Insights into Perioperative COVID-19 Impact on Surgical Outcomes
This study delves into the impact of perioperative SARS-CoV-2 infection on surgical outcomes, focusing on 30-day mortality rates and pulmonary complications. Key findings include associations with demographic factors, surgery type, and postoperative pathways, providing valuable insights for healthcare providers.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Covidsurg publications Claire Newton Consultant Gynaecological Oncologist
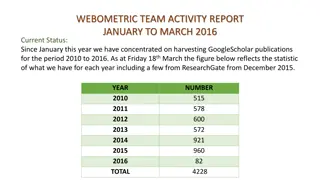
Lancet 2020; 396: 2738 reports 30-day mortality and pulmonary complication rates in patients with perioperative SARS-CoV-2 infection 235 hospitals in 24 countries had SARS-CoV-2 infection confirmed within 7 days before or 30 days after surgery 1128 patients who had surgery between Jan 1 and March 31, 2020. 835 (74 0%) had emergency surgery and 280 (24 8%) had elective surgery.
30-day mortality was 238% (268 of 1128). Pulmonary complications occurred in 577 (51 2%) of 1128 patients; 30-day mortality in these patients was 38 0% (219 of 577), accounting for 81 7% (219 of 268) of all deaths. In adjusted analyses, 30-day mortality was associated with male sex (odds ratio 1 75 [95% CI 1 28 2 40],p<0 0001), age 70 years or older versus younger than 70 years (2 30 [1 65 3 22], p<0 0001), American Society of Anesthesiologists grades 3 5 versus grades 1 2 (2 35 [1 57 3 53], p<0 0001), malignant versus benign or obstetric diagnosis (1 55 [1 01 2 39], p=0 046), emergency versus elective surgery (1 67 [1 06 2 63], p=0 026), major versus minor surgery (1 52 [1 01 2 31], p=0 047).
J Clin Oncol. 2020 Oct 6:JCO2001933. doi: 10.1200/JCO.20.01933.J Clin Oncol. 2020. PMID: 33021869 Aim: determine whether COVID-19 free surgical pathways were associated with lower postoperative pulmonary complication rates compared with hospitals with no defined pathway. 9,171 patients from 447 hospitals in 55 countries 2481 (27.1%) COVID-free vs 6690 (72.9%) patients no defined pathway 10 solid tumour types
Younger and less comorbidities in COVID-free pathway pulmonary complication rates were lower with COVID-19 free surgical pathways (2.2% v 4.9%; adjusted odds ratio [aOR], 0.62; 95% CI, 0.44 to 0.86). The postoperative SARS-CoV-2 infection rate was also lower in COVID-19 free surgical pathways (2.1% v 3.6%; aOR, 0.53; 95% CI, 0.36 to 0.76).