Malaria: Causes, Symptoms, and Paroxysms
Malaria is a mosquito-borne infectious disease caused by the Plasmodium parasites. It affects millions worldwide, with symptoms ranging from fever and headache to severe complications like coma and death. Learn about the causes, signs, and stages of this widespread disease.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
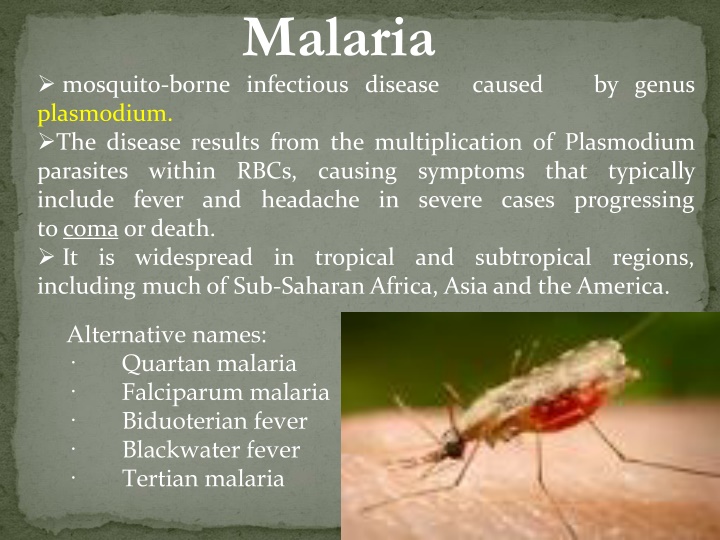
Malaria mosquito-borne infectious disease caused by genus plasmodium. The disease results from the multiplication of Plasmodium parasites within RBCs, causing symptoms that typically include fever and headache in severe cases progressing tocoma ordeath. It is widespread in tropical and subtropical regions, including much of Sub-Saharan Africa, Asia and the America. Alternative names: Quartan malaria Falciparum malaria Biduoterian fever Blackwater fever Tertian malaria
At risk for malaria: 40% of the world s population Commonly associated with poverty more than 500 million are ill of malaria yearly Eliminated from US, Canada, Europe and Russia but has resurged in tropics India has 1.5 million cases/year of malaria(40-50% are due to P.Falciparum)
CAUSES Plasmodium falciparum - most common and deadly type of malaria infection - can lead to cerebral malaria P.vivax - most common -causes relapse if treatment was not completed. P.ovale. P.Malaria
Hypnozoite P.V, M, O PATHOPHYSIOLOGY: Merozoites fever fever
Signs & symptoms: P. falciparum P. vivax P. ovale P. malariae Incubation period (days) Merozoite maturation (days) Merozoites produced 7-14 12-17 16-18 18-40 5-7 6-8 9 12-16 40,000 10,000 15,000 2,000 Sometimesthe incubation periods can be prolonged for several months in P. vivax, P. ovale, and P. malariae. All four species can exhibit non-specific prodromal symptoms a few days before the first febrile attack. These prodromal symptoms are generally described as 'flu-like - headache, slight fever, muscle pain, anorexia, nausea and lassitude. The symptoms tend to correlate with increasing numbers of parasites.
These prodromal symptoms will be followed by febrile attacks (malarial paroxysms) The Malarial Paroxysm COLD STAGE HOT STAGE SWEATING STAGE profuse sweating declining temperature exhausted and weak sleep lasts 2-4 hours feeling of intense cold vigorous shivering lasts 15-60 minutes intense heat dry burning skin throbbing headache lasts 2-6 hours The malarial paroxysm will usually last 4-8 hours
The fever paroxysm corresponds to the period of erythrocyte and invasion. infected rupture merozoite
Disease Severity and Duration vivax ovale malariae falciparum Initial Paraoxysm Severity Average Parasitemia (mm3) Maximum Parasitemia (mm3) Symptom Duration (untreated) Maximum Infection Duration (untreated) Anemia Complications moderate to severe moderate to severe mild severe 50,000- 500,000 20,000 9,000 6,000 50,000 30,000 20,000 2,500,000 2-3 weeks 3-8+ weeks 3-24 weeks 2-3 weeks 12-20 months 5-8 years 20-50+ years 6-17 months ++ + ++ renal ++++ cerebral
Uncomplicated Malaria Symptoms: fever, chills, headache, body pains, diarrhea, vomiting, cough Signs: anemia, thrombocytopenia Features of severe malaria Decrease in conscious level, neurological signs or fits Severe anemia Hematocrit < 15% Hyperpyrexia Hyperparasitemia > 5% Hypoglycemia (glucose < 2.2 mmol/L) Renal impairment or oliguria Pulmonary edema, hypoxia, acidosis Circulatory collapse or shock Hemostasis abnormalities hemolysis Hepatomegaly, Splenomegaly, Dehydration.
Diagnosis: Examine blood under microscope (geimsa stain) Thick and thin blood smears are gold standard Identify species and quantify density If can not identify species, treat for P.f. Re-examine smears or use alternative diagnostic tool Suspect P.f. If critically ill If returned from Sub-Saharan Africa, > 95 % chance of P.f. pure or mixed infection Parasitemia > 1% CT scan: to evaluate evidence of cerebral edema or hemorrhage Polymerase chain reaction (PCR) -determine the species of plasmodium Dipstick test (Immunochromatographic tests/Antigen-Capture Assay) - not as effective when parasite levels are below 100 parasites/mL of blood
Principles of management of malaria Prompt and accurate diagnosis Assess for signs of complicated/severe malaria Prompt use of appropriate antimalarial drugs Monitor clinical and parasitological improvement Cure parasitic and/or clinical Ancillary treatment Instructions for future prevention of malaria
The Anti-malarial Drugs Artesunate, Artether, Artemether Mefloquine, Amodiaquine Quinine, Chloroquine Lumefantrine, Halofantrine, Proguanilchlor (chlorguanide) Sulfadoxin+Pyrimethmine, Dapsone Tetracyclines, Doxycyclin, Clindamycin
Malaria Treatment non-falciparuminfections Chloroquine (CQ) is the drug of choice Pruritis is major side effect of CQ More common in dark-skinned people Can offer antihistamines, continue use Some CQ-resistant P. vivax has been reported from Oceania and South America Mefloquine or quinine for proven resistant cases
Complications of falciparum malaria Each cycle releases 20 times more merozoites than vivax Coma - cerebral malaria, convulsions Renal failure black water fever Hyperpyrexia, acute pulmonary edema Hemolytic Jaundice, severe bleeding Hypovolemic shock, Hypoglycemia Metabolic acidosis, Coagulopathy, Severe anaemia, hyperparasitemia Usually resistant to Chloroquine
Drug Rx. of falciparum Chloroquine is not the drug of choice Should not be treated with single drug Combination therapy is a must Combination therapy is a must Artemisinin based CT ACT is the Rx. of choice
Combination Therapy (CT) Anti-malarial combination therapy (CT) is the simultaneous use of two or more blood schizonticidal drugs with different biochemical targets in the parasites and independent modes of action. Artemisinin Artemisinin based based Combination Combination Therapy Therapy (ACT) (ACT) Artemisinin-based combination therapy (ACT) is an antimalarial combination therapy with an artemisinin derivative as one component of the combination given for at least 3 days.
Rationale for ACT Resistance to Chloroquine and SP Protect individual drug from resistance To decrease rate of decline in efficacy To interrupt spread of resistant strains To decrease transmission in a region The combination is often more effective In the rare event of resistance to one of the drugs during the course of the infection, the parasite will be killed by the other drug
Why Artemisinins ? Short half-life; hence good for combination Rapid substantial reduction of the parasite biomass Rapid resolution of clinical symptoms Effective action against multi-drug resistant P. falciparum Reduction of gametocyte carriage No documented parasite resistance yet Few reported adverse effects.
Artemether-Lumefantrine-AL (Coartem, Lumether, Riamet) 6 dose regimen of Lumether (20-120mg)
Artesunate + Mefloquine AS + MQ
Artesunate + Amodiaquine AS + AQ
Second line Combinations Artesunate (7 days) + Tetracycline(100mg) (7) 1. Artesunate (7 days) + Doxycycline(100mg) (7) 2. Artesunate (7 days) + Clindamycin(900mg) (7) 3. or 4. Quinine in place of AS + any of the above antibiotics for 7 days
severe severe falciparum falciparum malaria Chloroquine-resistant malaria or sensitivity not known malaria Artemisininsparenteral Arteether 150 mg (2ml) i.m od x 3 days or 3 mg/kg od i.m. x 3 days Artesunate: 2.4 mg/kg (loading dose) IV, followed by 1.2 mg/kg at 12 and 24 hours, then 1.2 mg/kg daily for 6 days. If the patient is able to swallow, the daily dose can be given orally. Artemether 3.2 mg/kg i.m. given on admission then 1.6 mg/kg per day is an acceptable alternative to quinine i.v infusions Rectal artemisinins are not as effective
Quinine parenteral A loading dose of quinine of 20 mg salt/kg bw. 10 mg/kg 8th hrly i.v infusion followed by - quinine tablets, 10 mg salt/kg, 8-hourly to complete a 7-day course of treatment, or a single dose of 25 mg/kg sulfadoxine and 1.25 mg/kg pyrimethamine (maximum 1500 mg sulfadoxine 75 mg pyrimethamine). Rate-controlled i.v. infusion is the preferred route of quinine admin. If this cannot be given safely, then i.m. injection is a satisfactory alternative. Rectal admin. is not effective Quinidine can substitute quinine
severe severe falciparum falciparum malaria Chloroquine Chloroquine- -sensitive malaria sensitive malaria malaria Chloroquine: 10 mg base/kg over 8 hours, followed by 15 mg/kg given over the next 24 hours. or Chloroquine: 5 mg base/kg over 6 hours, every 6 hours, for a total of 5 doses or (If IV infusion is not possible) chloroquine, 3.5 mg base/kg, every 6 hours IM or SC
Adjunct treatment of uncomplicated malaria Fever Acetominophen, paracetamol Avoid aspirin in kids due to risk of Reyes Syndrome Sponge baths Anemia Transfusion of RBCs may be needed Iron, folic acid Rehydration Solutions with extra glucose
What to give in pregnancy ? In 1st trimester Quinine + Clindamycin 7 days In 2nd and 3rd trimesters Any ACT combination as per rec. or Artesunate + Clindamycin 7 days or Quinine + Clindamycin 7 days Lactating women same ACT
Warning Artemisinins should never be used as monotherapy Artesunate combinations always given for 3 days; never single dose of AS. For AL six doses must be over 3 days AQ or MQ or SP should never be used alone - lest drug resistance occurs
Combinations not recommended Chloroquine based combinations (e.g CQ + SP; CQ + Artesunate) 1. Artesunate (single dose) + SP 2. Chloproguanil-Dapsone (LapDap) 3.
Antimalarial Chemoprophylaxis Prevents disease, not infection Appropriate for non-immune travelers Consider: immune status intensity/duration of exposure parasite drug resistance
Suppressive prophylaxis Chloroquine, proguanil, mefloquine and doxycycline only effective at killing the malaria parasite once it has entered the erythrocytic stage (blood stage) and therefore have no effect until the liver stage is complete. So these prophylactics must continue to be taken for four weeks after leaving the area of risk. Causal prophylaxis Malarone and primaquine Causal prophylactics target not only the blood stages of malaria, but the initial liver stage as well. So user can stop taking the drug 7 days after leaving the area of risk. Regimens recommended by the WHO for prevention of P. falciparum infection. Doxycycline 100 mg once daily (started one day before travel, and continued for four weeks after returning); Mefloquine 250 mg once weekly (started two-and-a-half weeks before travel, and continued for four weeks after returning); Atovaquone/Proguanil(malarone) 1 tablet daily (started one day before travel, and continued for 1 week after returning). In areas where chloroquine remains effective: Chloroquine 300 mg once weekly, and Proguanil 200 mg once daily (started one week before travel, and continued for four weeks after returning);
Personal Protection Protective clothing Insect repellants Household insecticide products Window and door screens Bed nets Consult physician for proper prophylaxis before traveling to endemic areas - usually anti-malarial drugs starting a day or two, usually chloroquine or mefloquine Treatment - continued through at least four weeks after leaving the endemic area Seek medical help : if having flu-like symptoms