Impact of the Opioid Crisis on Ohio's Children and Families
The opioid crisis in Ohio is deeply affecting children and families, with alarming rates of drug use leading to increased foster care placements and challenges in the child welfare system. Through facilitated discussions and activities, stakeholders are working to identify concerns, explore solutions, and make recommendations to support youth, parents, and caretakers in recovery.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Healthy Kids Learning Communities: Facilitated Discussions on the Opioid Crisis in Ohio Angela Lariviere, Youth and Family Advocate CASE WESTERN RESERVE UNIVERSITY CENTER FOR INNOVATIVE PRACTICES
The Opioid Crisis in Ohio The opiate crisis in Ohio is affecting our children and families at alarming rates. In order to understand the impact of the crisis, family and youth discussion groups were held to identify concerns and make recommendations.
Discussion Groups Northwest, Southwest, Southeast, Central, Upper Northeast and Lower Northeast Regions They included: Youth, Families and Providers
Facilitated discussion and activities were used to: explore the impact of the epidemic and give voice to ideas and concerns. explore strategies and models that support youth, parents and/or kinship caretakers in recovery.
OPENING INTRODUCTION ACTIVITY: COMMON CIRCLES GOALS AND EXPECTIONS DEFINE THE PROBLEM WRITTEN FEEDBACK IDENTIFY COMMUNITY EXPLORING RESOURCES MAKE RECOMMENDATIONS EVALUATIONS ADJOURN A G E N D A
What We Know Defining the Problem
50% of children taken into custody in 2015 had a parent actively using drugs with 28% actively using opiates or heroine 70% of children under the age of 1 in custody had a parent actively using opiates or heroine Facts: Children in the System Children in relative placement has increased 62% Foster Care placements have increased 11%. Shortage of front line staff In 2016, 1 in 4 cases workers left their positions 1 in 7 case workers left their position all together Ohio ranks 50th in the nation for state funding for Child Welfare *Source: Public Children Services Association of Ohio
The FACTS Ohio is the Second worst state in the nation for drug overdoses, with Dayton ranked 1rst with the highest per capita overdoses in the county. We rank in the top 6 for most deaths. Children in relative placement has increased 62% Foster Care placements have increased 11%. While Opiate use has increased the State allotment of Child Welfare funding has decreased by 21%.
What we see What we don t see Families and children Doubled up with Grandparents and other Relatives due to parents Opiate addiction but not Officially involved with Child welfare.
Written Responses What is the biggest issue facing your community? What is one barrier to accessing treatment or services in your area? What is the most important thing you need when helping a friend or family member who is addicted?
What is the biggest issue facing your community? Drugs - #1 Violence - #2 Lack of police officers Nothing to do No safe activities for youth People thinking it is OK to get high Peer pressure Lack of awareness about Trauma and Addiction Lack of mental health treatment for children in foster care Addiction Stigma Parent participation Unemployment Broken homes Understanding culture and community Lack of funding for services Nothing better to do but get high Poverty Not enough free things to do Overdoses Gangs
What is one barrier to accessing treatment or services in your area? Access Age Cost Culture Lack of options in low income areas Lack of services and inpatient for youth Lack of services for the entire family Parents not giving permission for youth to participate in treatment or counseling Transportation to follow up Not knowing how to get signed up Lack of school based services Lack of understanding about what is available No support No medical insurance Have to get in trouble before you can get services No local options Not having anywhere to go after Keeping motivated
What is the most important thing you need when helping a friend or family member who is addicted? Access to resources - #1 Empathy Some type of Peer support - #2 Whole family resources Have a support system Information about how to get access to treatment People who know and understand Workers with personal experience Resources Support groups Knowing how to connect to services Someone you can trust Medical/professional guidance Family Affordable sober living options Faith Love Support
Defining Community Roles, Barriers, Supports and Recommendations
Self Peers Family Police Emergency Responders: Including EMT and ER Schools Government Treatment Programs: In and out patient Courts Child Welfare Community Agencies: including churches, community centers, afterschool programs
Role S c h o o l s Teach, provide support services, prepare for life Support Safe space, trusting relationship, provides support services Peer to Peer, provides opportunity for mentor, Basic needs: food Barriers Mandatory reporters, not enough Behavioral Health support Not enough funding, no transportation to afterschool activities Recommendations Better defined roles and expectations for schools, More funding for Behavioral Health support for schools Trauma informed training for teachers and administration
Role P o l i c e Safety, Patrol neighborhood, Make everyone safe, arrest drug dealers Support Resource officers in school, Crime intervention, Safety from drugs on street Barriers Not enough training, Not enough funding, Not enough police, Corruption Not enough focus on crime prevention, not getting to know the community Recommendations More training for police in Crisis Intervention, More funding for additional officers Create programs to build community relationships with police Better background checks to know about drug or criminal history
Role C o u r t s Provide justice, Punish crime, Provide intervention, Mandate treatment Support Drug courts, Family interventions, Mandating treatment Barriers Issues have to escalate before they are able to intervene, Not enough drug/mental health courts, Court the only way to get services Recommendations Spend more funds on prevention and early intervention, look for trauma informed punishment, include entire family when can Create programs to build community relationships and understanding of the courts role, attach punishment and reward to treatment
Role C h i l d W e l f a r e Make homes safer, Find placement for kids in crisis, provide case management Support Prove support for families, Make referral's to treatment, Mandate families to get help Get services for kids, Provide follow-up and check ins. Barriers Overloaded, no response or call backs, Not enough placements (especially for older youth) Relative placement with other drug addicted family members, No support, inexperienced workers Recommendations More funding, Provide support for older youth when placements are not available, Provide better prevention and in home supports before taking custody, Build better partnerships with families and youth Work on building trust with youth and communities, Build a better reputation, Offer youth self referral options
O t h e r Self Role: Take care of yourself, ask for help Barrier: depression, self hate, not recognizing when there is a problem Support: self motivation, only you know you Recommendation: More outreach and information on resources, peer support Family Role: Primary caregivers, provide support, participate in treatment Barrier: Culture of addiction, poverty, generational issues, no time, no support Support: love, trust, loyalty, place to live, resources Recommendation: Whole family treatment plan, provide resources, peer support Peers Role: be there for you, provide support, listen, give advice Barrier: Lack of experience, bad influences, fake friends, pressure Support: available anytime, open and honest, trust, place to stay Recommendation: include in treatment plan, provide peer training
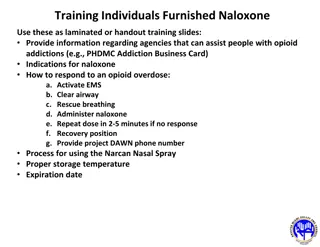
First Responders O t h e r Role: Come in an emergency, prevent death by OD, admin Narcan Barrier: Response time in rural areas Support: trained in responding to OD Recommendation: More funding, more training with community partners, families Community Role: Provide support and services Barrier: No funding, not EB, grassroots, transportation Support: Trust, knows community, faith based Recommendation: Incorporate into funding and treatment for families and youth Treatment Centers Role: inpatient or outpatient services Barrier: Lack of beds, far away, not enough funding, no family services Support: services, counseling, outpatient, when avaiable. Works if long enough Recommendation: better follow-up, inclusion of whole family, community referrals
Making Statewide Recommendations 10 Common Priorities
1. Flexibility in funding community based solutions, not only evidence based practice but also to allow new ideas. 2. Support and interventions for families through Child Welfare before major crisis and support for older youth who are unattached to families. 3. Strategic partnerships with community based agencies including Y programs, community centers, faith based, afterschool programs, and housing agencies. 4. Better communication between Government agencies local community agencies and persons with lived experience. 5. Focus on culture, mental health and trauma training for Police.
6. Funding and support for school based services, including behavioral health services and trauma, community resources and intervention training for teachers. 7. Access to self and family referral to treatment facilities. 8. Funding for professional peer support services to family and youth. 9. Increase drug and mental health interventions and diversion programs in the court system. 10. Entire family issues and dynamics should be considered when treating children and youth for behavioral health problems.
FOR MORE INFORMATION SUBSTANCE ABUSE AND MENTAL HEALTH SERVICES ADMINISTRATION www.samhsa.gov Public Children Services Association of Ohio www.pcsao.org Case Western Reserve University Center for Innovative Practice https://case.edu/socialwork/begun/center-for-innovative- practices-cip Bobbi Beale bobbi.beale@case.edu Angela Lariviere : Angela.yepdirector@gmail.com