of the HIV pandemic, focusing on most-at-risk and vulnerable populations, UNAIDS targets, stigma, and discrimination. Learn about key populations like injecting drug users and female sex workers, as well as vulnerable groups such as young people and migrants.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Implications of the HIV pandemic Dr Hany Ziady Professor of Public Health Alexandria Faculty of Medicine 2022
Dr Hany Ziady Professor of Public Health Alexandria Faculty of Medicine ziadyhany@gmail.com
Learning objectives 1- to know that is meant by most-at-risk and vulnerable populations and their importance in HIV response. 2- to be oriented about approaches and services used in relation to HIV at-risk populations. 3- to understand the UNAIDS targets for ending the AIDS epidemic. 4- to be aware about the situation of at-risk populations in Egypt. 5- to know what is HIV stigma and discrimination, their causes and effects.
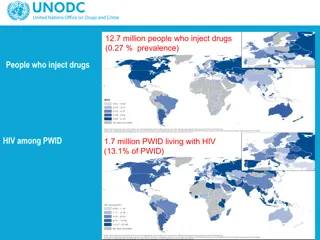
Most-at-risk populations In 2016, outside of sub-Saharan Africa, key populations and their sexual partners accounted for 80% of new HIV infections. Even in sub-Saharan Africa, key populations accounted for 25% of new HIV infections in 2016
Most-at-risk populations These are people who are particularly at-risk to HIV and frequently lack adequate access. They are at increased risk of acquiring the HIV infection because their practices are associated with a high risk of HIV transmission. Examples of those population groups are injecting drug users (IDU), female sex workers men who have sex with men.
Vulnerable populations People are said to be in a state of vulnerability if their living conditions would place them at risk of contracting HIV. Examples of those groups are young people, women, migrants, long-distance drivers, displaced populations, men in uniform and others.
The heightened by the transmission of the virus among populations with high- risk behavior, and then propagating to the general populations via so-called bridging groups, depending on the extent and nature of social linkages and networks populations. Evidence has shown that expanding awareness, prevention and behavior change interventions populations at increased risk of HIV can slow or even curb the epidemic. HIV epidemic is usually Importance of working with vulnerable groups and key populations at increased risk of HIV between these among key
Bridging populations may include Partners/clients of female sex workers Migrant workers Truck drivers and others Importance of working with vulnerable groups and key populations at increased risk of HIV Bridging vulnerable groups may differ from one country or community to another populations as well as
Importance of working with vulnerable groups and key populations at increased risk of HIV
Moreover, in low level and concentrated epidemics populations at increased risk of appropriate services can be more efficient identifying PLHIV and thus, can provide an entry point for PLHIV to access care, treatment and support. HIV key reaching Importance of working with vulnerable groups and key populations at increased risk of HIV HIV with in
Programmes designed to address vulnerable groups and key populations at increased risk of HIV should ensure a friendly environment to allow the access of those groups to the service. Population-friendly environment entails a non-judgmental attitude provided within a non-stigmatizing service understanding service providers. It also entails ensuring geographical, financial and procedural accessibility. However these approaches differ between different communities and cultures. In some communities these approaches are very supportive and guide these key populations to how to continue their practices with minimum risks. In other communities however, where there are more stigma and punitive laws approaches are weaker, however they exist and mostly depend on NGOs working with the key populations. In this latter settings, the range of services provided is narrower. Approaches to working with facility, by capable and vulnerable groups and key populations at increased risk of HIV targeting them, the
Peer involvement: Peers are the ones who understand most the needs of their fellows. Interaction facilitated by the sense of belonging to the group and by breaking the barriers of misunderstanding, intimidation . In addition, peers can play the role of models for each other. Outreach: Individuals may not seek certain services for various reasons. These reasons can be personal (e.g. level of awareness, perceptions, trust, (taboo, stigma), geographical, etc. vulnerable groups and key populations at increased risk of HIV can help transcending those barriers. between them is Approaches to working with vulnerable groups and key populations at increased risk of mistrust and etc.), legal, Outreaching socio-cultural financial, HIV to
Low Complicated admission procedures and paper work may pose a barrier particularly to risk and vulnerable groups. Low minimizing the administrative requirements for attending to the needs of the service users. Basing those facilities within the communities can improve geographic access and ensure community support. Self help and support groups: Belonging to a group where members share similar life conditions and problems provides the assurance that one is not alone. Collective thinking and problem solving in the group empowers individuals through having an insight to how others managed their situations. In addition, it helps the group to find solutions suitable for their collective situation. threshold community-based facilities: Approaches to working with vulnerable groups and threshold and regulatory means key populations at increased risk of HIV (cont.)
Awareness raising and behavior change communication Counseling and Testing Supply of prevention material such as condoms and sterile injection equipment Substitution and maintenance therapy for opiate drug users STI diagnosis and management Prevention, diagnosis and management of opportunistic and common co-infections such as TB, Hepatitis B and Hepatitis C Care, treatment and support for PLWHA and their families Prevention of mother to child transmission Referral for secondary and tertiary health care needs and for other types of services as needed Services provided to key populations at increased risk of HIV
Special NGOs that work with the special groups to achieve equality in the society, encourage their well being and promote their safety, through providing services, knowledge and support. Sex guides PEP HIV testing Investigations National HIV testing week, i.e. largely offering HIV testing during a certain week usually before the World AIDS Day on the 1stof December every year, in a way similar to National Immunization Days Examples of services offered to most-at-risk populations in Western countries
Prevention options: condoms, PEP, PreP PreP: used by HIV negative, in UK can be bought online. Doses depend on the type of practice e.g. IDU. Type of sexual relations, etc. Dose is usually daily but the person needs to have a confirmation that he/she is HIV negative. PEP: after unsafe sex with higher risk exposures, Safer sex packs: condoms, water-based lube, information on PreP, PEP, U=U, testing, condom use, sexual health guides and online support. Examples of services offered to most-at-risk populations in Western countries
Working with vulnerable groups and key populations at increased risk of HIV in the EM Region Over time, several countries in the Eastern Mediterranean Region have developed successful experiences in addressing vulnerable groups and key populations at increased risk of HIV. Services provided in various countries include outreach education awareness raising, syringe distribution, condom distribution, HIV testing and counselling, opioid substitution therapy, and others. The comprehensiveness of the services and their level of coverage, however, remain a great concern.
Key populations may slightly differ between countries and in different cultures According to CDC in USA for example While all Americans are affected by the HIV epidemic, some populations bear an especially heavy burden and account for the largest numbers of HIV infections. Success in HIV prevention can only be achieved by addressing these disparities and working to achieve health equity. Hard-hit populations include: Gay and bisexual men of all races and ethnicities remain the group most severely and disproportionately affected by the epidemic. Men who have sex with men (MSM*) represent approximately population, but accounted for 61 percent** of all new HIV infections in 2009. By race, age and risk group, young, black gay and bisexual men (ages 13-29) are the only population in the United States in which new HIV infections increased between 2006 and 2009. African Americans are by far the most affected racial/ethnic population in the United States. African Americans represent 14 percent of the U.S. population, but accounted for 44 percent of new HIV infections in 2009. The HIV infection rate among African Americans was almost eight times as high as that of whites in 2009, and among African American women it was 15 times higher than among white women.7 2 percent of the U.S.
Key populations may slightly differ between countries and in different cultures Latinos affected approximately 16 percent of the total U.S. population, but accounting for 20 percent of all new HIV infections. In 2009, the HIV infection rate among Latinos was three times as high as that of whites. Injection drug users (IDUs) represented 9 percent of new HIV infections in 2009. African Americans accounted for 48 percent of new infections among IDUs, and Latinos accounted for 21 percent. Transgender individuals affected by HIV. A 2008 review of studies of HIV among male-to-female women found that, on average, 28 percent tested positive for HIV. are also disproportionately HIV, representing by are heavily
transgender The term transgender refers to people whose gender identity and expression expectations of their biological sex at birth. They may see themselves as male, conformist, or one of a spectrum other genders. Transgender people have diverse sexual orientation and behaviours. Generally, HIV prevalence among transgender women (people who are assigned male at birth but identify as being women) is higher than transgender men (people who are assigned female at birth but identify as being men). However, very little is known about transgender men and their vulnerability to HIV. are different to social female, gender non-
The UNAIDS 2016 2021 Strategy The UNAIDS 2016 2021 Strategy calls for bold action to Fast-Track the AIDS response. It incorporates a human rights-based approach to development and aims to leave no one behind in the AIDS response. The strategy recognizes sexual and reproductive health and rights issues, calls for comprehensive sexuality education and the removal of punitive laws, policies and practices that block an effective AIDS response, including travel restrictions and mandatory testing, and those related to HIV transmission, same-sex sexual relations, sex work and drug use. However these principles are not applicable in all cultures in the world. Some cultures due to conservative customs or due to some religious backgrounds do not accept all these calls or principles.
UNAIDS 90-90-90 targets to end AIDS epidemic In December 2013, the UNAIDS Programme Coordinating Board called on UNAIDS to support country- and region-led efforts to establish new targets for HIV treatment scale- up beyond 2015. In response, stakeholder consultations on new targets have been held in all regions of the world. At the global level, stakeholders assembled in a variety of thematic consultations focused on civil society, laboratory medicine, paediatric HIV treatment, adolescents and other key issues. Powerful momentum is now building towards a new narrative on HIV treatment and a new, final, ambitious, but achievable target: By 2020, 90% of all people living with HIV will know their HIV status. By 2020, 90% of all people with diagnosed HIV infection will receive sustained antiretroviral therapy. By 2020, 90% of all people receiving antiretroviral therapy will have viral suppression. All three percentages by 2030 are increased to 95%. These targets have been achieved in a number of developed countries such as England, by the end of 2020,
The situation of HIV and most-at- risk populations in Egypt Fever Hospitals in different governorates represent the National AIDS Programme. They are responsible for diagnosis, treatment, follow up and PEP to health care workers who are accidentally exposed. However Pre-exposure prophylaxis is not offered by the Ministry. Alexandria is the third governorate in Egypt in the numbers of registered HIV cases after Cairo and Giza. Egypt is recognized by most stakeholders to have some evidence of concentrated epidemic among two populations of people who inject drugs and men who have sex with men ( BBSS 2006,2010) in a setting of overall low prevalence among the general population. At present there is no evidence of an epidemic among any other population that has been confirmed through HIV testing. Egyptian national data estimate the number of people over fifteen years of age living with HIV in 2015 to be 11,000. By that time there were about 6800 PLHA already registered at the national HIV/AIDS data base (i.e. 62%). It is estimated that people living with HIV in Egypt were 22000 by the end of 2019. While the total registered cases were around 13500 (61%).
The situation of HIV and most-at- risk populations in Egypt NGOs working with PLWH in Egypt are not many, around 6-7 organizations. Perhaps the most known is CARITAS.(www.caritas-egypt.org) These NGOs provide support groups, health education, rapid test for HIV. Also some organizations provide outreach and harm reduction services for injecting drug users.
The situation of HIV and most-at- risk populations in Egypt People who inject drugs is a key population to which all stakeholders agree there is a concentrated epidemic in Egypt. The integrated BioBSS-2010 has been used to determine HIV prevalence among these groups whose numbers increased between the two rounds of surveillance in 2006 and 2010, estimated at 6.8% in Cairo and 6.5% in Alexandria. According to the national estimates in 2014, There were estimated 30,000 people who inject drugs in Greater Cairo (Cairo & Giza) and Alexandria with a further 1,000 in Menia out of total 93,400 estimated injecting drug users in Egypt.
The situation of HIV and most-at-risk populations in Egypt Men who have sex with men: In 2010 surveys has been used to determine HIV prevalence among these population to be estimated at 5.7% in Cairo and 5.9% in Alexandria . A package of prevention activities is implemented: education, and comprehensive condom promotion. For men who have sex with men who also inject drugs, the package of activities for people who inject drugs is also offered. Voluntary counseling and testing is provided and people who test positive for HIV may join support groups and are referred for care. However, no systematic tracking of care is done. targeted
The situation of HIV and most-at-risk populations in Egypt Female sex workers Difficulty in defining and accessing female sex workers due to the absence of a definite structure and the prevalence of high levels of stigma, continue to pose great challenges. A wide range of other services are offered through a drop-in center, including health, legal services, psychosocial support, referral for health services, and voluntary counseling and testing. Services were provided only in Cairo and Alexandria
U = U An HIV person with undetectable viral load is unable to pass HIV on to someone else. This is also referred to as "treatment as prevention OR (T as P), or simply U=U, i.e. undetectable = unstransmissible. 95% of people after 6 months of treatment become with undetectable viral loads, i.e. become un-transmissible in UK "Those who are HIV positive by undetectable are less likely to pass HIV than those who say they are HIV negative." Partners who are undetectable and negative showed zero HIV transmission in a study on around 800 couples (one is undetectable and the other is HIV negative) in UK with a long period of follow up.
Stigma HIV stigma is negative attitudes and beliefs about people with HIV. It is the prejudice that comes with labeling an individual as part of a group that is believed to be socially unacceptable. Here are a few examples: Believing that only certain groups of people can get HIV Making moral judgments about people who take steps to prevent HIV transmission Feeling that people deserve to get HIV because of their choices
What is discrimination? While stigma refers to an attitude or belief, discrimination is the behaviors that result from those attitudes or beliefs. HIV discrimination is the act of treating people living with HIV differently than those without HIV. Here are a few examples: A health care professional refusing to provide care or services to a person living with HIV Refusing casual contact with someone living with HIV Socially isolating a member of a community because he is HIV positive Referring to people as HIVers or Positives
What are the effects of HIV stigma and discrimination? HIV stigma and discrimination affect the emotional well-being and mental health of people living with HIV. People living with HIV often internalize the experience and begin to develop a negative self-image. They may fear they will be discriminated against or judged negatively if their HIV status is revealed. stigma they
What are the effects of HIV stigma and discrimination? Internalized stigma or self- stigma happens when a person takes in the negative ideas and stereotypes about people living with HIV and starts to apply them to internalized stigma can lead to feelings of shame, fear of disclosure, isolation, despair. These feelings can keep people from getting tested and treated for HIV. himself. HIV and
What causes HIV stigma? HIV stigma is rooted in a fear of HIV. Many of our ideas about HIV come from the HIV images that first appeared in the early 1980s. There are still misconceptions about how HIV is transmitted and what it means to live with HIV today. The lack of awareness combined with outdated beliefs lead people to fear getting HIV. Additionally, many people think of HIV as a disease that only certain groups get. This leads to negative value judgements about people who are living with HIV. information and
What can be done about HIV stigma? Talk About HIV Talking openly about HIV can help normalize the subject. It also provides opportunities misconceptions and help others learn more about HIV. But be mindful of how you talk about HIV and people living with HIV. Take Action We can all help end HIV stigma through our words and actions in our everyday lives. Lead others to supportive behaviors. to correct
Summary Most-at-risk populations have an important role in propagation of HIV. Working with most-at-risk populations can provide an entry point for PLWH to access care treatment and support. There are packages of services for most-at-risk and vulnerable populations. In Egypt there is HIV concentrated epidemic among IDU and MSM. U=U, i.e. people with undetectable viral loads are unable to pass HIV to others. HIV stigma and discrimination have negative effects on prevention, treatment and care programmes and need to be appropriately addressed.
Important websites www.who.int www.unaids.org www.caritas-egypt.org