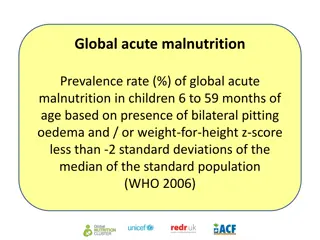
Integrated Management of Acute Malnutrition in Kenya
Explore the comprehensive approach to managing moderate acute malnutrition in Kenya by enabling health workers to follow standard protocols. Learn about the overall objective, learning objectives, health facility requirements, and steps to admission in a supplementary feeding program.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Republic of Kenya Ministry of Health INTEGRATED MANAGEMENT OF ACUTE MALNUTRITION Management of moderate Acute Malnutrition
ACKNOWLEDGMENT MINISTRY OF PUBLIC HEALTH MINISTRY OF MEDICAL SERVICES
OVERALLOBJECTIVE Enable health workers to manage Moderate Acute Malnutrition (MAM) as per standard protocols
LEARNING OBJECTIVES By the end of this session participants should be able to: State the aim of Management of Moderate Acute Malnutrition Identify patients affected by moderate acute malnutrition Manage moderate acute malnutrition applying standard protocols Know the requirements and procedure in setting up a programme to manage moderate acute malnutrition
HEALTHFACILITYREQUIREMENTS Supplementary Feeding Programme Health worker trained in MAM Capacity to conduct assessments, monitoring, and treatment services for patients with moderate acute malnutrition, every two weeks Medical and anthropometric equipment Routine medicines including antibiotics, antihelminths. SFP admission card, SFP registers, and monthly reporting forms. An adequate supply of ready-to-use
STEPSTO ADMISSIONINA SUPPLEMENTARY FEEDING PROGRAMME Step 1: Initial Screening and Referral Step 2: Conduct a medical assessment to identify individuals with emergency signs and immediately transfer to a qualified health worker for treatment Step 3: If no emergency signs are found, then conduct a medical assessment to determine if the child has any priority signs and transfer to a qualified health worker for treatment. Step 4: Nutritional Screening at the Health Facility or Outreach Site for Non-Urgent Cases
STEPSTO ADMISSIONINA SUPPLEMENTARY FEEDING PROGRAMME Step 5: Conduct a medical assessment consisting of a medical history and physical examination Step 6: Conduct Appetite Test if the individual has severe acute malnutrition Step 7: Identify underlying cause of acute malnutrition Based on the above medical, nutrition and causal assessment, determine the management of the individual. If an individual has moderate acute malnutrition according to the following admission criteria then admit to a supplementary feeding programme and follow the treatment protocols in this section.
ADMISSIONAND DISCHARGE CRITERIA Admission Discharge Children 6-59 months with MAM CURED For those admitted based on WHZ, greater than -2 Z score for 2 consecutive visits and a minimum 2 months treatment since admission or For those admitted based on MUAC, MUAC greater than or equal to 12.5cm for 2 consecutive visits and minimum 2 months treatment since admission Children discharged from therapeutic feeding should stay in the SFP for a minimum of 2 months. Individuals should NOT remain in SFP for longer than 4 months. Died died while in treatment Defaulter absent for 3 consecutive visits Non-Response discharge criteria within 4 months WHZ Greater than or equal to 3 z-score to less than -2 z-scores or MUAC 11.5cm to 12.4cm and Appetite, clinically well, alert also Children discharged from OTP. These children are admitted anthropometric status and discharged after 2 months in the programme, assuming their nutritional status does not deteriorate. Children with MAM based on MUAC or WFH who also have bilateral edema should be referred for treatment of SAM rather than into a targeted SFP. Children with MAM with severe medical complications should be referred for immediate medical care. regardless of does not reach
ADMISSIONAND DISCHARGE CRITERIA Admission Pregnant women MUAC 16 to 20.9 at any stage of confirmed pregnancy Lactating women with infant < 6 months MUAC 16 to 20.9 cm Discharge Pregnant women MUAC 23 cm OR If a pregnant woman does not reach MUAC 23 cm before delivery she automatically graduates lactating women program. Postpartum lactating women Discharged when their infant reaches 6 months of age When the infant reaches 6 months of age, the mother should be reassessed for admission to nutrition program based on adult criteria. The infant at 6 months should be assessed for MAM and SAM and referred as appropriate. Pregnant and lactating women to the
ADMISSIONAND DISCHARGE CRITERIA Admission Older Children 5 9 years of age WHZ -3 Z score and < -2 Z score Discharge BMI for age BMI for age WHZ -2 Z score BMI for age WHZ -2 Z score Adolescents 10 17 years of age BMI for age WHZ -3 Z score and < -2 Z score Adults 18 years BMI greater than or equal to 16 and less than 17 BMI greater equal to 18.5 BMI 18.5 MUAC 23.3 cm >22 than or Adults HIV/AIDS living with BMI 16 to 17 MUAC 16 to 18.4 cm Pregnant Lactating living with HIV/AIDS Older persons 60 years of age and MUAC 19 21.9 cm women MUAC 18.5 to <21 cm And if an individual presents with the following then do not keep them in the SFP but refer to the nearest health facility for medical assessment and care Bilateral edema Acute episode of inability to stand/immobile Extreme weakness or dehydration Anorexia MUAC 21 cm
REGISTRATION New Admissions Patients who come spontaneously to the health facility because of another illness (such as diarrhea, pneumonia, malaria, etc.) and meet the criteria for MAM. Patients referred by a health center or private practitioner because they fulfil the criteria of MAM NEW admissions; Registered with a unique nutrition registration number (that they will keep throughout MAM treatment
REGISTRATION Admissions registered in the SFP register as follows: New Cases WHZ if the patient was admitted due to a WHZ , MUAC if the child was admitted due to a MUAC Relapse: a cured child readmitted for a second episode of MAM within 2 months of discharge Transfer from out-patient therapeutic care Old Cases Internal transfer from another SFP Old Cases Readmissions / Returned Defaulters Old Cases
REGISTRATION Old cases: Retain the unique nutrition registration number that they received on their original admission A copy of the transfer form (and a phone call if possible) should have been sent with the individual Re-measure the MUAC, weight and height. Take a brief history concentrating on the complaints, symptoms and signs
OTHERTASKS Register child for admission in the register book MOH 410A or MOH 410B Provide the caregiver with advice/counselling on medical and dietary treatment and progress Provide the patient with an SFP ration card Give routine medications Give a 2 week supply of supplementary food Link the caregiver to the community health worker (CHW) that covers his/her community Ask caretaker to return to the health facility or SFP outreach site for follow-up Refer for Provider Initiated Testing and Counseling for HIV/TB
MANAGEMENT OF CHILDREN WITH ACUTE MALNUTRITION & INFECTED WITH HIV Children with MAM who are diagnosed with HIV and qualify for lifelong ART should be started on ART as soon as possible. HIV infected children with MAM should receive the same ART regimen, in the same dose, as children with HIV and no MAM. HIV infected children with MAM starting ART should be closely monitored in the first 12 weeks. HIV infected children with MAM should be managed with the same therapeutic feeds and same micronutrient supplementation as children who are HIV Negative. Prophylaxis with co-trimoxazole (septrin) should continue throughout the management of MAM. Children with HIV infection are at increased risk of TB and this should be actively sought out for diagnosis and treatment.
COMPONENTSOFA SUPPLEMENTARY FEEDING PROGRAMME
NUTRITIONSUPPORT Consider local food habits, tastes and preferences when determining food rations and designing the food basket Food basket: cereal, pulses, oil and sometimes sugar Provides 1000 to 1200 Kcal per person per day; 35 to 45 grams of protein (12%); and 34 to 45 grams of fat (30%
NUTRITION SUPPORT Dry rations/premixes - Fortified blended foods (FBF) such as Corn Soy Blend (CSB), Wheat Soy Blend (WSB), UNIMIX or Super Cereal Plus. These commodities require some additional preparation in the home. Ready to Use Foods (RUF) Ready to Use Supplementary Food (RUSF). RUFs can be eaten directly from the package without any additional preparation
PRINCIPLESOFMAMCOMMODITIES The food contains ALL essential nutrients in adequate amounts to allow for the extra nutritional requirements Nutrients biologically available to children with the altered intestinal function that is associated with MAM All the inorganic compounds used need to be water soluble
PRINCIPLESOFMAMCOMMODITIES Soy and other pulses dehulled prior to grinding - cereal flours with a low level of extraction (to reduce fiber content). Amount of anti-nutrient compounds and naturally occurring toxins, cyanogens, alkaloids or other potentially poisonous or deleterious natural ingredients must be minimized Ingredients known to contain thermo-labile anti- nutrients should be heat treated prior to fortification
GUIDELINESFORTHEUSEOFAPPROVED COMMODITIESIN KENYA Fortified Blended Food (Super Cereal Plus, WSB/CSB/UNIMIX): Super Cereal Plus is the new brand name for Corn Soy Blend (CSB) that is based on maize, and Wheat Soy Blend (WSB), based on wheat Super Cereal Plus is a further improvement of super cereal with minimized fiber content, animal protein, vegetable oil and sugar. Consumed as a porridge or gruel
GUIDELINESFORTHEUSEOFAPPROVED COMMODITIESIN KENYA 2. CSB/WSB/UNIMIX: For a take-home dry ration, prepare a premix by mixing the appropriate ingredients together in a big basin. Avoid distributing separate ingredients for take home rations
GUIDELINESFORTHEUSEOFAPPROVED COMMODITIESIN KENYA CSB/WSB/UNIMIX Quantities Quantities per child 6 to 59 months old (kg) for a 14 day ration Food items CSB/WSB/UNIMIX 3.5 Vegetable oil 0.35 Total 3.85
GUIDELINESFORTHEUSEOFAPPROVED COMMODITIESIN KENYA Ready to Use Supplementary Foods (RUSFs): Suitable for children exiting therapeutic programmes in order to prevent their relapse to severe acute malnutrition Can be used in both emergency and transitional phases Pre-cooked, does not require preparation or dilution with water.
GUIDELINESFORTHEUSEOFAPPROVED COMMODITIESIN KENYA Ready to Use Supplementary Foods quantities Quantities per child 6 to 59 months old (sachet)14 day ration Food items Ready to Use Supplementary Food (RUSF) 14 Total RUSF 14
HANDOUT 5B: DEMONSTRATION Preparation of premix Preparation of porridge 1. 2.
SUMMARYOFROUTINEMEDICALTREATMENT FORCHILDREN, ADOLESCENTSANDADULTS Name of Medication When Age <1 year Prescription Do not give Dose 1/2 tab on admission 1 tab on admission 1 2 years 200mg Albendazole At admission >2years 400 mg OR <1 year Do not give Mebendazole* At admission Single dose on admission Daily dose from 6 to 12 months of age Daily dose Daily dose Daily dose 1 year and above 500mg 12.5mg iron/50 g folic acid 20-30mg 30-60mg 6 to 24 months (low birth weight & infants) Iron /folate** At admission 2 to 5 years 6 to 11 years Adolescents & adults 60mg Measles vaccination At admission 9 months Once
VITAMIN A Children 6-59 months: Supplementation status should be checked on admission. Give on admission if the child has not received vitamin A in the past 30 days A child showing clinical signs of vitamin A deficiency should be referred immediately to the nearest health facility for treatment Breastfeeding women: a single dose of 200 000IU Vitamin A within first 4 weeks postpartum
DE-WORMING Children 12-59 months: Treat all children 12-59 months routinely for worm infections with Pregnant women :Treat for worm infections during second trimester not first trimester to avoid teratogenicity (gross fetal malformation) Individuals discharged from (therapeutic feeding programs): Not needed. Dosages can be repeated after 3 months
MEASLESVACCINATION All children at 9months should be vaccinated with measles and incase of an outbreak up to 15yrs receive the same
IRONANDFOLICACID On admission for individuals six months and greater, and then administered as a daily dose for 14 days. Given where malaria can be treated effectively Examine for anemia, especially in areas with high malaria prevalence and highand high worm infestation
MEDICALPROBLEMS Anemia: Refer to health facility and Treat according to the IMCI guifdelines (e.g. daily dose of iron sulphate). Malaria: If the initial test is positive, treatment under observation on admission. If beneficiary shows signs of severe malaria, refer to an inpatient facility. Diarrhea: Daily supplement of zinc for 10 days for children with acute diarrhea and dehydration should be prevented and beneficiaries treated with oral rehydration solution as per routine IMCI protocols.
SUMMARYOFROUTINEMEDICALTREATMENT FORPREGNANTANDLACTATINGMOTHERS Name of When Physiological Prescription Dose Product status Within first 4 weeks after delivery Vitamin A Post-partum 200,000 IU Single dose on admission Mebendaz ole Second trimester Single dose Pregnant 500mg Iron/ Folic acid During pregnancy and 60mg iron/400 g folic Daily dose On admission lactation acid
KEY MESSAGESON ADMISSIONTO SFP AND NUTRITION COUNSELLING Rations are provided for the target client The patient or caregiver must receive adequate information about the cause of their malnutrition, and how to avoid a relapse Some patients may require both nutrition counselling and food rations. Ensure that they receive both Explain the expected progress from the child and likewise the adult patient
KEY MESSAGESON ADMISSIONTO SFP AND NUTRITION COUNSELLING After counselling, ask caregiver or adult patient to explain what they will do at home Explain to the patient or caregiver that a CHW is likely to visit his/her home for follow-up Make an appointment with the caregiver or patient for follow-up Carefully explain what will happen at the next visit Ask the adult patient or caregiver to refer others. with similar problems to the health facility. Conduct a cooking demonstration for those taking blended foods
During follow-up visits the below actions should be done: Take Weight Take Height (after one month for children) Take MUAC Calculate W/H and check progress towards target weight Do medical examination Give applicable routine medication/supplementation as Provide nutrition counseling
DATA COLLECTIONAND REPORTING SFP ration cards inserted into the Mother and Child Health Booklets should be used to record all information related to MAM treatment The card s information is similar to the health facility register The cards are presented at each health facility visit and shown to the CHW when visiting a patient s home. Counsel caregivers to ensure that the cards are kept in good condition
WHERETHEREISNO SFP Counsel on selection and use of locally available foods to meet the nutritional needs of children with moderate acute malnutrition by emphasizing on feeding frequency hygienic preparation to ensure age appropriate complementary feeding
CRITERIAFORFAILURETORESPONDTO TREATMENT Either no or trivial weight gain after 5 weeks in the program or at the 3rd visit Any weight loss by the 3rd week in the program or at the 2nd visit Failure to reach discharge criteria after 3 months in the program Abandonment of the program (defaulting) No weight gain after 6 weeks in the program Weight loss exceeding 5% of body weight at any time
REASONSFORFAILURETORESPOND Problems with the application of the protocol: this should be addressed first Nutritional deficiencies that are not being corrected by the diet supplied in the SFP Home/ Social circumstances of the patient An underlying physical condition/ illness Other causes
PROCEDURETOADDRESSFAILURETO RESPOND Protocol problems:proper application of the protocol and the training of the staff at field level should be systematically reviewed, if possible by external evaluation Uncorrected nutritional deficiencies Social problems: sharing of rations, child abuse, sibling rivalry, povery, discrimination Underlying medical conditions/ other conditions
STEPSTOBETAKENFORCHILDRENTHAT FAILTORESPONDTOTREATMENT Failure to respond to treatment 1. Check the application of the protocol 2. Change the diet to check for uncorrected nutritional 3. Check for problems with home environment/ social problems 4. Admit for full clinical assessment to search for underlying undiagnosed pathology 5. Refer to a health facility with diagnostic facilities & senior paediatric personnel for assessment & further management of the case
TREATMENTFOR FAILURETO RESPOND One at a time in the sequence shown above Substitute the current supplementary commodity used for this individual with a superior commodity (either super cereal plus or RUSF) for 14 days After 14 days: If he/she now responds to treatment, continue the treatment with the superior commodity for the remainder of the treatment for this individual in the SFP.
TREATMENTFOR FAILURETO RESPOND If he/she does not respond to treatment, this means that the dominant problem is NOT A NUTRITIONAL problem and that now investigation for a social issue should be started
TREATMENTFOR FAILURETO RESPOND During the home visit, if a problem is identified that can be alleviated or solved: Deal with the problem, leave the child at home for follow up and further visits can be made the next weeks. If they identified a problem that cannot be alleviated or solved at home: Take any steps necessary to alleviate the problem such as 1) admission of the child to a health facility ETC
TREATMENTFOR FAILURETO RESPOND If no problem is identified to account for the failure to respond to treatment, then it is still likely that there is a social problem that has not been identified during the home visit Admit the child for a trial of feeding for 3 days with feeds under supervision in an in-patient in a health facility or a day-care center to receive food under supervision If still the child is not responding to treatment, refer to hospital have the facilities to investigate
DISCHARGE CRITERIA Cured: Individual that has reached the discharge criteria defined for the programme Death: Individual that died from any cause while registered in the programme. Defaulter: Individual that is absent for 3 consecutive service or programme rounds. Home visit is arranged in order to determine the reason and encourage participation in the SFP. Non-response: Individual who has not reached discharge criteria after a 4 months despite all investigations and transfer options