Improving Access to Personalised Care in London Community of Practice: Social Prescribing & Community Led Prevention
"Discover the value of personalised care in secondary care, focusing on holistic support, reducing demand/capacity burden, and improving patient outcomes. Learn about workstream priorities and activities to improve access to personalised care across secondary care in London."
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
@SP_LDN rf-tr.socialprescribing@nhs.net Improving access to personalised care in secondary care London Community of Practice Terms of Reference (ToR) Social Prescribing & Community Led Prevention
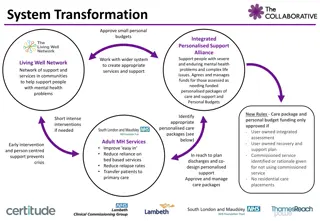
Value of Personalised Care in Secondary Care Holistic support and personalised care can help to reduce the demand and capacity burden for secondary care staff, support cost savings for the NHS and improve patient outcomes. Evidence suggests that access to more holistic, personalised care can have a positive impact on: Demand & capacity: Population health: Patient outcomes: Economic outcomes: People from the most deprived areas & most impacted by health inequalities are more likely to be in poor health & most likely to attend A&E more frequently. Personalised Care improves integration of health & social care systems in the community and proactively targets groups facing higher levels of health inequalities, thereby improving population health. Improvements in mental health, social connections & in overall wellbeing, in turn improves clinical outcomes. Evaluations of Social Prescribing demonstrate a favourable SROI & studies reported a link to reduced secondary care use. The NAPC found that Social Prescribing & Care Coordination support led to increased activation, less hospital admissions, less falls, less GP contacts . Personalised care addressing social determinants can help prevent problematic polypharmacy exacerbated by the socioeconomic gradient saving the NHS ~ 1 billion on medicine related admissions (see slide 11 in appendix). A study in 2017 from the University of Westminster illustrated Social Prescribing led to a 24% fall in A&E attendance. A prediabetes support group set up in Waltham Forest, used Social Prescribing to engage & tailor support for people from Black & South Asian backgrounds. NHSE are encouraging expansion of personalised care support in secondary care. Find out more about current policy, context and background in slide 12 in Appendix.
Improving access to personalised care across secondary care: Workstream Priorities The Social Prescribing & Community Led Prevention Team will support London's health and care systems to scale community centred models of care which focus on addressing the wider social determinants of health and target those experiencing the greatest health inequalities Improve access to Personalised Care across secondary care in London Workstream 3 Support and scale approaches to improve access to holistic support in secondary care leading to more sustainable and integrated pathways Develop resources, build the evidence base and communicate the impact Priorities Activities As part of this workstream, the Social Prescribing & Community Based Prevention Team are committed to: Sharing and spreading examples of services across London that are improving access to holistic support in secondary care, with a particular focus on sharing approaches, models, learnings, enablers and impacts. Supporting frontline approaches & the transformation of services that are embedding access to non-clinical wellbeing support in the community. Improving patient experience through better integration between local services e.g. between primary care, secondary care, VCSE and local communities, strengthening place-based partnerships. Advocating for the impact of holistic care in secondary care settings in order to influence commissioning and funding. See slide 13 & 14 in Appendix for more information on our 23/24 team priorities & Theory of Change for this workstream.
Improving access to holistic care in secondary care: Activities What we've been doing so far Planned activities Mapping the landscape of social prescribing & personalised care in secondary care across London, including: o Models, cohorts and referral pathways o Enablers and challenges o Funding models o Supervision & training o Evaluations and impact o Similar work supporting these initiatives Support secondary care to embed access to non-clinical wellbeing support in the community. Develop and share resources to support rollout of holistic support in secondary care. Develop cross-sector partnerships to embed personalised care approaches in acute settings. Developing case studies of innovative and exciting pilots/projects embedding personalised care roles in secondary care. Read here! Support better integration between local services. Providing direct support & resources to pilot projects in development.
What we've heard so far: CoP Scoping Session We want to create a platform for all those interested or involved in developing personalised care roles and access to holistic support across secondary care settings in London. We had 16 colleagues attend with representation from: We hosted a scoping session on 13th June to explore: Social Prescribers who have/are exploring work in secondary care settings What people hope to gain from a CoP in this space How the CoP should be shaped to ensure it is most useful for all involved ICS personalised care leads SP managers/team leads supporting roles based in secondary care settings We all shared: What brings us to being interested in the CoP What we hope to gain from a CoP What we envisage should be the main purpose/aims of the CoP? (ranking suggestions) What we would like to see included in sessions Preference for timing, frequency & online connection Suggested questions, topics or themes to cover in future sessions Lead Clinicians based in NHS hospital trusts Transformation managers at NHS hospital trusts See the workplan for a detailed summary of themes
Proposed purpose & scope The top things perceived as useful aims for a CoP were: To build connections and a wider support network to share learnings & signpost to scale more integrated and sustainable approaches. To strengthen place based partnerships & community development by bridging the gap between primary care, secondary care and community organisations. To amplify impacts to influence funding & commissioning enabling expansion of models that are improving access to personalised/holistic support for target cohorts experiencing inequalities across London. The CoP aims to achieve this through: Drawing on insights, expertise and learnings, and sharing ideas Enabling cross sector collaboration at place & regionally Building a network of champions able to advocate for impact and disseminate learnings/resources Proposed goal/mission: To champion and support development of integrated & sustainable approaches to improve access to personalized care in secondary care across London.
Theory of change for the CoP Inputs Activities Outputs Outcomes Impact Engagement with wider stakeholders across specialties & pathways in secondary care Brainstorm, plan & deliver useful outputs/activities Network of champions able to advocate for the impact of personalised care in secondary care Greater understanding of what s happening across London Personalised care roles are more embedded in secondary care settings Diverse discussions on topics selected by the group Stronger connections across geographies, specialisms & sectors Commitment to regular sessions CoP sessions Improved access to holistic support in secondary care Bank of resources sharing examples & supporting development of models e.g. case studies, toolkits Share projects or exciting work with Q&A Time to support development of outputs that will be useful for the system Reduced demand for secondary care services freeing up capacity for clinical staff Collective voice amplifying impacts to influence policy, strategy and funding Creative exercises to unpick challenges & brainstorm solutions
Proposed membership Core representation at CoP (10-30) Additional/visiting members Personalised care roles based in secondary care ICS personalised care leads Secondary care staff e.g. medical consultants, clinicians, nurses, social workers etc. Allied Health Professionals VCSE organisations Chief Execs Hospital Trust charities Specialist alliances or networks Service improvement teams in Trusts People with examples of Personalised Care in secondary care across the system (regionally & nationally) Patient voice/lived experience Experts in relevant topics e.g. Social Impact Bonds, Evaluation, communicating impacts, data sharing Important to ensure: Representation across London ICSs, hospitals and community sector All core members are sighted and agreed on the purpose, aims & scope of the CoP Flexibility in terms of attendance and commitment to output delivery, based on preferences, capacity and relevance to each member Engagement strategy to share outputs or outcomes with a wide range of stakeholders
Proposed meeting structure Every 6 weeks for 1hr MS Teams channel available for connection between meetings Regular core members + additional depending on topic Breakout rooms or whole group discussions depending on number in attendance Topic idea for next meet shared and agreed in last meeting Item Time Welcome & introductions for new faces 5 mins Updates from regional/national/members 10 mins Options depending on topic/request: Brainstorming & planning useful activities or outputs that the CoP could deliver Diverse discussions on topics selected by the group (collectively or in breakouts) Sharing projects or exciting work with Q&A Creative exercises to unpick challenges & brainstorm solutions Feedback from the group & AOB 35/40 mins 5/10 mins
Social needs & economic gradient Problematic polypharmacy: Inappropriately given multiple medications; increases with deprivation levels Up to 10% Life events Environmental stressors Low socioeconomic status Increased wear and tear on the body of prescriptions are not necessary. 6.5% of hospital admissions are caused by adverse drug reactions; 20% Chronic conditions Substance abuse Mental health issues (if in the >65 years age group). 66% Medicine related admissions are preventable would save NHS approx. 1 billion More adverse drug reactions More pharmaceutical prescriptions Regional Drug and Therapeutics Centre (RDTC) led a study on the effect of social prescribing on medicines use in primary care and found that SP slowed increases in prescribing of antidepressants, likely by improving wellbeing
Policy, context & background 2023/24 NHS priorities and operational planning guidance Guidance released 23rd December 2022 NHSE asking systems to: 1. Prioritise recovering core services and productivity 2. Return to delivering key ambitions in the NHS Long Term Plan (LTP) 3. Continue transforming the NHS for the future NHSE published: A letter to systems setting out further recommendations regarding winter resilience plans Guidance to Supporting High Frequency Users (HFU) through proactive personalised care, delivered by Social Prescribing Link Workers, Health and Wellbeing Coaches and Care Coordinators A short video which also outlines how one system is using social prescribing to help Persistant Users in Dudley 2022/23 NHSE commitments: Publication setting out package of measures to boost capacity ahead of winter: We will maximise recruitment of new staff in primary care across the winter, including care coordinators and social prescribing link workers September Winter pressure new letter to systems: ARRS-recruited staff treated as the core general practice cost base beyond 2023/24 meaning permanent contracts can be offered these staff groups Weencourage PCNs to continue to recruit, making full use of their ARRS entitlement to improve access to care and support for patients, with the knowledge that support for these staff will continue Changes to DES contract: 37 million in funding released to PCNs as part of a monthly PCN Support Payment from Oct 2022-March 2023 to support PCN capacity and ARRS maximum reimbursement rates increased for 2022/23 to account for the Agenda for Change uplift Next steps for integrating primary care: Fuller stocktake report highlighting importance of: Providing proactive, personalised care in multidisciplinary teams, for example for those with Long Term Conditions Building integrated teams in every neighbourhood, from across PCNs, wider primary care providers, secondary care teams, social care teams, and domiciliary and care staff A culture shift towards a more psychosocial model of care that takes a more holistic approach and realignment of the wider health & care system to a population-based approach e.g. through aligning secondary care specialists to neighbourhood teams
Social Prescribing & Community Led Prevention Supporting London s health and care systems to develop more proactive, preventative and community centred approaches to improve the health and wellbeing of those most impacted by health inequity Workstream 1 Workstream 2 Workstream 3 Secondary Care System Support & Evaluation Community Assets Develop a thriving personalised care workforce to maximise impact, ensuring benefits are measured, understood, and effectively communicated Develop local community assets to address local unmet needs Improve access to personalised care across secondary care Priority Activities Priority Activities Priority Activities Supporting system leaders and managers to embed proactive, personalised care workforce development support inc. leadership, recruitment & retention Support evidence, evaluation and demonstrating impact of Social Prescribing Support and scale approaches to improve access to holistic support in secondary care leading to more sustainable and integrated pathways Develop resources, build the evidence base and communicate the impact Develop and scale a community chest for social prescribing type model across London Support the expansion of specialist community assets to support local population needs. Initial focus BCYP & Social Welfare & Legal Advice To deliver maximum impact for London we will: Establish cross sector partnerships to harness collective assets and resources Provide a voice for community prevention in London and a platform to share latest guidance, updates, innovations, good practice and evidence Deliver once for London projects, co-produce shared resources, and hold regional events and webinars to share best practice to support local delivery Continue to develop the evidence across all our activity and remain outcome and impact driven to support sustainable long-term transformation Convene stakeholders to shape our work ensuring its adding value to local systems and support systems to align with regional and national priorities Offer bespoke tailored support based on local priorities. This includes specific support to ICSs, boroughs, neighbourhoods, providers, and other regional programmes as agreed.
Improving access to Personalised Care across secondary care: Workstream Theory of Change SP and other personalised care ARRS roles are not always well supported outside of primary care. There is no London wide strategy or ambition to scale personalised care roles across acute settings. Many projects are in early development and as such lack thorough evaluations and impact data. Acute and secondary care services are experiencing underfunding, high demand compared to capacity, and workforce pressures. Pressures could be reduced through providing appropriate holistic support to patients and workforce, utilising assets in the community. Challenge Personalised care roles can help to address wider social determinants of health, which improves patient experience and outcomes. Using Personalised Care roles effectively in secondary care enables proactive targeting of at risk groups with inequality in access, experience or outcomes to reduce health inequalities, helping to improve population health and prevention. Identifying underlying causes of reattendance, readmission or poorer outcomes can reduce dependence on both primary and secondary care services. Supporting expansion of SP & personalised care outside of primary care, alongside other activity supporting holistic care, improves integrated care across London through enabling an interface between integrated neighbourhood teams (including VCSE, primary care) & secondary care. Opportunity Support secondary care to embed access to non-clinical wellbeing support in the community Develop and share resources to support rollout of personalised care support in secondary care Develop cross-sector partnerships to embed personalised care approaches in acute settings Support better integration between local services Aims