Legislative Hearing on Eleanor Slater Hospital and Olmstead Decision
Explore the legislative hearing on Eleanor Slater Hospital and the Olmstead Decision, which underscores the rights of individuals with disabilities to community-based supports. Learn about ESH's history, patient demographics, and compliance with regulatory standards like the Americans with Disabilities Act and the Olmstead Decision.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
House Oversight Committee Legislative Hearing regarding Eleanor SlaterHospital Thursday, April 1,2021 Rhode Island Department of Behavioral Healthcare, Developmental Disabilities & Hospitals 1
A Look at Eleanor Slater Hospital Slide Page# Overview of Eleanor Slater Hospital (ESH) System 3 Americans with Disabilities Act (ADA) / Olmstead Decision Consideration 4 The Joint Commission (TJC) Accreditation 5 Discharge Process/Progress 6, 7 8 High-level Summary of the Consultant s Report Planning for the Future 9 Communication at ESH 10 Appendix 11 5-year Census Across ESH Facilities 12 13 Division of Capital Asset Management & Maintenance (DCAMM) Facility Assessments 2
Overview of Eleanor Slater Hospital Eleanor Slater Hospital (ESH) is a long-term acute care hospital (LTACH) that serves patients with complex psychiatric (psych) and medical (med) diagnoses including patients with intellectual and developmental disabilities (I/DD) and traumatic braininjuries A state hospital was established in 1870 and has gone through many iterations. In 1994, four separate facilities were combined to form the Eleanor Slater Hospital. It has been known as the hospital of last resort serving individuals whom, under older models of care, were considered to be patients who could not be served in the community Patients were admitted to ESH through either the forensic system (court mandated) or as a non-forensic admission if, at the time of admission, they could not be served in either a nursing or community-based setting, like a group home Prior to 2020, the hospital has not had robust discharge protocols in place, resulting in long-term to end-of-life stays. As a benchmark, Center for Medicaid and Medicare Services (CMS) guidance estimates a typical length of stay for an LTACH is between 30 and 90 days Campus Building Population PatientCount ESH Average Length of Stay Cranston Benton ForensicPsych 50 ~0-12months Forensic Psych OverflowUnit CivilPsych AdolphMeyer 27 ~12years Civil Psych Med (VentUnit) Regan 39 ~11years Burrillville Zambarano Med 74 ~16years 190/230 licensedbeds (64 Forensic / 126 Non-Forensic) ESHCombined ~13years 3
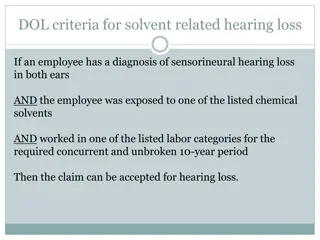
Americans with Disabilities Act (ADA) / Olmstead Decision In 1999, the Supreme Court held in Olmstead that people with disabilities have a right to receive state funded supports and services in the community rather than institutions Olmstead interprets the Americans with Disabilities Act's integration mandate, which requires public entities to administer services, programs, and activities in the most integrated setting appropriate to the needs of the qualified individuals with disabilities The Olmstead decision centered on patients in a psychiatric hospital. Later cases have confirmed that Olmstead applies to all state and Medicaid fundedinstitutions Regulations implementing the Supreme Court s Olmstead decision continue to emphasize the development of community-based alternatives to inpatientcare Once a person no longer needs hospital level of care, the state must work with the person and their support team to discharge to the least restrictive setting that meets their needs and preferences The Olmstead decision reinforces our commitment to ensure patients clinical needs define their care not any other factor. 4
ESH is Accredited by The Joint Commission (TJC) The Joint Commission last surveyed the hospital in September 2017 Findings included approximately 25 deficiencies ranging from causing an Immediate Threat to Life to Low/No Impact/Harm Noteworthy finding: presence of ligature risk compromising safety of psychiatric patients in Adolph Meyer and Regan (Zambarano does not meet building requirements to serve psychiatric patients) Presence of ligature risk is currently remediated through five-minute staff checks; significant capital funding would need to be committed to fully remediate physical deficiencies ESH was given a preliminary notice of denial after which the hospital had 60 days to remediate findings and maintain compliance TJC accredited the hospital retroactive to September 2017 after remediation of findings and further unannounced on-sitesurveys TJC was scheduled to return for its regular three-year accreditation visit in Fall 2020, however, due to COVID, accreditation was postponed; TJC is expected to return imminently (March-April 2021) 5
Discharge Process Historically, there has not been a routine process for assessing level of care and discharging non-forensic patients who no longer needed hospital services Average length of stay > 12 years Most hospitals, including LTACHs, follow industry best practices to be begin discharge planning on day one, in order to align all treatment goals with discharge goals 20192020 2021 Zambrano * 5 0 * 30 4 Adolf Meyer (AM) In 2020, ESH began assessing level of care and meeting with patients to begin discharge planning Level of Care determination is made by a clinician such as a utilization review nurse or physician Regan * 3 3 Benton * 29 10 It is ESH's practice to only discharge people who are willing and have a safe discharge plan. ESH has met and will continue to meet with the Mental Health Advocate, Disability Rights Rhode Island, Alliance for Long Term Care, and other stakeholders for feedback ESH has a contract with the Alliance, to support individuals discharging into a nursing home setting, post ESH Discharge. ESH supports individuals post discharge by ensuring that they have authorization/ access to services post discharge, such as a medication, etc. In late 2020, ESH published a discharge appeals policy, ensuring patients who might disagree with discharge decisions had access to Executive Office of Health and Human Services (EOHHS) due process and appeals rights and we are continuing to refine/update this process based on stakeholder/patient/family feedback. Total Discharges 87 67 17 Deaths 16 19 3 Total Patient Outflow -103 -96 -20 6
Discharge Progress Since July 2020, the hospital has discharged approximately 22 non- forensic patients to home and community-based placements: PatientMortality, 14 Home -2 MHPRR -14 Nursing Home - 1 Assisted Living -2 DD Group Home - 1 Discharged to Community Placement,22 No patient was discharged against their will. For patients that have a guardian, guardians were also in agreement with the discharge. If a patient is deemed competent to make their own decisions, their desire to discharge, when in line with physician recommendation is what is acted upon. Family input is also welcomed and important but ultimately, the patient had the decision-makingauthority. In addition to the 22 discharges (4 from Burrillville and 18 from Cranston), there have been 14 patient mortalities since July 2020. Non-Forensic Patientscurrently at ESH, 127 7
Consultant Proposals Alvarez & Marsal in 2020 delivered a report outlining potential redesign scenarios and their respective financial impact for the State, on which the department testified before the House Finance and Senate Finance Committees last fall. Three scenarios were developed in the report: Scenario #1: Close Zambarano, Regan, Adolph Meyer, license Benton as an independent Forensic Hospital, develop capacity in the community for high acuity patients to be served in the least restrictive settings Scenario #2: Close Regan, Adolph Meyer, license Benton as an independent Forensic Hospital, redefine Zambarano as a mixed-use long-term care facility (not a hospital) for populations that the existing continuum of care does not serve Scenario #3: Maintain Status Quo close Adolph Meyer, maintain Regan, Benton and Zambarano under existing licensure These proposals highlight that regardless of the scenario ultimately pursued, the hospital must engage in active discharge planning per federal guidelines and allow individuals to transition into the most appropriate, least restrictive setting in accordance with Olmstead, the landmark Supreme Court ruling. This is what is best for our patients and their loved ones. 8
Planning for the Future: Addressing the Behavioral Health (BH) Continuum of Care BHDDH recognizes that gaps exist in the current continuum of care that prevent patients from immediately transitioning into a less restrictive setting BHDDH is working with EOHHS/Medicaid to develop the continuum of care to support people in the most appropriate and least restrictive setting Capacity building grants for nursing facilities Enhanced nursing home rates for individuals with high acuity psychiatric needs BHDDH is working with stakeholders to continue to build up the BH Continuum of Care Develop community-based service options for individuals with traumatic brain injuries Enhance capacity with Mental Health Psychiatric Rehabilitative Residence (MHPRR) services to serve individuals with high acuity behavioral health needs 9
Communication re: ESH Since the beginning of my tenure as Director of BHDDH, my team and/or I have had meetings to discuss the ESH Transition and Transformation Plan with many constituencies, using various platforms. To date, there have been: 20 meetings with DOA/HR to seek guidance on moving forward 18 Union Leadership and/or Local Meetings (this includes Council 94, Laborer s International, SEIU, NAGE, UNAP) 15 Medical Staff Meetings 15 Medical Executive Staff Meetings 8 Town Hall Meetings open to all ESH Staff 1 Meeting at Zambarano with the two area legislators and union reps Numerous Meetings with Advocates, Provider Networks and Organizations (such as HARI, Governor s Council on Behavioral Health, Substance Use Mental Health Leadership Council, Long-Term Continuum of Care Council, etc) Legislative Testimony, as well as interviews about our plans in the Providence Business News and on WJAR-10 10
Appendix Additional information related to Eleanor Slater Hospital Redesign and Transition 11
ESH Admissions/DischargeData Admissions Data by PatientType Discharge Data by Year OverallCensus 2019 2020 2019 2020 2021 300 250 200 150 100 50 Medical Admissions Zambrano * 5 0 22 6 AdolfMeyer (AM) * 30 4 Forensic Admissions 96 61 Regan * 3 3 Total Admissions +118 +67 Benton * 29 10 0 2020 2019 2018 2017 2016 Total Discharges 87 67 17 Aggregate Discharges by Patient Type 222 pts 222 pts 222 pts 239 pts 273 pts Deaths 16 19 3 2019 2020 TotalPatient Outflow -103 -96 -20 Medical /Civil Discharges 19 25 3/22/2021 Forensic Discharges 68 42 *only aggregate dataavailable Total Discharges -87 -67 12
Physical Facilities Condition Facility Conditions Assessment performed by EMG Engineering indicates the following: Adolph Meyer (Feb 2019) Overall, the building appeared to be in poor condition Indoor air quality in the building was reported to be very poor. Suspected fungal growth was observed in the building, with the highest concentrations observed in the basement. Given the building s age, asbestos containing materials may exist beyond the items identified in this report. The building has not been well maintained (Source: EMG FCA Report, Feb 2019) Regan (Feb 2019) Overall, the building appeared to be in fair condition. There were issues with water infiltration at the basement level and several isolated instances of finished in poor condition. Isolated ceiling tiles were observed with suspected fungal growth. . . asbestos was reportedly uncovered [in flooring]. . . . Reports indicate that elevators have become unreliable, and need frequent service, resulting in downtime. (Source: EMG FCA Report, Feb 2019) Zambarano (Feb 2019) Overall, the building appeared to be in fair condition. There were several concerns observed of structural, safety, and environmental nature. The exterior wall at the north service elevator was observed to be cracked and bowing, which appears to present some risk of partial collapse. . . Environmental concerns noted include deteriorating finishes with suspected asbestos containing materials, including floor tiles and building piping insulation, as well as paint peeling in stairwells that is suspected of containing lead. (Source: EMG FCA Report, Feb 2019) Report Date / ThirdParty Evaluator CurrentReplacement Value(CRV) Age Condition Adolph MeyerBuilding (CranstonCampus) 80+ Feb 2019 /EMG $76m Poor Regan Building (CranstonCampus) 45+ Feb 2019/EMG $84m Fair Beazley Building (Zambarano Campus) 70+ Feb 2019/EMG $66m Fair 13