Meningitis
Meningitis is the inflammation of the meninges over the brain and spinal cord. It can be caused by various pathogens such as bacteria, viruses, fungi, and parasites. The infection can lead to symptoms like malaise, headache, fever, neck rigidity, and more. Lab diagnosis involves examining the cerebrospinal fluid (CSF) obtained through lumbar puncture for microbial presence. Treatment depends on the specific pathogen involved.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Meningitis Inflammation of meninges over brain & spinal cord
Source of infection: Blood stream or occassionally by spreading from middle ear or nasal sinuses or face, throat Types: a. Acute pyogenic meningitis b. Tubercular meningitis c. Viral meningitis Signs & symptoms: malaise, headache, fever, intolerance to light, vomitting, convulsions, neck rigidity (severe pain at the back of neck when trying to raise the head in supine position), haemorrhagic rash often associated with meningococcal meningitis
Features Normal CSF Pyogenic Tubercular Viral CSF findings in meningitis 1 . Pressure Normal 2 Total protein 30-45mg% 100--600mg% 80--120mg% 60 80mg% 3 Sugar 40 80mg% or absent 0 20mg% 30 50mg% normal 4 Total cell/cu mm 1--3 1000 20,000 50--500 4--10 5 Type of cell Lymphocytes 98% polymorphs 2%lymphcytes 90%lymphocyte 10%neutro Lymphocytes 6 Bacteriological exam A Gram stain Nil GNB or GPC or GNC or GPB Nil Nil B ZN stain Nil Nil AFB seen also cobweb appearance in CSF Nil C Culture No growth According to agent MTB may grow in LJ medium Viruses may grow in cell culture
Possible pathogens Bacteria (pyogenic meningitis) I. In children & adults: Str pneumoniae, Neisseria meningitidis, Haemophillus influenzae, Staph aureus, E coli, Pseudomonas II. In neonates: E coli, Listeria monocytogenes, Klebsiella pneumoniae, Strep agalactiae (group B) III. Treponema pallidum all ages Tubercular meningitis: Mycobacterium tuberculosis
Viruses: Coxsackie virus, Echo virus, Herpes simlex virus, Arbo virus, Varicella zoster virus, Polio virus(rarely) Fungi: Cryptococcus neoformans, Candida, Aspergillus spp. Parasitic: Naegleria fowleri, Toxoplasma gondii (mostly associated with AIDS), Trypanoma spp.,
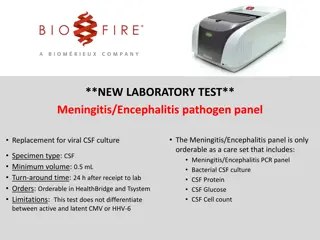
Lab diagnosis 1. CSF is obtained after lumbar puncture & examined immediately after collection or placed in incubator for examination within 1hour 2. CSF is collected in 3 vials: 1.cell count 2.chemical examination 3.culture & staining 3. Appearance : clear/ cloudy/ blood stained 4. Centrifuged deposit: gram stain, ZN stain & negative stain (for capsulated organisms)
Gram stain look for organisms & pus cells Str pneumoniae gram positive lanceolate shape capsulated diplococci Neisseria meningitidis gram negative capsulated diplococci with adjacent side flatte ned and found both intracellularly & extracellularly Haemophillus influenzae- gram negative coccobacilli Staph aureus gram positive cocci in clusters E coli, Klebsiella & Pseudomonas gram negative bacilli Candida gram positive budding yeast cells ZN stain acid fast bacilli, M tuberculosis Negative stain cryptococcus, Streptococcus pneumoniae, Klebsiella &Neisseria
5. Culture :centrifuged CSF deposit is taken up for culture on blood agar, MacConkey agar, chocolate agar & LJ medium (if tubercular meningitis is suspected) and cooked meat broth & incubate Isolated organisms if any are identified by biochemical tests & put up for antibiotic sensitivity testing 6. Blood culture 7. Cell count of CSF & type of cell done in Neubauer chamber & Leishman/Giemsa stain 8. Chemical examination of CSF for glucose & protein
Demonstration of bacterial products a. Bacterial antigens N. meningitidis (group A & C), Haemophillus influenzae & Streptococcus pneumoniae. b. Bacterial endotoxin present in blood can be dected
Aseptic meningitis- meningitis when the causative agent is not detected CSF: highly turbid, cells: 10-500 mostly lymphocytes Causative agent -mostly viruses, few bacteria, fungi &protozoa Fungi mostly in immunocompromised individuals Causative agents: Viruses Mumps V, Herpes simplex, Varicella zoster V. Measles V, Adeno V, Arbo V Entero viruses(ECHO virus, Coxsackie V, polio V.) Bacteria M. tuberculosis, Leptospira, T.pallidum Fungi candida, cryptococcus Protozoa- Acanthamoeba, Naegleria, Toxoplasma
Urinary tract infection -UTI 2ndmost comon infection after respiratory tract infection Def: A disease caused by microbial invasion of the genitourinary tract that extends from the renal cortex of the kidney to the urethral meatus Bacteriuria: presence of detectable bacteria in urine Pyuria: presence of pus cells in urine Normally area from kidneys to proximal urethra is sterile Distal urethra may have transient bacterial flora derived from faecal flora
Types of UTI Lower (ascending infection) 1. Urethritis Upper (haematogenous infection) 1.Acute pyelitis pelvis of kidney 2. Acute pyelonephritis - parenchyma of kidney 2. Cystitis urinary bladder 3. Proctatitis
Predisposing factors 1. Gender: females more prone to infection (i)short urethra & its proximity to anus (ii)sexual contact (iii) pregnancy Males over 60 years due to prostatic enlargement 2. Obstruction to urinary flow: stricture, prostatic hypertrophy, urinary stone, tumour 3. Neurogenic bladder dysfunction: spinal cord injury, multiple scelorisis 4. Highly virulent bacterial infection 5. Reflux of urine from bladder to ureter or renal pelvis 6. Genetic factors 7. Associated illness - Diabetes
Clinical features 1. Asymptomatic: detected only during routine culture 2. Symptomatic: Increased frequency of micturition Dysuria & supra-pubic pain & loin pain Fiver with rigor
Causative agents A. Gram negative bacilli i. Escherichia coli responsible for 70-80% cases (virulence may be associated with K antigens which inhibit phagocytosis & bacterial adhesion by specialised fimbriae) ii. Klebsiella species iii. Proteus species specially P. mirabilis iv. Enterobacter spp. v. Pseudomonas aeruginosa vi. Morganella, Serratia, Acenatobacter spp, Citrobacter
B. Gram positive cocci: i. Staph aureus & saprophyticus ii. Enterococcus spp. iii. Staph epidermidis normally commensal but may be pathogenic in immunocompromised host C. Miscellaneous: i. Mycobacterium tuberculosis ii. Streptococcus agalactiae D. Fungus: Candida albicans in immunocompromised host
Lab diagnosis Urine culture: A. Specimen collection: (i) Mid stream urine collected after cleaning the part thoroughly with soap &water & prior to administering antibiotics (ii) Catheter specimen only if patient is catheterised (collect directly from tube & not from collecting bag) (iii) Infants: clean catch directly into sterile container Transport specimen to lab with minimum delay or refrigerate at 4oC to a maximum of 24 hours
1. Microscopic examination: centrifuge urine & examine deposit for pus cells, epithelial cells, RBC, bacteria, casts & crystals 2. Culture: Standard loop technique standard caliberated loop is used to culture a fixed volume of urine (24 SWG wire, 4mm internal diameter holds 0.005 ml urine: 200loopful=1ml Inoculate one loopful each on MA &BA and incubate at 37oC overnight
Day 2: examine plate for total number of colonies x200 = total colonies/ml Identify organism based on gram stain, biochemical tests & slide agglutination test & perform antibiotic susceptibility testing by Kirby Bauer method or Stokes method Colony count >105/ml of single species is Significant Bacteriuria indicates active UTI & needs to be treated Differenciation of upper and lower UTI: antibody coated bacteria dected by immunofluorescence staining indicates Upper UTI
Tuberculosis of kidney (haematogenous infection) Increased frequency with painless haematuria & no pathogen detected in culture 3 consecutive early morning specimen collected since intermittent excretion of bacilli Centrifuged deposit ZN staining acid fast bacilli Centrifuged deposit cultured on LJ medium & incubated for 6-8weeks- growth identified by ZN stain &Niacin test