Mechanisms of Tissue Injury in Autoimmune Diseases
Antibodies in autoimmune diseases can opsonize cells and activate the complement system, leading to phagocytosis and destruction of cells. This process is a key mechanism in conditions like autoimmune hemolytic anemia and thrombocytopenia. Immune complexes can also mediate tissue damage in various organs, causing reactions like serum sickness and Arthus reaction. Explore the roles of Type II and III immune responses in clinical examples such as transfusion reactions, autoimmune hemolytic anemia, and more.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
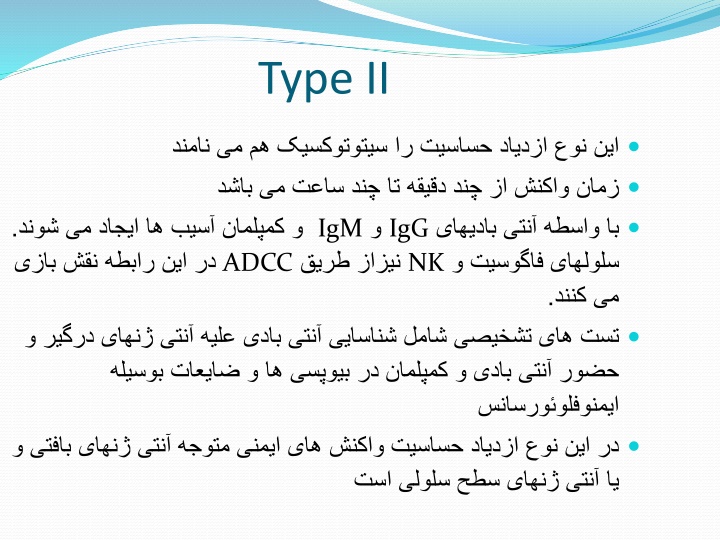
Type II IgM . ADCC IgG NK .
Clinical Examples Transfusion reactions Autoimmune Hemolytic anemia Hemolytic disease of newborn Drug induced hemolytic anemia Cephalosporins Levodopa Methyldopa Penicillin and its derivatives Quinidine Some nonsteroidal anti-inflammatory drugs (NSAIDs) Autoimmune thrombocytopenia Pemphigus vulgaris(desmoglein ) Goodpastures syndrome Myasthenia gravis Graves disease Insulin resistant diabetes Pernicious anemia
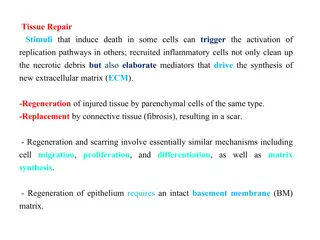
Tissue injury mechanisms Antibodies may opsonize cells or activate the complement system Production of complement proteins that opsonize cells. These cells are phagocytosed and destroyed by phagocytes that express FcR and CR Main mechanism in autoimmune hemolytic anemia and thrombocytopenia and hemolysis in transfusion reactions.
Type III (Immune complex mediated Diseases) Von pirquet 1911
Type III (Immune complex mediated Diseases) The reaction may be general (e.g., serum sickness) or may involve individual organs including skin ( Arthus reaction), kidneys, lungs, blood vessels , joints or other organs. It is mediated by soluble immune complexes The reaction may take few hours after exposure to the antigen The lesion contains primarily neutrophils
Tissue injury mechanisms Antibodies may opsonize cells or activate the complement system Production of complement proteins that opsonize cells. These cells are phagocytosed and destroyed by phagocytes that express FcR and CR Main mechanism in autoimmune hemolytic anemia and thrombocytopenia and hemolysis in transfusion reactions.
Tissue injury mechanisms . Myasthenia gravis Grave
Some diseases caused by immune complexes Systemic Lupus Erythematosus Nephritis Vasculitis Post streptococcal glomerulonephritis
Transplantation A graft transplanted from one individual to the same individual is called autograft A graft transplanted between two genetically identical is called syngeneic graft A graft transplanted between two genetically different individuals of the same species is called allograft A graft transplanted between individuals of different species is called xenograft The molecules that are recognized as foreign on allografts are called alloantigens The lymphocytes and antibodies that react with alloantigens are alloreactive
Alloreactive T cells The activation of alloreactiveT cells require presentation of alloantigenes by donor drived APC in the graft or by host APC that present graft alloantigens
Effector mechanisms of allograft rejection Graft rejection is classified on the basis of histopathologic features or the time course of rejection after transplantation . 1)Hyperacute 2)Acute 3)chronic
Hyperacute rejection Mediated by preexisting antibodies that bind to donor endothelial antigens Activation of complement induce a number of changes in the graft endothelium that promote intravascular thrombosis Begins within minutes to hours aftertransplantation
Acute rejection Mediated by antibodies and T cells that usually begins after the first week of transplantation Th and Tccells by responding to MHC molecules present on vascular endothelial or parenchymal cells cause direct lysis of graft cells or produce cytokines that recruit and activate inflammatory cells which injure the graft Antibodies to vessel wall antigens also mediated acute rejection
Chronic rejection Characterized by fibrosis and vascular abnormalities with loss of graft function occurring during a prolonged period