Improving HIV Cascade Among Injecting Drug Users in Ukraine
Ukraine faces challenges in HIV cascade among injecting drug users, with improved behavioral surveys suggesting positive outcomes. Findings indicate increased linkage to care and treatment uptake, highlighting the need for targeted interventions in this key population.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
National bio National bio- -behavioral surveys suggest behavioral surveys suggest improvement in HIV cascade among people who improvement in HIV cascade among people who inject drugs in Ukraine inject drugs in Ukraine Olga Varetska, Alliance for Public Health @TwitterHandle Share your thoughts on this presentation with #IAS2019 #IAS2019 Share your thoughts on this presentation with
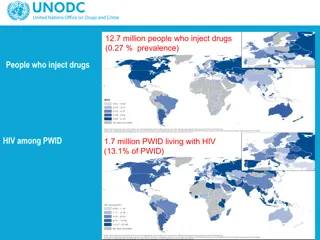
Background Background Ukraine is a country in Eastern Europe with estimated HIV prevalence of 0.6% among adults HIV epidemic was initially driven by PWID, who have the highest prevalence among key populations (22.6% in 2017) PWID constitute almost half of estimated number of PLHIV and account for 75% of new HIV cases in Ukraine Estimated number of HIV-positive PWID in Ukraine is 79,168. During 2011 2017 significant scale-up of community-based services for PWID that were shown to improve access to ART in other settings occurred in Ukraine: harm reduction coverage increased from 157,011 in 2011 to 226,467 in 2017, and case management for HIV-positive PWID from 0 to 8459.
Effectiveness of case management in linking HIV Effectiveness of case management in linking HIV- - positive PWID to care, program data 201 positive PWID to care, program data 2017 7 Standard of care Case management 5000 4736 1000 4500 41% 928 67% 900 4000 800 3500 700 29% 3000 2800 600 2500 500 53% 1998 2000 400 306 1500 300 1000 200 145 100 500 0 0 PWID who received positive results of rapid tests PWID registered in care PWID who started ART PWID who received positive results of rapid tests PWID registered in care PWID who started ART
Methods Methods Secondary analysis of 2011 and 2017 integrated bio-behavioral surveillance (IBBS) data collected in all 27 regions of Ukraine using respondent-driven sampling (RDS) Results of rapid HIV testing and self-reported data on HIV status awareness and enrollment into HIV care and treatment were used to construct the HIV services cascades (RDS weights not used) Chi-square test was used to determine significance of differences between the two years
Results Results In 2017, 10,076 PWID were recruited (18% females) and 21.1% tested positive for HIV. In 2011, 9,069 PWID were recruited (28% females) and 21.9% tested HIV-positive Between the two years, among those who tested positive for HIV: linkage to HIV care increased from 47% (95%CI 44.56% 49.50%) to 52% (50.18% 54.43%), and treatment uptake from 18% (15.75%-19.52%) to 38% (36.34% 40.48%) Awareness of HIV status remained stable
HIV Care Cascade among PWID in Ukraine, IBBS 2011 HIV Care Cascade among PWID in Ukraine, IBBS 2011 - - 2017 2017 70% (1) PWID aware of HIV status : percentage of PWID who reported about HIV-positive status during the interview (among those who responded about previous HIV testing experience and tested positive), IBBS 2017. 60% 58% 56% 52% 50% 47% 38% 40% (2) PWID In HIV care : percentage of PWID who reported about registration at AIDS clinic as HIV-positive person (among those who responded about previous HIV testing experience and tested positive), IBBS 2015 30% 18% 20% (3) PWID receive ART : percentage of PWID who reported about current ART intake (among those who responded about previous HIV testing experience and tested positive), IBBS 2017 10% 0% (1) PWID aware of HIV status (2) PWID In HIV care (3) PWID receive ART 2011 2015
Conclusions Conclusions Enrollment into HIV care and ART coverage among HIV-positive PWID in Ukraine significantly improved from 2011 to 2017 Nevertheless, considerable gaps exist in the cascade, mainly in HIV status awareness and access to ART among those in care Services such as case management are important interventions that may further improve access to treatment for PWID IBBS may serve as a valuable source of data to analyze HIV service cascade outcomes for key populations
Acknowledgements Acknowledgements National HIV prevention program among PWID and case management intervention for PWID (CITI) implemented by Alliance for Public Health and supported by Global Fund and PEPFAR Co-authors: Kostyantyn Dumchev, Olga Varetska, Yana Sazonova, Pavlo Smyrnov