Motor Delay and Hypotonia in Children: Diagnosis and Evaluation
Explore the case of Felix, an eighteen-month-old boy presenting with motor delay and hypotonia. Learn about the importance of identifying and treating hypotonia, along with the diagnostic studies and questions for review. Discover the potential treatment options for co-occurring medical and developmental conditions associated with motor disorders.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
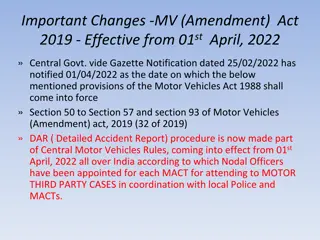
Motor Delay/Disorders: Treatment DBP Fellow Foundations 2021
Review co-occurring medical and developmental conditions for the following motor disorders Hypotonia Cerebral Palsy Spina Bifida Disorders of muscle weakness Learning Objectives Discuss treatment practices for co- occurring medical and developmental conditions for the above motor disorders
Felix is an eighteen month old boy being seen for a new visit in Neurodevelopmental Fellow s clinic. Family reports to you that they are concerned that he is not yet walking, and uses a couple of words including mama and dada. Family s other children ages 4 and 8, walked around 12 months of age and were very chatty by the time they were Felix s age. Family denies any developmental regression, only that developmental progress has been much slower than expected. Physical examination is notable for normal and symmetric movements against gravity, although coordination is immature. He is getting into and out of sitting independently and onto all fours, but not yet pulling to stand or cruising. Reflexes are normal to brisk, muscle bulk normal but soft to palpation. Decreased resistance to flexion and extension of extremities noted, as well as axillary slip through with upright suspension. Family is looking to you to determine next steps to 1) identify and etiology and 2) provide recommendations for treatments Felix
What do you think is the most likely diagnosis? Hypotonia Normal strength, normal reflexes and normal movements against gravity No regression Physical examination consistent with hypotonia Why?
What studies would you perform? Why? Serological Neurological Genetic Other
On your review of systems, what questions are going to be most important to ask and why?
Trouble with chewing and swallowing- dysphagia Oral or pharyngeal Aspiration Consistency of foods matters Time it takes to eat long or short Certain types of food refusal Clinical feeding evaluation Video fluroscopic swallow study Feeding therapy mechanical or behavioral Thickener Gastrostomy tube
Trouble Sleeping Difficulties with initiation Difficulties with maintenance Snoring Restlessness Sleep walking/parasomnias depending on age Restless leg syndrome (low ferritin treat with ferrous sulfate) Apnea- confirmed with sleep study, recommendation for surgical or medical intervention Delayed sleep onset: melatonin Behavioral insomnia of childhood
Hearing or vision problems Particularly hearing given the language delay But these are two systems that we have lots of evidence based treatment approaches which improve outcomes, so we always ask about those
Gastrointestinal Reflux or Constipation Dysmotility in gut common in children with hypotonia, including slower transit times. Commonly in toddlers leads to constipation, but can also cause significant GE reflux in infancy which can lead to oral aversion. Picky diet can exacerbate constipation Discussion about what constipation looks like Treatment with stool softeners as well as stimulant laxatives often improves GE reflux as well with lower stool burden. Children with hypotonia will be always at risk of having constipation even if diet and fluid intake are appropriate
Musculoskeletal issues Flat feet Scoliosis Hip and joint pain Often orthotics provided for feet to provide not only arch support but ankle stability in early childhood evidence for this is inconsistent Low threshold for ordering spine films if asymmetry noted and referral to orthopedics if necessary Physical therapy to improve conditioning and improve mechanics also helps build strength which can improve skills
What sort of developmental supports would you want to put in place, and why? Speech therapy through Birth to Three Alternative and augmentative communication strategies (AAC) if possible Physical Therapy: gross motor skills Occupational Therapy: activities of daily living and fine motor skills Feeding Therapy
Maggie is a nine-year-old with cerebral palsy being seen for a follow up visit in Neurodevelopmental Fellow s clinic. Family reports to you that they are concerned that she is not sleeping well during the night, and that they are having difficulty getting her dressed as well as changing her diapers. They describe her as loving school, and is an active participate in class, she is functioning at grade level in ELA, math and science, and has a paraeducator to support her physically during her general education classes. She uses a wheelchair for all types of mobility both at home and community settings Maggie Physical examination is notable for an engaged 9-year-old girl, using an AAC device to communicate her needs. Family is looking to you to determine next steps to 1) identify and etiology and 2) provide recommendations for treatments Cerebral Palsy Research Network
What GMFCS Level would she be? On your review of systems, what questions are going to be most important to ask and why?
Oral Pharyngeal Function Dental complications Motor challenges with handling dental hygiene Excessive gagging Gingivitis due to seizures Food in mouth longer caries Malalignment of upper and lower teeth Lip tongue and check biting Dysarthria Speech understandability Impaired oral communication AAC Dysphagia with aspiration Risk for chronic silent aspiration Video fluoroscopic swallow study Gastrostomy tube/dietary modifications Sialorrhea Aspiration Social isolation Oral medications (glycopyrulate) Botox to the salivary glands
Nutrition/GI Constipation Gastroesophageal Reflux GI Dysmotility Increased risk poor nutrition due to oral, pharyngeal, and gastrointestinal dysfunction May need assistance with feeding due to motor dysfunction Adaptive treatment approaches Thickening Pureeing Gastrostomy tube
Sleep Very common! Sleep can be problematic for the following reasons GE Reflux, constipation (cramping) Pain: musculoskeletal, pressure sores Sound sensitivity Drooling seizures Common sleep conditions Abnormal melatonin production Abnormal neurological sleep patterns Sleep disordered breathing: central and obstructive
Hearing or vision problems Hearing: sensorineural, conductive Vision Cortical visual impairment Strabismus myopia
Musculoskeletal Scoliosis Hip dislocation Due to challenges with typical weight bearing Monitor with annual xray Contractures Ongoing research looking into whether our therapeutic approaches (stretching, botox, other tone management) reduces severity or prevents contractures jury is still out Foot and knee deformities Adaptive devices often used Surgical options exist Cervical spine stenosis Much more common in dystonic types CP Bone health Increased risk of fracture due to low bone mineral density Serum vitamin d checked at least annually Vitamin d and calcium supplementation often required Risks for curvature increase during periods of growth Monitor with annual xray
Musculoskeletal Surveillance Scoliosis Monitor with annual xray Hip dislocation Monitor with annual xray Contractures Monitor annual or biannual exam documenting pt full range of motion Foot and knee deformities Cervical spine stenosis Review signs and symptoms of c-spine compression Bone health Serum vitamin d checked at least annually
Musculoskeletal treatments- medical management Orthopedic interventions Tendon lengthening Tendon transfer Osteotomies Spine surgery Oral Medications Dystonia Baclofen Trihexyphenidyl (Artane) L dopa, carbidopa-levodopa Oral medications Spasticity Baclofen Diazepam (valium) Tizanidine Dantroline Gabapentin Intramuscular medications botox Neurosurgical tone management Baclofen pump Selective dorsal rhizotomy Deep Brain Stimulation under exploration for dystonia type CP
Musculoskeletal treatments- Therapeutic management Physical Therapy Resistance/Strength training Functional balance training Coordination exercises Treadmill/Gait training Robotics robotic assisted movement Endurance training Sports skills training Stretching Support with adaptive and assistive equipment, selection and fitting Aquatic Exercise Therapy Occupational Therapy Constraint induced movement therapy Hand arm bimanual intensive therapy Sensory integrative therapy
Neuro Increased risk for seizures
Co-occurring developmental conditions Disorders of cognition Disorders of learning Autism Spectrum Disorder ADHD
Co-occurring mental health conditions Anxiety disorders Depressive disorders
Leo is a 4 year old boy with L2-L3 myelomeningocele coming into clinic for his semi-annual routine developmental medicine visit. Family reports in general he is doing well, going to preschool, and has friends. Leo Family would like to better understand Leo s motor abilities today, and whether to expect any changes as he grows up. They would also like to discuss when or if Leo will achieve independence with his self care routines
What biological challenges would you expect a child with L2- L3 myelomeningocele to experience?
Bends at hips +/- knee extension - Ankle flexion or extension - May at a young age be able to independently ambulate with support of walker or arm crutches As get older will probably rely on wheel chair mobility - Gross Motor Function
Neurogenic bowel No rectal sensation No sphincter control Oral Medical Management: Stool Softeners Stimulant Laxatives Gastrointestinal Function Rectal Medical Management: Enemas Cone enema saline + glycerine Balloon enema Phosphate Enemas (Fleets) Suppositories - lubricate rectum and anus and provide stimulation Surgical Bowel Management Cecostomy: an artificial tube from the skin of the abdomen through to the cecum, which is the entrance to the large intestine. A couple weeks after the procedure, the surgeon places either a Chait Trapdoor or MIC-KEY button, which needs to be changed about twice a year. ACE: anterograde continence enema, use the appendix to make a channel to the abdominal wall. https://spinabifidabowelmanagement.com/
Urological Function 1) Neurogenic Bladder 2) Urinary retention urinary tract infections hydronephrosis renal impairment Urological Interventions 1) Clean Intermittent Catheterization 2) antibiotics 3) anticholinergic meds 4) botox to bladder 5) vesicostomy UROLOGIC CARE AND MANAGEMENT.PDF (spinabifidaassociation.org)
Neurological Function 1) Hydrocphalus 2) Syrinx 3) Chiari Malformation
Developmental Profile -Children with SBM can identify faces and read words, but have difficulty with visual spatial reasoning and visually-guided goal-directed action. -Strengths are noted in vocabulary and grammar. However, children with SBM experience challenges at the level of oral discourse, comprehension, and the use of language in context (pragmatics).12 Individuals with SBM have difficulty in matching language output to a changing social language context. -Children with SBM can learn math facts. However, complex procedures that require multiple steps and algorithms are an area of challenge. They often experience difficulties with estimating quantities and have impaired problem-solving skills. Problems with math, a long-term predictor of adult independence, are common in adults and children with SBM -Many children with SBM meet criteria for Attention Deficit Disorder, Predominantly Inattentive Type (ADD).22-23 However, in contrast to children with ADD related to frontal lobe dysfunction, the attention profile of children with SBM is characterized by under- arousal and excessive persistence in controlling attentional focus. -Individuals with higher lesion levels have more severe neuro-anatomic brain malformations and higher rates of intellectual disability. Spinal defects at T12 and above are more frequent among individuals of Hispanic/Latino ethnicity. These populations also often have lower socio-economic status, diminished access to care and adverse outcomes attributable to social determinants of health.