Improving Blood Pressure Accuracy in Pediatric Primary Care Clinic
Explore a quality improvement project aiming to enhance blood pressure accuracy in pediatric patients in primary care settings. The project involves staff training, education on blood pressure measurement techniques, and assessment of systolic accuracy pre- and post-intervention.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
IMPROVING BLOOD PRESSURE ACCURACY IN PEDIATRIC PRIMARY CARE CLINIC: A QUALITY IMPROVEMENT PROJECT Brenda Jobe, DNP, RN, FNP
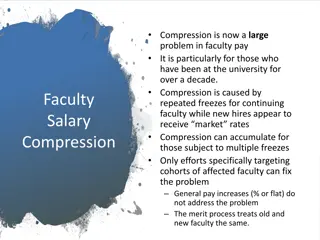
BACKGROUND AND PURPOSE Approximately 1 in 7 children in U.S. have hypertension Jackson, et al., (2018) Complications of untreated pediatric hypertension include cardiac and kidney damage Meng, et al., 2015; Vasilevska-Ristovska, et al., (2018) Hypertension diagnosis is dependent upon accurate BP readings Purpose: Improve accuracy of staff BPs on pediatric patients Objectives: 100% of staff obtain accurate blood pressures on- 1) blood pressure simulation arm 2) on pediatric clients
LITERATURE REVIEW No literature regarding BP accuracy for professionals in practice Nursing students overestimate their theoretical and practical knowledge of BPs Pereira, Nascimento, Lima, Rezende Dazio and Coelho Leite Fava (2018) Blood pressure simulation arm (BPSA) improved accuracy in pharmacy students with each additional attempt Seybert and Barton (2007) Accuracy similar in BPSA as in live subjects Lee, Sobieraj and Kuti (2010) If pharmacy students struggle with accuracy, it will be seen in high and low blood pressures Bottenberg, Bryant, Haack and North (2013)
METHODS IRB approval from university and Pediatric Primary Care Clinic (PPCC) Sample: Convenience sample 2 Pediatric Primary Care Clinics in Upper Midwest Participants- Registered Nurses and Medical Assistants Baseline data: staff manual BP vs automatic BP Baseline data: Video for cuff inflation & rate of descent (n=34 BPs)
METHODS Survey prior to Intervention (n=19) Intervention (n=19) Education (2-step BP, Cuff size, Rate of deflation) Practice on blood pressure simulation arm (BPSA) before and after education Survey after intervention (n=19) Post-intervention data: Staff BP vs automatic BP and (n=18) Post-intervention data: Video for cuff inflation & rate of deflation (n=18 BPs)
RESULTS: SYSTOLIC ACCURACY/BPSA 5.8 5.6 5.4 mm/Hg 5.2 5 4.8 4.6 Goal Pre-Intervention Post-Intervention Not Statistically Significant Change p value .662 Goal: Difference <5mm/Hg= Goal Not Met
RESULTS: DIASTOLIC ACCURACY/BPSA 5 4.5 4 3.5 3 mm/Hg 2.5 2 1.5 1 0.5 0 Goal Pre-Intervention Post-Intervention Not Statistically Significant Change p value .425 Goal: Difference <5 mm/Hg = Goal Met
SYSTOLIC ACCURACY ON PEDIATRIC CLIENTS 16 14 12 10 mm/Hg 8 6 4 2 0 Goal Pre-Intervention Post-Intervention Statistically Significant Change p value .03 Goal: Difference < 5mm/Hg = Improvement Post-Intervention Goal Not Achieved
DIASTOLIC ACCURACY ON PEDIATRIC CLIENTS 8 7 6 5 mm/Hg 4 3 2 1 0 Goal Pre-Intervention Post-Intervention Not statistically Significant p value .35 Goal: Difference <5mm/Hg= Improvement Post-Intervention Goal Not Achieved
RATE OF CUFF DEFLATION ON PEDIATRIC CLIENTS 9 8 7 mm/Hg/sec 6 5 4 3 2 1 0 Goal Pre-Intervention Post-Intervention Not Statistically Significant Change p value .614 Goal: Difference <2mm/Hg/sec = Improvement Post-Intervention, But Goal Not Achieved
MAXIMUM INITIAL CUFF INFLATION ON PEDIATRIC CLIENTS 160 155 150 mm/Hg 145 140 135 130 Pre-Intervention Post-Intervention Statistically Significant p value .015
STAFF SURVEY RESULTS ABILITY Before intervention Likert Scale 1-5 (5 is very confident) prior to educational intervention with BPSA 37% of staff rated themselves at 5 (very confident) regarding ability to obtain accurate BP on child 3-17 yrs 58% of staff rated themselves at 4 (confident) regarding ability to obtain accurate BP on child 3-17 yrs
STAFF SURVEY RESULTS Frequency at which staff deflates cuff at proper rate: self-report prior to educational intervention with BPSA 100% of the time- 1 staff 95% of the time - 2 staff 90% of the time - 6 staff 80% of the time - 1 staff 60% of the time - 1 staff 50% of the time - 3 staff 0% of the time- 1 staff Did not know 2 staff Left blank 1 staff
SURVEY RESULTS BARRIERS TO CHANGE Staff report - after educational intervention BP on young children (moving, talking, anxious) Lack of time Room configuration Lack of management support to change room configuration
NEXT STEPS? Utilize Kotter s Change Model Compare manual pressure by staff to manual pressure of investigator Intervention More practice time with the 2 step Intervention includes following the MA to the next step where coaching occurs as they incorporate a 2- step BP, measure cuffs and slow down the rate of decent. Very select preceptors for new MAs on orientation (it might not be who you think) Elite mentors to precept new MA (it might not be who you think) The real answers are within the staff themselves!!
CONCLUSION Additional practice change is needed to achieve accurate blood pressures. Staff skills are not congruent with staffs perception of the own skills. Recommend deliberate use of Kotter s Change Model, Kotter (2012) & Plan-Do-Study-Act (IHI) Model for future projects.
THANK YOU Marquette Faculty - Dr Rapala, Dr Breakwell & Dr Miles Dr Rohloff Jaspreet Samra Amy Kastens Participating BP champions and clinics
REFERENCES Bottenberg, M.M., Bryant, G.A., Haack, S.L. & North, A.M. (2013). Assessing pharmacy students ability to accurately measure blood pressure using a blood pressure simulator arm. American Journal of Pharmaceutical Education, 77(5). Institute for Healthcare Improvement. (2020). Tools: Plan-do-study-act (PDSA) worksheet. Retrieved from http://www.ihi.org/resources/Pages/Tools/PlanDoStudyActWorksheet.aspx Jackson, S.L., Zhang, Z., Wiltz, J.I., Loustalot, F., Ritchey, M.D., Goodman, A.B., & Yang, Q. (2018). Hypertension among youths United States, 2001-2016. United States Department of Health and Human Services/Centers for Disease Control and Prevention Morbidity and Mortality Weekly Report,67(27), 758-762 Kotter, J. (2012). Leading change. Brighton, MA: Harvard Business Lee, J.J., Sobieraj, D.M., & Kuti, E.L. (2010). Student measurement of blood pressure using a simulator arm compared with a live subject s arm. American Journal of Pharmaceutical Education, 74(5), 1-4. doi 10.5688/aj740582
REFERENCES Meng, L., Hou, D., Zhao, X., Hu, Y., Liang, Y., Liu, J., Yan, Y., & Mi, J. (2015). Cardiovascular target organ damage could have been detected in pediatric hypertension. Blood Pressure, 24 doi: 10.3109/08037051.2015.1049424 Pereira, B.C., Nascimento, M.G., Lima, R.S., Rezende Dazio, E.M., & Coelho Leite Fava, S.M. (2018). Knowledge and skills about measuring blood pressure among nursing undergraduate students. Care is Critical, 10(3), 729-736.doi: 10.9789/2175- 5361.2018.v10i3.729-736 Seybert, A.L. & Barton, C.M. (2007). Simulation-based learning to teach blood pressure assessment to doctor of pharmacy students. American Journal of Pharmaceutical Education, 71 doi: 10.5688/aj710348 Vasilevska-Ristovska, J., Hudes,S.Z., Naguleswaran, K. Langlois, V., Matsuda-Abedini, M. & Parekh, R.S. (2018). Pediatric hypertension: Impact on the heart, brain, kidney, and retina. Current Cardiovascular Risk Reports,12. doi: org/10.1007/s12170-018-0577-6