Legal Responsibilities of Professions: Child-Friendly Law
Explore the legal intricacies regarding autonomy, consent, and refusal in professional responsibilities, specifically related to children. Delve into key issues, interpretations of landmark cases like Gillick v. Norfolk, and the balance between autonomy and welfare in decision-making for minors within the healthcare system.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
The Legal Responsibilities of the Professions: is the law child or professional friendly? Jonathan Montgomery 18 June 2015
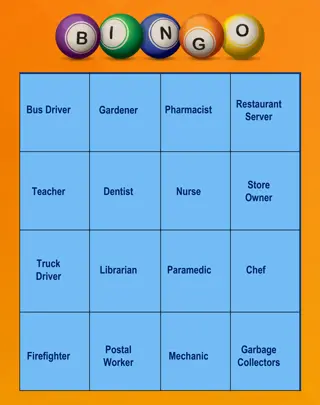
Key Issues Autonomy, Consent and refusal Beyond consent Participation and partnership Acceptable & good practice Nature and function of judicial oversight Construction of parental and professional power Judicial expectations of medical ethics Integration rather than opposition
Interpreting Gillick P. Alderson & J. Montgomery Health Care Choices: Making decisions with children (IPPR 1996). Gillick v W Norfolk & Wisbech HA [1986] 1 AC 112 as promising young people Welfare, and also Autonomy UN Convention on the Rights of the Child Autonomy & participation
Retreat from Gillick? Donaldson: denying autonomy, reinforcing welfare Consent but not refusal Fragility autonomy rights dependent on competence Weakness liable to be overridden by parents or court Re R [1991] 4 All ER 177 Re W [1992] 4 All ER 627 Tail wagging dog problem
Autonomy, Consent and refusal The logic of concurrent consent givers Withholding consent is not the same as a right to refuse Licence to treat Doctor rather than patient focus? English law is more concerned with the duties of doctors than the rights of patients But are rights more than a conglomeration of duties anyway? Rights in law generate duties in order to protect interests Parental rights exist to promote their children s interests Professionals have power, clinical freedom and responsibilities for the same reason
No one can dictate the treatment to be given to any child, neither court, parents nor doctors. . . The doctors can recommend treatment A in preference to treatment B. They can also refuse to adopt treatment C on the grounds that it is medically contra-indicated or for some other reason is a treatment which they could not conscientiously administer. The court or parents for their part can refuse to consent to treatment A or B or both, but cannot insist on treatment C. The inevitable and desirable result is that choice of treatment is in some measure a joint decision of the doctors and the court or parents. Re J [1991] 3 All ER 930, 934
If the parents disagree, one consenting and the other refusing, the doctor will be presented with a professional and ethical, but not with a legal, problem because, if he has the consent of one authorised person, treatment will not without more constitute a trespass or a criminal assault. Re R [1991] 4 All ER 177
A key test area: is intolerability the touchstone of best interests in withdrawal of treatment cases? (Hidden Lawmakers [2014] MLR p 367-9) Burke v GMC [2004] EWHC (Admin) 1879 (Munby J); [2005] EWCA Civ 1003 Portsmouth v Wyatt [2004] EWHC 2247 (Fam) (Hedley J) Aintree v James [2013] UKSC 67, [36]-[39] Re SE (Moor J) [2014] EWHC 3182 (Fam). Rules or discretion? Law or ethics?
Losing the friendly judicial licence to exercise power conscientiously Misleading children and families Montgomery v Lanarkshire [2015] Re T Misalignment of purposes? Mistakes of fact and logic Bolitho v Haringey HA Vitalist decisions not respected in best interests framework Courts grappling with this
Re S [1994] 2 FLR 1065 that for her to submit to further transfusions would have consequences for her in the life hereafter and it is for that reason and not because of any wish to die, so-called, that she resists the local authority's application for treatment to be authorised. (1068)
`S seemed to me to be not only small, frail and pale of face, but she seemed to me to be less mature than most girls of her age in the way she spoke, responded to questions and generally conducted herself . `holding her Bible in both her hands as she answered questions, this young woman never wavered in her refusal to have more blood transfusions `[s]he has said on previous occasions that if it was forced upon her it would be like rape .
When I was a child, I spoke as a child.' That seemed to me to be how S feels and speaks. There are those who are children and those who are adults and those who are in-between. I do not believe that S is in-between. She is still very much, in my view, a child. Whilst as she gave evidence I was so very strongly impressed by her integrity and her commitment, I believe they were the integrity and commitment of a child and not of somebody who was competent to make the decision that she tells me she has made. She hopes still for a miracle. My conclusion is, therefore, that she is not `Gillick-competent'.
Re L [1998] 2 FLR 810. Not fully aware of mode of death Had not been told Narrow experience limited understanding Sheltered life (only JW community) Psychiatric evidence on competence
The psychiatrist [made] the point that the girl s view as to having no blood transfusion is based on a very sincerely, strongly held religious belief which does not lend itself in her mind to discussion. It is one that has been formed by her in the context of her own family experience and the Jehovah s Witnesses meetings where they all support this view. He makes the point that there is a distinction between a view of this kind and the constructive formulation of an opinion which occurs with adult experience
An NHS Foundation Hospital v P [2014] EWHC 1650 (Fam) Paracetamol overdose by competent woman of 17 years of age, hospital refused to treat on basis of parental consent this court is under a heavy duty to take what steps it can to protect P's life which is manifestly in danger tonight. Accordingly, I have made an order including a declaration that it is lawful and in P's best interests for the medical practitioners having responsibility for her care and treatment to treat her for the effects of her overdose notwithstanding the fact that she is refusing treatment. Para [16]
D (A Child ; deprivation of liberty), Re [2015] EWHC 922 (Fam), para [60] All professionals involved in his life and in reviewing his care and treatment are agreed that these arrangements are overwhelmingly in D's best interests. On the facts of this case, why on public policy or human rights grounds should these parents be denied the ability to secure the best medical treatment and care for their son? Why should the state interfere in these parents' role to make informed decisions about their son's care and living arrangements?
A (A Child), Re (Rev 1) [2014] EWCOP 920, para [45] . the relationship between the hospital, social services and A has become conflictual. I heard evidence that A requires decision making from an independent 'authority figure'. It quickly became obvious that the figure should be the Judge.
Q The Legal Responsibilities of the Professions: is the law child or professional friendly? A: The law supports professional power (clinical freedom) because if is prefers ethics to law and trusts doctors to be more friendly to children s rights than it does court processes