Investigation of Suspected Acute Pulmonary Thromboembolism
This case study presents a 48-year-old male with a history of COPD who developed sudden chest pain and shortness of breath. Through detailed examination and tests, the possibility of acute pulmonary thromboembolism (PTE) is being considered along with differential diagnosis. The importance of investigating and ruling out PTE in such cases is highlighted, and various diagnostic tools such as ultrasound, echocardiography, troponin assay, D-dimer assay, and CTPA are discussed.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Investigation of suspected acute pulmonary thromboembolism (PTE) Internal Medicine Society of Australia and New Zealand
Hugh Patient medical history (PMHx) 48-year-old male plumber ex-smoker (1 pack of cigarettes per day for 10 years) having ceased 6 months previously mild chronic obstructive pulmonary disease (COPD) medications; regular Spiriva inhaler and Ventolin inhaler as required no recent illnesses, weight loss, calf pain or long-haul plane flights Symptoms 10 days ago he developed a bad head cold with runny nose and sore throat, followed by onset of a hacking cough productive of purulent sputum and shortness of breath on exertion. After 4 days, he went to his GP and was prescribed antibiotics. His symptoms were improving until today when he suddenly developed sharp pleuritic chest pain adjacent to his left mid-sternum and worsening shortness of breath. Because the pain was severe and he was unable to go to work, he took himself to the local hospital ED for assessment
Hugh Examination no fever pulse rate (PR) 60 bpm blood pressure (BP) 140/80 lying supine position, 125/70 standing normal heart sounds with no murmurs scattered coarse inspiratory crackles and mild expiratory wheeze heard over all lung zones with no friction rub marked tenderness over the left 4th anterior costochondral joint abdominal and neurological examinations are normal no calf swelling or tenderness Tests / Investigations full blood count and 20-item biochemical profile normal electrocardiograph normal chest X-ray shows mild hyperinflation of both lungs with no other focal abnormalities pulse oximetry shows normal arterial oxygen saturation of 96% on room air.
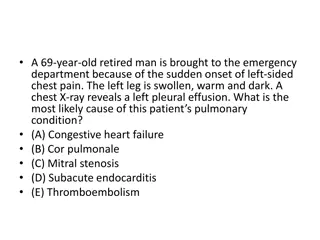
What is the diagnosis? Viral or cough-induced costochondritis? Acute pulmonary thromboembolism (PTE) with clots passing to his lungs? Need to rule out acute pulmonary thromboembolism (PTE) due to severity of the condition.
What investigations can be used for suspected acute pulmonary thromboembolism? Duplex ultrasound of the lower limb veins Imaging test used to demonstrate venous thrombi which, if located in the deep venous system, can embolise to the lungs. Echocardiography Imaging test to assess right ventricular function and measure right heart pressures in acute PTE. Serum troponin assay Blood test to detect elevated troponin levels resulting from right heart strain in acute PTE or myocardial ischaemia resulting from decreased cardiac output in massive or sub-massive PTE. D-dimer assay Highly sensitive test to detect breakdown products of venous thrombi in the bloodstream. Computerised tomography pulmonary arteries (CTPA) Imaging test requiring contrast infusion which can detect embolised thrombi in pulmonary arteries in patients with suspected PTE.
Which investigations are recommended in this case of suspected acute pulmonary thromboembolism (PTE)? Duplex ultrasound of the lower limb veins Echocardiography Serum troponin assay D-dimer assay Computerised tomography pulmonary arteries (CTPA)
Use a validated prediction tool such as the modified Wells score to guide choice of investigation. Modified Wells score includes variables such as symptoms and signs of DVT and heart rate >100 bpm, where a score < 4 makes acute PTE unlikely. For Hugh, the modified Wells score is 0. This indicates low pre-test probability of acute PTE. As a result, the recommendation for investigation for Hugh is: o Duplex ultrasound of the lower limb veins o Echocardiography o Serum troponin assay o D-dimer assay o Computerised tomography pulmonary arteries (CTPA)
Correct steps for management D-dimer assay yields a result of 300 ng/ml which, for Hugh, is below upper normal age- adjusted reference value (or cut-point) of 550 ng/ml. This result renders the probability of acute PTE < 1% (ie very unlikely). No further investigations for acute PTE are recommended for Hugh. History and examination suggests costochondritis induced by prolonged coughing or viral infection as the most likely cause for Hugh s presentation. Hugh is treated with: analgesics 2. local anaesthetic injection to his costochondral joint 3. discharged from ED with follow-up from his GP. 1.
Evolve Recommendation Don t request computerised tomography pulmonary angiography (CTPA) as the first-choice investigation in patients with low risk of venous thromboembolism (VTE) by modified Wells score. Instead request D-dimer and perform imaging only if levels are elevated, after adjusting for age Internal Medicine Society of Australia and New Zealand Evolve is facilitated by the Royal Australasian College of Physicians
What is best practice? The modified Wells score (see adjacent table) is a validated prediction rule for estimating pre-test probability of DVT or acute PTE. A low score (< 4) equates to a low (< 10%) probability of DVT or PTE. Modified Wells score Feature Clinical signs and symptoms of DVT PTE most likely diagnosis Heart rate >100 beats per minute Immobilisation at least three days or surgery within past four weeks Previous DVT or PTE Haemoptysis Malignancy treatment within six months or palliative 1 Points 3 3 The quantitative D-dimer assay is highly sensitive for DVT and acute PTE, such that a negative result (ie value below the upper normal reference value, after adjusting for age*) effectively rules out this condition in patients with low pre-test probability, as determined by the modified Wells score. 1.5 1.5 1.5 1 *Adjustment for age: for patients over age 50, upper normal reference value for the assay is multiplied by age/100 In patients with modified Wells score < 4, D-dimer assay should be the first-choice investigation rather than CTPA or duplex venous ultrasound Total score is summation of all points assigned according to the presence of each feature listed
What is best practice? Unnecessary use of CTPA has negative consequences of: contrast allergy radiation exposure identification of benign incidentalomas that may provoke further invasive investigations identification of isolated small sub-segmental emboli that do not account for the clinical presentation and whose natural history is unknown, but which may lead to commencement of anticoagulation which has not been shown to be of any benefit in such cases, and instead imposes risk of major bleeding unnecessary cost unnecessary delays in discharging very low risk patients from congested EDs
How this case study was made This case study was developed through the RACP Evolve initiative by Professor Ian Scott. This case study has been reviewed by RACP, NPS MedicineWise and the Internal Medicine Society of Australia and New Zealand. This case study was approved for publication by the Internal Medicine Society of Australia and New Zealand in December 2019.
Evaluation How likely is this Evolve recommendation to change your practice? 1. Not at all 2. Somewhat 3. Significantly Explain your reasoning
About Evolve As part of a global movement, Evolve is a flagship initiative led by physicians, specialties and the Royal Australasian College of Physicians (RACP) to drive high-value, high-quality care in Australia and New Zealand. Evolve aims to reduce low-value care by supporting physicians to: be leaders in changing clinical behaviour for better patient care make better decisions, and make better use of resources. Find out more: www.evolve.edu.au Get in touch: evolve@racp.edu.au