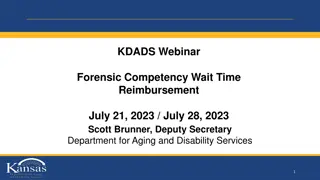
Implementation of Outpatient Hospital Reimbursement Methodology
This presentation covers the implementation of a new outpatient hospital reimbursement methodology by EGID, focusing on changes from a percentage-of-charges approach to a fee schedule based on Medicare's Ambulatory Payment Classifications. It discusses the impact on providers, the introduction of Comprehensive APCs, and the implementation of J1 logic in Medicare reimbursement.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
1 EGID J1 Implementation PUBLIC HEARING MAY 25, 2018
Presentation Topics 2 EGID s outpatient hospital reimbursement methodology. CMS changes to the Medicare Hospital OPPS. Implementation of composite APCs/J1 logic. Rationale for EGID s adoption of J1 logic. Impact on providers.
EGID Outpatient Hospital Reimbursement Methodology 3 Changed from a primarily percentage-of-charges approach to a fee schedule based on Medicare s Ambulatory Payment Classifications (APCs) beginning 4/1/16. Phased in over 3 years, with final phase-in implemented 4/1/18. Most services are reimbursed at a percentage of the Medicare APC rate (based on the national Addendum B rates by HCPCS code). Tier-specific percentages. Some services are packaged or bundled in alignment with Medicare logic (i.e., status indicator N). Separate reimbursement for most revenue codes phased out. Selected revenue codes reimbursed at a percentage of charges.
Introduction of Comprehensive APCs 4 CMS introduced in OPPS Final Rule October 2014 and implemented 1/1/15. Initially 25 C-APCs in 2015 (219 HCPCS codes). Currently 60 C-APCs in 2018 (2,756 HCPCS codes). Some, but not all C-APCs are device intensive. Procedure codes with J1 status indicator are always assigned to a comprehensive APC. Reimbursement is similar to a DRG or bundled payment. Adjunctive services billed with a procedure code assigned a J1 status indicator are packaged. When certain pairs of J1 services are reported on the same claim, claim is eligible for a complexity adjustment (payment for the claim based on the rate of the next higher comprehensive APC within the same clinical family).
5 Implementation of Comprehensive APCs CMS substantially increased Medicare rates for most codes with a J1 status indicator in anticipation of applying packaging/bundling logic.
Medicare J1 Logic 6 The following items and services are packaged/bundled under the Medicare J1 logic: Procedure codes with status indicators P, S, T or V. Procedure codes with status indicator J1. Non-pass-through drugs and biologicals (status indicator K). Blood products (status indicator R). DME (status indicator Y). Therapy services (HCPCS codes with status indicator A reported with therapy revenue codes).
Medicare J1 Logic, cont. 7 The following services are excluded from the J1 logic and reimbursed separately: Brachytherapy services (status indicator U). Pass-through drugs, biologicals and devices (status indicators G or H). Corneal tissue, CRNA services, and Hepatitis B vaccines (status indicator F). Influenza and pneumococcal pneumonia vaccines (status indicator L). Ambulance services. Mammography. Certain preventive services.
Proposed EGID J1 Logic 8 Medicare J1 logic packages/bundles many more services than EGID proposes to package/bundle. EGID proposes to package/bundle only the following items and services: Procedure codes with status indicators P, S, T, or V ONLY those in the range 10000-69999 and 92900- 93999. Procedure codes with status indicator J1 ONLY those in the range 10000-69999 and 92900-93999.
Items Excluded from EGID Logic 9 Non-pass-through drugs and biologicals (status indicator K).* Blood products (status indicator R).* DME (status indicator Y).* Therapy services (status indicator A).* Brachytherapy services (status indicator U).** Pass-through drugs, biologicals and devices (status indicators G or H).** Corneal tissue, CRNA, and Hepatitis B vaccines (status indicator F).** Influenza and pneumococcal pneumonia vaccine services (status indicator L).** Ambulance services.** Mammography.** Certain preventive services.** *Medicare bundles these items; however, providers would receive separate reimbursement under EGID s proposed logic. **Items not bundled under Medicare logic or EGID s proposed logic. Providers receive separate reimbursement.
Rationale for Adoption of J1 Logic 10 Under EGID s current outpatient hospital reimbursement methodology, most adjunctive services billed on claims where a J1 status indicator is present are reimbursed separately. CMS increased Medicare rates for the majority of HCPCS codes with J1 status indicators in anticipation of bundling adjunctive services. Because most of EGID s reimbursement rates are established at a percentage of the Medicare rate for each HCPCS code, EGID is now paying higher rates for these codes as well as paying separately for most adjunctive services. EGID proposes to package/bundle some, but not all of the same adjunctive services that Medicare packages/bundles. Most radiology, lab and drug codes will continue to be reimbursed separately.
Estimated Impact of J1 Logic 11 Estimated 1-year* change in total allowed for claims containing J1 codes: -18% Tier 1: -15% Tier 2: -22% Tier 3: -15% Tier 4: -13% *Modeled for CY 2018 using CY 2017 paid claims. Implementation proposed for CY 2019.
12 Questions/Comments