Medicare Direct Contracting
A briefing on the issues surrounding Medicare Direct Contracting, highlighting concerns with the program's impact on access to care and financial incentives for providers. The discussion covers the potential threats to Medicare's integrity, the role of DCEs in limiting spending, and the implications for vulnerable seniors and disabled individuals. Insights from healthcare policy experts shed light on the risks associated with the current model and its resemblance to managed care schemes of the past.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Medicare Direct Contracting Congressional Briefing Jan. 27, 2022
Introductions Ana Malinow MD Past president, Physicians for a National Health Program (PNHP) Ed Weisbart MD Board member and Chair of Missouri Chapter, PNHP Diane Archer JD Founder of Medicare Rights Center; Founder and CEO of JustCare Eagan Kemp Public Citizen healthcare policy advocate; senior policy analyst at GAO 2008-2017 Additional comments by Don Berwick MD CMS administrator 2010 - 2011; Senior Fellow, Institute for Healthcare Improvement
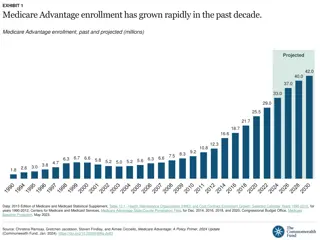
A Trump-administration scheme is continuing to Threaten Our Cherished Public Program Medicare Direct Contracting Launched by CMMI to test new payment models There are now 53 Direct Contracting Entities ( DCEs ) Mostly insurers and investors inserted between Medicare and providers Paid a flat fee to limit spending in Traditional Medicare
A Trump-administration scheme is continuing to Threaten Our Cherished Public Program Medicare Direct Contracting As in Medicare Advantage DCEs have financial incentives to create restrictive networks DCEs have a financial incentive to limit access to medically necessary care and influence participating physicians Evidence from MA suggests DCEs will not save money or improve outcomes
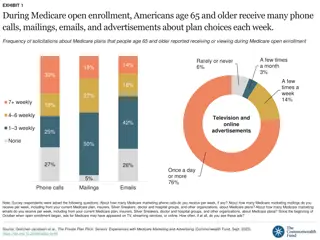
A Trump-administration scheme is continuing to Threaten Our Cherished Public Program Medicare Direct Contracting CMS auto-assigns vulnerable seniors and people with disabilities who specifically chose Traditional Medicare New assignments occur without their knowledge or consent , and we re already hearing a lot of confusion from seniors Patients who want to leave their auto-assigned DCE need to find a different primary care physician not in that DCE HHS has authority to scale up DCEs and similar models across Traditional Medicare without Congressional approval
The Siren Call of Managed Care 1973 HMO Act Direct Contracting Promised to reduce waste and improve quality by aligning financial interests through capitation Promises to reduce waste and improve quality by aligning financial interests through capitation Experience and evidence from managed care (e.g., Medicare Advantage) is raising alarms about the likely impact of Direct Contracting on Traditional Medicare
NCI Cancer Centers may be particularly important to patients with Advanced-stage, Rare, or Complex Cancers 41% 100% of NCI Cancer Centers accept Traditional Medicare of Medicare Advantage plans include no NCI Cancer Centers or the affiliated academic medical center in their provider network Although DCE members retain full access to Medicare s networks, DCEs have similar financial objectives as MA plans KFF analysis of 306 MA plans across 15 counties , 2016. https://files.kff.org/attachment/Report-Medicare-Advantage-Hospital- Networks-How-Much-Do-They-Vary Accessed Jan. 25 2022
Traditional Medicare is Lean, Efficient, and Effective 13.6% 13.2% Overhead and profit 1.8% Traditional Medicare Medicare Advantage Commercial Insurers Source for Traditional Medicare: Calculated from the 2021 Annual Report of the Board of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds. Table II.B1. Excludes Medicare Part C Overhead and Expenditures. Source for Private Insurance: Calculated from 2021 Historical National Health Expenditures Accounts for Year 2018, as net cost of health insurance for private health insurance divided by total NHE expenditures by private insurers. Source for Medicare Advantage: U. S. Government Accountability Office, Medicare Advantage: 2011 Profits Similar to Projections for Most Plans, but Higher for Plans with Specific Eligibility Requirements, no. GAO-14-148 (January 22, 2014).
Traditional Medicare is Lean, Efficient, and Effective 60% 52.6% Commercial Health Insurance Cumulative growth in per-enrollee spending 40% 21.5% 20% Medicare 2008 2010 2012 2014 2016 2018 https://www.axios.com/health-insurance- costs-private-medicare-medicaid-c40bb6f1- c638-4bc3-9a71-c1787829e62e.html Accessed Dec 17, 2019
Upon reaching the age of eligibility for Medicare, USA Mortality Rates Improve from Worst to Best 1 This reflects the impact of Traditional Medicare as it predates high MA market share Help us protect Traditional Medicare 3 USA mortality rate ranked against 17 peer nations 5 7 Age 65 9 Women 11 13 Men 15 17 0-1 1-4 5-9 10-14 15-19 20-24 25-29 30-34 35-39 40-44 45-49 50-54 Age 55-59 60-64 65-69 70-74 75-79 80-84 85-89 90-94 95-99 Institute of Medicine. Shorter Lives, Poorer Health. Fig 1-9: Ranking of US mortality rates by age group among 17 peer countries, 2006-2008. 2013
Direct Contracting creates issues of concern at both Patient and System Levels Patient-level concerns As with Medicare Advantage, upfront capitated payments create a financial incentive for DCEs to: Drive physician behavior in ways that reduce costs without regard to patient care needs or health outcomes Create narrow networks and inappropriately delay and deny care Patient protections are limited: Enrolled without their consent or knowledge Guardrails do not protect them from being advised to drop Medigap or switch to MA Opting out of a DCE requires patients to give up their primary care physicians
Direct Contracting creates issues of concern at both Patient and System Levels System-level concerns Direct Contracting Entities threaten some of Medicare s greatest qualities Cost effectiveness: Like MA plans, DCEs will be able to upcode, despite limits and guardrails Equity: TM distributes risk and costs across a large population and addresses the needs of people with costly conditions without making people surmount large hurdles Transparency:A lack of transparency in DCEs limits CMS s ability to assess strengths and weaknesses, ensure compliance, and drive system improvements Direct Contracting Entities transfer traditional Medicare as a public good into private hands and put us on a path to Medicare s total privatization Risk that DCEs reduce health care spending by creating larger financial and administrative barriers to care for people with Medicare
Wrapping Up (Part 1) and What Were Asking Medicare Direct Contracting is beyond what Congress intended when chartering CMMI Congress should reevaluate the CMMI charter to protect it against future political pressures Urge Secretary Becerra to: Immediately stop assigning any additional members into DCEs Do not activate or approve any additional DCEs Immediately cancel existing DCE contracts; completely dissolve them by July 1, 2022
The current model of Direct Contracting Goes Against the Medicare Mission More aptly named IndirectContracting Introduces new fiscal intermediaries with business imperatives that could prioritize wealth-seeking over health-promotion CMMI models should focus reforms on the Triple Aim: Better outcomes Better care Lower cost (without fiscal intermediaries)
If not possible to stop the DCE model, CMS should Redefine a Limited Direct Contracting Model 1. Eliminate all Insurer DCEs from GPDC model 2. Require DCEs to follow existing ACO requirement for 75% provider governance 3. Eliminate potential for DCE Risk-Score Gaming and clarify publicly 4. Limit the size of the DCE enrollment no more than NextGen 1.3 million 5. Clarify that this is a limited test not the future for ACOs 6. Create Guardrails for Investor DCEs see HA Blog* No expansion of service area or networks 7. Design a new MSSP Track for advanced Provider ACOs for January 2023 8. Explore new Risk Adjustment Methodology to eliminate HCC System *Health Affairs ForeFront Sept 30, 2021
Wrapping Up (Part 2) and What Were Asking If Congress is interested in saving money, focus on the problems in Medicare Advantage Members of Congress can highlight that they delivered on promises to protect Medicare from privatization by ending this Trump-envisioned assault on seniors and people with disabilities