Management of Fever and Hyperglycemia in Acute Ischemic Stroke Case
Learn about the management of fever and hyperglycemia in a patient with acute ischemic stroke, including recommendations for body temperature treatment, common first-line approaches for fever, and relevant clinical guidelines. Understand the importance of addressing these factors in stroke care for optimal patient outcomes.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Case of the week Management of fever and hyperglycemia in a patient with acute ischemic stroke Dr Oyebola Fasugba Prof Sandy Middleton Nursing Research Institute, St Vincent s Health Australia Sydney, St Vincent s Hospital Melbourne & Australian Catholic University
Case of the week A 65-year-old female presents to the emergency department (ED) at 4.35pm with sudden onset of left sided hemiparesis and aphasia. A detailed history from her husband reveals she has a past medical history of hypertension and is currently on Enalapril 10mg orally once a day. She is not on any oral anticoagulant or antiplatelet medications. Evaluation of the patient by the ED physician reveals she has a National Institutes of Health Stroke Scale (NIHSS) score of 13. A brief neurologic examination shows she is conscious and alert and has difficulty with gait/balance with left motor weakness in her upper and lower limbs. She also shows signs of expressive aphasia. Her vital signs are assessed, and she is found to have a temperature of 38.6 C. Blood samples collected from the patient are sent to the laboratory for routine blood tests.
Case of the week Question 1 Recommendations for stroke management include treating a body temperature higher than: a) 35.5 C b) 36.5 C c) 37.5 C d) 38.5 C e) 39.5 C
Case of the week Question 1 Recommendations for stroke management include treating a body temperature higher than: a) 35.5 C b) 36.5 C c) 37.5 C d) 38.5 C e) 39.5 C Summary The Australian Clinical Guidelines for Stroke Management1 and the Canadian Stroke Best Practice Recommendations for Acute Stroke Management2 both recommend treating stroke patients with a fever >37.5 C. The United States Guidelines for the Early Management of Patients with Acute Ischemic Stroke3 and the European Stroke Organisation (ESO) guidelines4 recommend treatment when the body temperature is 38 C.
Case of the week Question 2 Based on her temperature reading, what will be the most common first-line approach to managing her fever? a) Acetaminophen (paracetamol) b) Ibuprofen c) Cooling blankets d) Aspirin e) Ice packs
Case of the week Question 2 Based on her temperature reading, what will be the most common first-line approach to managing her fever? a) Acetaminophen (paracetamol) b) Ibuprofen c) Cooling blankets d) Aspirin e) Ice packs Summary The most frequently used antipyretic is acetaminophen (paracetamol) which works by inhibiting prostaglandin production in the central nervous system.5 It is well tolerated with few adverse events such as the potential for hepatic toxicity.
Case of the week While a beneficial effect on patient outcomes was noted for use of high dose paracetamol in managing fever in acute stroke patients in the Paracetamol (Acetaminophen) In Stroke (PAIS) trial,5 further research of this finding in the PAIS 2 trial did not demonstrate improvement in functional outcome.6 Use of ibuprofen is associated with an increased risk of bleeding. Evidence on the clinical effectiveness of physical cooling or non-pharmacologic measures such as cooling blankets and ice packs is mixed and these measures may lead to shivering and vasoconstriction in patients.7 However,evidence from the QASC trial demonstrated when fever is managed in combination with hyperglycaemia and swallowing in the first 72 hours following stroke this resulted in reduced 90- day death and disability8, 9 with over 20% of patients more likely to be alive four years following their stroke.8, 9
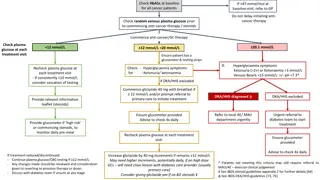
Case of the week Concurrently, the patient undergoes a finger prick test for glucose to rapidly determine her blood glucose level while awaiting results of the venous blood glucose levels from the laboratory. The reading suggests the presence of hyperglycemia with a blood glucose level of 15.6 mmol/L (280.8mg/dL). Question 3 The threshold for treatment of hyperglycemia in acute stroke patients is: a) >5 mmol/L (90mg/dL) b) >10 mmol/L (180mg/dL) c) >15 mmol/L (270mg/dL) d) >20 mmol/L (360mg/dL) e) >25 mmol/L (450mg/dL)
Case of the week Concurrently, the patient undergoes a finger prick test for glucose to rapidly determine her blood glucose level while awaiting results of the venous blood glucose levels from the laboratory. The reading suggests the presence of hyperglycemia with a blood glucose level of 15.6 mmol/L (280.8mg/dL). Question 3 The threshold for treatment of hyperglycemia in acute stroke patients is: a) >5 mmol/L (90mg/dL) b) >10 mmol/L (180mg/dL) c) >15 mmol/L (270mg/dL) d) >20 mmol/L (360mg/dL) e) >25 mmol/L (450mg/dL)
Case of the week Summary Evidence from the Quality in Acute Stroke Care (QASC) trial showed that treatment of blood glucose levels >10mmol/L (180mg/dL) as part of a bundled care package, improves outcomes in patients regardless of their diabetic status at 90 days post-stroke.8 The United States Guidelines for the Early Management of Patients with Acute Ischemic Strokerecommend treating hyperglycemia to achieve blood glucose levels in a range of 7.8 to 10 mmol/L (140 to 180 mg/dL) and to closely monitor to prevent hypoglycemia in patients with acute ischemic stroke.3
Case of the week Neuroimaging using computed tomography (CT) scan shows hyperdensity in the right middle cerebral artery suggestive of a thrombotic occlusion and confirms the diagnosis of acute ischemic stroke. Her platelet count, activated partial thromboplastin time and international normalized ratio (INR) are within normal limits. Intravenous recombinant tissue type plasminogen activator (tPA- Alteplase) is administered at 5.15pm approximately 2 hours after time last known to be symptom-free. Endovascular clot retrieval with recanalization of the right middle cerebral artery is successfully undertaken. The patient s neurological examination improves with a post-procedural NIHSS score of 3. She is transferred to the stroke unit for subsequent monitoring and care.
Case of the week Question 4 How often should temperature and blood glucose levels be monitored in patients with acute stroke? a) Every 30 minutes b) Hourly c) Every 1 to 2 hours d) Every 4 to 6 hours e) All may apply depending on the patient s clinical situation
Case of the week Question 4 How often should temperature and blood glucose levels be monitored in patients with acute stroke? a) Every 30 minutes b) Hourly c) Every 1 to 2 hours d) Every 4 to 6 hours e) All may apply depending on the patient s clinical situation
Case of the week Summary Temperature may be monitored frequently as clinically indicated. It is recommended that while the patient is in the ED, temperature readings should be taken every 30 minutes and 4 hourly in the stroke unit.2, 8 ,10 Blood glucose levels should be monitored 6 hourly for the first 72 hours following admission.10 If blood glucose is >140 mg/dL (7.8mmol/L) and the patient has received thrombolysis, it may be necessary to monitor the blood glucose every 1 to 2 hours, because of the potential for intracranial haemorrhage in these patients.10 The patient is discharged home on aspirin and enalapril after 3 days to continue multidisciplinary team management involving the speech therapist, physiotherapist and occupational therapist to assist with post-stroke rehabilitation and recovery.
Key learning points Monitoring of vital signs such as temperature is an important part of acute stroke care as presence of fever has the potential to affect the patient s prognosis. Evidence shows that fever in acute stroke patients is associated with poor neurological outcome and increased mortality.10 Hence, managing the fever may improve outcomes for patients. Routine blood tests that provide pointers to conditions associated with unfavourable outcomes for the stroke patients or may influence treatment choice should be performed. Measurement of blood glucose levels is essential because hyperglycemia in acute stroke patients has been found to be an independent predictor of larger infarct size, poor clinical outcome and higher risk of mortality.11 It could also counteract the beneficial effect of intravenous thrombolysis and mechanical thrombectomy in patients with acute ischemic stroke.10 Vital sign monitoring in the first 72 hours following stroke has been shown to be associated with 90-day independence.12
References 1. 2. Stroke Foundation. Clinical guidelines for stroke management. 2019. Melbourne, Australia. Boulanger JM, Lindsay MP, Gubitz G, Smith EE, Stotts G, Foley N, Bhogal S, Boyle K, Braun L, Goddard T, Heran MK. Canadian stroke best practice recommendations for acute stroke management: prehospital, emergency department, and acute inpatient stroke care, update 2018. International Journal of Stroke. 2018;13:949-84. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, Jauch EC. 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50:e344-e418. Ntaios G, Dziedzic T, Michel P, Papavasileiou V, Petersson J, Staykov D, Thomas B, Steiner T, European Stroke Organisation. European Stroke Organisation (ESO) guidelines for the management of temperature in patients with acute ischemic stroke. International Journal of Stroke. 2015;10:941-9. den Hertog HM, van der Worp HB, van Gemert HM, Algra A, Kappelle LJ, Van Gijn J, Koudstaal PJ, Dippel DW, PAIS investigators. The Paracetamol (Acetaminophen) In Stroke (PAIS) trial: a multicentre, randomised, placebo-controlled, phase III trial. The Lancet Neurology. 2009;8:434-40. De Ridder IR, den Hertog HM, van Gemert HM, Schreuder AH, Ruitenberg A, Maasland E, Saxena R, van Tuijl JH, Jansen BP, Van den Berg-Vos RM, Vermeij F. PAIS 2 (Paracetamol [Acetaminophen] in Stroke 2) Results of a Randomized, Double-Blind Placebo-Controlled Clinical Trial. Stroke. 2017;48:977-82. Wrotek SE, Kozak WE, Hess DC, Fagan SC. Treatment of fever after stroke: conflicting evidence. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy. 2011;31:1085-91. Middleton S, McElduff P, Ward J, Grimshaw JM, Dale S, D'Este C, Drury P, Griffiths R, Cheung NW, Quinn C, Evans M. Implementation of evidence-based treatment protocols to manage fever, hyperglycaemia, and swallowing dysfunction in acute stroke (QASC): a cluster randomised controlled trial. The Lancet. 2011;378:1699-706. Middleton S, Coughlan K, Mnatzaganian G, Low Choy N, Dale S, Jammali-Blasi A, Levi C, Grimshaw JM, Ward J, Cadilhac DA, McElduff P. Mortality reduction for fever, hyperglycemia, and swallowing nurse-initiated stroke intervention: QASC Trial (Quality in Acute Stroke Care) follow-up. Stroke. 2017;48:1331-6. Summers D, Leonard A, Wentworth D, Saver JL, Simpson J, Spilker JA, Hock N, Miller E, Mitchell PH. Comprehensive overview of nursing and interdisciplinary care of the acute ischemic stroke patient: a scientific statement from the American Heart Association. Stroke. 2009;40:2911- 44. Piironen K, Putaala J, Rosso C, Samson Y. Glucose and acute stroke: evidence for an interlude. Stroke. 2012;43:898-902. Middleton S, McElduff P, Drury P, D Este C, Cadilhac DA, Dale S, Grimshaw JM, Ward J, Quinn C, Cheung NW, Levi C. Vital sign monitoring following stroke associated with 90-day independence: A secondary analysis of the QASC cluster randomized trial. International journal of nursing studies. 2019;89:72-9. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12.