Neonatal Haematology Insights: Blood Count, Anaemia & Causes
Explore the intriguing world of neonatal haematology with insights on normal blood count variations, anaemia development, and potential causes such as haemolysis and immune factors. Dive into the journey of blood cells in newborns and understand the unique characteristics of neonatal haematology.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
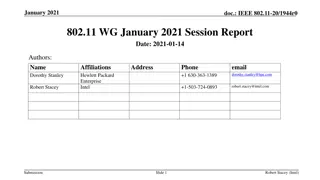
Neonatal haematology Ass.prof.Abeer Anwer Ahmed
Normal blood count The cord blood Hb varies between approximately 16.5 and 17 g/dL and is influenced by the timing of cord clamping The reticulocyte count is initially high (2-6%) but falls to below 0.5% at 1week as erythropoiesis is suppressed in response to the marked increase in the oxygenation of tissues This is associated with a progressive fall in Hb to approximately 10-11 g/dL at 8 weeks from which point it recovers to 12.5 g/dL at around 6 months birth
In the blood film, nucleated red cells will be seen for the first 4 days and for up to 1 week in preterm infants. Numbers are increased in cases of hypoxia, haemorrhage or haemolytic disease of the newborn (HDN). MCV averages 119 fL but falls to adult levels by around 9 weeks. By 1 year, the MCV has fallen to around 70 fL and rises throughout childhood again to reach adult levels at puberty. Preterm infants have a more dramatic fall in Hb to 7-9 g/dL at 8 weeks and are more prone to iron and folate deficiency in the first few months of life.
Neutrophils are initially high at birth and fall to plateau at 4 days-from this point on the lymphocyte count is higher than neutrophils throughout childhood
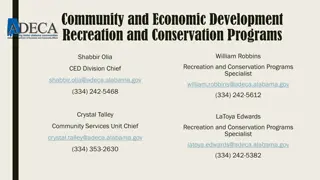
Anaemia in the neonate This should be considered for Hb <14 g/dL at birth. The clinical significance of anaemia is compounded by the high (70-80%) levels of HbF at birth, as this is less effective than HbA at releasing oxygen to the tissues
Causes 1 Haemorrhage: Fetomaternal, twin-twin, cord, internal, placenta. 2 Increased destruction: Haemolysis (immune or non-immune) or infection. 3 Decreased production : Congenital red cell aplasia, infection (e.g. parvovirus). Anti-Kell causes alIoimmune anaemia of the fetus and newborn with decreased erythropoiesis.
Generally, anaemia at birth is usually secondary to immune haemolysis or haemorrhage; Nonimmune causes of haemolysis appear within 24 h Impaired red cell production is usually not apparent for at least 3 weeks.
Haemolysis is often associated with severe jaundice and the causes include HDN autoimmune haemolytic anaemia (AIHA) in the mother congenital disorders of the red cell membrane or metabolism. Red cell transfusion may be needed for symptomatic anaemia with Hb <10.5 g/dL or a higher threshold if there is severe cardiac or respiratory disease
Anaemia of prematurity Premature infants have a more marked fall in Hb after birth and this is termed physiological anaemia of prematurity. Features include: a slowly falling Hb normal blood film and reticulocytopenia. It can be minimized by ensuring adequate iron and folate replacement and limiting phlebotomy. Erythropoietin is used in some centers.
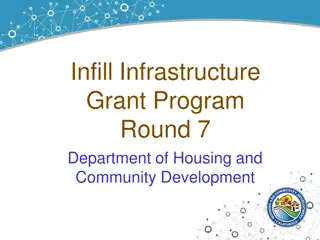
Neonatal polycythaemia This is defined as a venous haematocrit over 0.65 and can occur with: twin-twin transfusion intrauterine growth restriction maternal hypertension or diabetes. If symptoms are present it should be treated with partial exchange transfusion using a crystalloid solution.
Fetomaternal alloimmune thrombocytopenia Fetomaternal alloimmlme thrombocytopenia (FMAIT) results from an immunological process similar to that which causes HDN. Fetal platelets that possess a paternally inherited antigen (HPA-1a in 80%; HPA-5b in 15%) that is not present on maternal platelets can sensitize the mother to make antibodies that cross the placenta ,coat the platelets ,which are then destroyed by the reticuloendothelial system and lead to serious bleeding, including intracranial haemorrhage.
Alloimmlme thrombocytopenia differs from HDN in that 50% of cases occur in the first pregnancy. Its incidence is approximately1 in 1000-5000 births. Thrombocytopenia can lead to serious, sometimes fatal, bleeding in utero or after birth. Treatment is unsatisfactory. Severe postnatal cases may be treated with a platelet transfusion that is negative for the relevant antigen. Antenatal treatment may be either maternal intravenous immunoglobulin or fetal transfusion with HPA-compatible platelets.
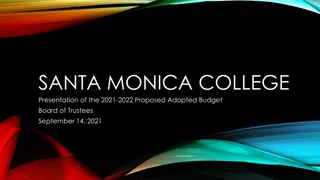
Coagulation Standard tests need to be interpreted with caution in the neonate. The activated partial thromboplastin time (APTT) and prothrombin time (PT) are prolonged because of reduced levels of the vitamin K dependent factors II, VII, IX and X, and return to normal at around 6 months. The thrombin time (TT) is comparable with adult values
Neonates have an increased risk of thrombosis. This is a result of physiologically low levels of inhibitors of coagulation Antithrombin (AT) and protein C levels are approximately ,60% of normal for the first 3 months. Homozygous protein C deficiency is associated with fulminant purpura fulminans in early life. Therapeutic protein C concentrates are now available.
Homozygous AT deficiency usually presents later in childhood but arterial and venous thrombosis may also occur in the neonate