Importance of Proper Inhaler Technique in Respiratory Care
Improper inhaler technique can lead to ineffective drug delivery in patients with COPD and asthma, resulting in increased symptoms, exacerbations, and hospitalizations. This article stresses the significance of correctly administering inhaled medication to improve patient outcomes and prevent potential complications.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
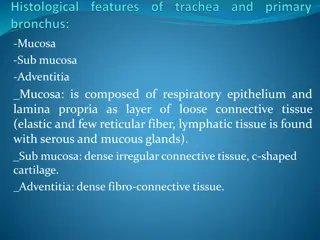
Inhaler Technique Training for Respiratory Ward Staff Author: Jill Leyshon Asthma & COPD Specialist Nurse
Why Does Inhaler Technique Matter? COPD & Asthma are controlled with Inhaled Medication o Inhaled drugs reduce exacerbations and improves symptoms (such as breathlessness) and quality of life 70% of patients make an error with a metered dose inhaler Up to 50% of patients make an error with a dry powder inhaler o Poor technique can mean the drug is not delivered to the lung and will not have an effect o Poor technique is associated with increased symptoms, exacerbations & hospitalisations o It is important to remember, patients can die from an exacerbation of asthma or COPD Molimard et al. J Aerosol Med 2003;16;249 254
Preventing a lung attack with inhaled therapy is equally as important as preventing a heart attack with cardiac medication o We carefully administer tablets and IV drugs o We also need to observe the delivery of inhaled medication and correct any errors in technique
Teaching correct Inhaler techniques in hospital prevents 30 day readmissions .but not 90 day readmissions Inhaler techniques often wane and patients get into bad habits Therefore, every hospital admission is an opportunity to check and correct at every administration Press VG. Ann Am Thorac Soc2016pp:816-24
What are we asking you to do? When administering inhalers, observe the patient using it Identify poor technique Coach the patient as needed Highlight if you think the patient needs a device change Document in the notes that you have checked & the outcome Work through this learning module to increase your knowledge and skills about inhalers Can you legitimately sign to say an inhaled drug has been administered without observing the patient taking it?
Seven Basic Steps For Inhaler Use 1. Prepare 2. Exhale (away from mouthpiece) 3. Posture 4. Inhale Flow Rate 5. Breath Hold 6. Wait, then repeat if necessary 7. Mouth Rinse if administering an inhaled steroid Remember, an error affecting drug delivery can occur at any step .and replace inhaler cap!
Errors can occur at any step Procedure Step 1. Prepare Error To get the inhaler ready for use. Errors in preparing commonly result in no drug delivery Exhaling first increases the volume of the inhaled breath and therefore drug delivery Not exhaling is a very common error 2. Exhale Patients should be sitting or standing upright to allow lung expansion, chin slightly tilted upwards Poor posture can result in the drug being delivered to the mouth/ throat not the lungs 3. Posture Metered dose inhalers - slow steady inhalation Dry Powder inhalers - quick deep inhalation Incorrect inhalation flow can mean little or no drug delivery to the lung 4. Inhale To allow the drug to drop down into the lung and bind to the relevant receptor This is commonly missed 5. Breath Hold Wait 30-60 seconds after using an MDI the device must be shaken again before the 2nd dose No wait & re-shake of an MDI results in only the first dose being delivered 6. Wait MDI s Inhaled steroids can cause dysphonia (an altered voice) sore mouth & throat/ oral thrush Can be caused by poor technique causing mouth deposition 7. Mouth Rinse
Using a Metered Dose Inhaler (MDI) (sometimes called a pMDI or pressurised MDI) MDIs need a Slow and Steady Breath Watch this video https://www.asthma.org.uk/advice/inhaler-videos/pmdi/ 3 Common Errors o Not shaking o Not waiting and shaking again before 2nd puff o Inhaling too quickly inhalation should last for 4-5 seconds SPACER! Very few patients can use an MDI well We recommend all patients use a
Using an MDI with Spacer o MDIs spray out at around 70mph o This makes co ordination of spray and breath very difficult o A Spacer is a holding chamber, allowing the patient more time to inhale the drug using one or multiple breaths Watch these videos https://www.asthma.org.uk/advice/inhaler-videos/single-breath-and-hold/ https://www.asthma.org.uk/advice/inhaler-videos/tidal-breathing/
The Respimat device The other device you will often encounter when a slow and steady breath is required, is the Respimat. If patients are struggling to use the Respimat, but are unsuitable for a dry powder inhaler, you can use it with a Spacer Watch this video https://www.asthma.org.uk/advice/inhaler-videos/respimat/
Dry Powder Inhalers (DPIs) In the UK we are starting to use more DPIs, reserving MDIs for patients who are unable to use a DPI o They are often easier to use o They have a much lower carbon footprint than MDIs DPIs require a fast and deep inhalation for 2-3 seconds o The breath pulls the drug out of the inhaler o Some DPIs need a stronger inhalation than others o Some DPIs are very simple to use, however, others are complicated and require good manual dexterity Preparation varies and is specific to each device type In Cornwall we are encouraging the use of the easiest devices
Easy Complicated Patients with severe disease may not be able to breathe hard and fast enough to use a DPI We can test using a whistle or incheck device
Using Dry Powder Inhalers Watch these videos https://www.asthma.org.uk/advice/inhaler-videos/nexthaler/ https://www.asthma.org.uk/advice/inhaler-videos/ellipta/ https://www.asthma.org.uk/advice/inhaler-videos/easyhaler/
How can I find out how to use other inhalers? Asthma UK https://www.asthma.org.uk/advice/inhaler-videos/ You can also share these videos with patients Rightbreathe https://www.rightbreathe.com This site, for healthcare professionals, has a wealth of information about inhalers, including videos There is also a free smart phone App
I have identified poor technique but feel out of my depth in finding a solution Identifying poor technique is a great first step 1. If it s a simple error (i.e. exhaling) retrain the patient 2. Ask for help from your Ward Pharmacist or Asthma & COPD Specialist Nurse 3. Look to observe what the Ward Pharmacist or Asthma & COPD Specialist Nurse do - build your confidence and experience 4. Remember, Inhalers are easy when you know how!
What are we asking you to do? Lets recap Learn & embed the 7 steps of inhaler use in your clinical practice When administering inhalers, observe the patient using it every time Identify poor technique & correct with the patient Highlight if you think the patient needs a device change Document in the notes that you have checked, including the outcome
Disposal of Used or Unwanted Inhalers Greenhouse gases have far-reaching environmental and health effects. They cause climate change by trapping heat and also contribute to respiratory disease from smog and air pollution. The propellants in commonly used MDI inhalers contain powerful greenhouse gases Even after the MDI inhaler has been used, significant amounts of these damaging gases remain in the canister Landfill disposal of MDI inhalers is extremely harmful to the environment due to the residual gas from canisters being released in to the atmosphere as greenhouse gases Plastics take 100s of years to decompose and even then, only if they are exposed to sun, moisture and air. Burying plastic inhalers in landfill blocks any exposure to those elements and prevents discomposure completely.
Disposal of Used or Unwanted Inhalers Inhalers returned to Pharmacies for safe disposal can be disposed of with other medicine waste. This waste is thermally treated to destroy the greenhouse gases completely. If all inhalers in the UK were returned for safe disposal, this could save 512,300 tonnes of CO2eq annually. This is equivalent to driving a car around the world 88,606 times. Remember, all inhalers should be returned to a Pharmacy for safe disposal