Neonatal Total Parenteral Nutrition Overview
Neonatal Total Parenteral Nutrition (TPN) is essential for meeting metabolic and nutritional needs in newborns when enteral nutrition is inadequate. Explore indications, components, formulation, administration, monitoring, complications, and weaning of TPN along with its goals and challenges.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
NEONATAL TPN NEONATAL TPN Dr. ALOLIKA NANDI 1
NEONATAL TPN NEONATAL TPN Need for TPN Indications Components Formulation Administration Monitoring Complications Weaning of TPN Challenges Take home messages 2
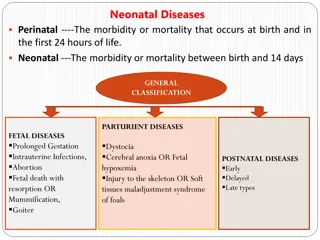
NEED FOR TPN NEED FOR TPN Metabolic & nutritional needs of a newborn are equal to/ greater than fetus of the same GA Subsequentgrowth failure Undernutrition at critical stages of development Poor neurodevelopment outcomes TPN is indicated when normal metabolic and nutritional needs are not met by normal enteral nutrition 3
NEED FOR TPN NEED FOR TPN Goals of TPN 1. achievement of PN growth similar to normal fetus at same GA 2. ensuring optimum long term neurodevelopment AGGRESSIVE ENTERAL FEEDING OPTIMAL TPN 4
INDICATIONS OF TPN INDICATIONS OF TPN No available National guidelines Individualised approach, broad guidelines Not on significant enteral feeds for > 3-5 days/previously established enteral feeds stopped due to illness & enteric nutrition unlikely to start in 3-5 days, or Anticipated to be receiving < 50% of total energy requirement by day 7 of life Surgical conditions- NEC,Gastroschisis,Omphalocele,TEF,Malrotaion, Intestinal atresia etc 5
INDICATIONS OF TPN INDICATIONS OF TPN WHOM ? (Birth weight) WHEN ? < 1 kg Day 1 1 1.499 kg Not on significant feeds for >/= 3 days > 1.5 kg Not on significant feeds for >/= 5 days 6
COMPOSITION OF TPN COMPOSITION OF TPN 1.Carbohydrates : Glucose for Energy 2.Proteins : Crystalline AAs for Positive N2 balance & Growth 3.Fats : Lipids for Energy & to prevent EFA deficiency 4.Electrolytes : Na, K, CL-,Ca2+,PO43-,Mg2+ 5.Trace elements : Zn , Cu , Mn , Se , Fl , I2 , Fe 6.Vitamins 7
Energy Energy Energy needed for 1. Resting Metabolic Rate 2. Activity 3. Thermoregulation 4. Growth Energy requirement of Normal PT @ 110- 120 kcal/kg/d Normal T @ 90- 100 kcal/kg/d Carbohydrate -> Dextrose -> 3.4 kcal/g Lipids -> 9 kcal/g Protein accretion = Protein : Energy ratio = 3-4g/ 100 kcal 8
Carbohydrates, Protein, & Carbohydrates, Protein, & Lipids Lipids Component Commercial preparation Concentration Dose Carbohydrates Dextrose 5%,10%,25%,50% GIR @ 4-6 mg/kg/min Can be increased/decreased by 2 Max 12-14 mg/kg/min Protein Crystalline Amino acids, (Aminovein) 10% 20% 1.5 gm/kg/d, increase by 1 gm/kg/d Max 3 gm/kg/d ( terms ) 4 gm/kg/d ( preterms ) Lipids Intralipid/ SMOF Intralipid (10%/20%) S(Soya 30%) M ( MCT 30% ) O ( Olive Oil 25%) F (Fish Oil 15% ) Started @ 1g/kg/d Increased by 1g/kg/d Max of 3 g/kg/d 9
Electrolytes Electrolytes Component Commercial preparation Concentration Dose 0-3 mEq/kg/d ( 1st week) 2-3 mEq/kg/d ( >1st week, term) 3-5 mEq/kg/d ( >1st week, preterm) Sodium Inj Nacl 0.9% ( 0.15 mEq/ ml) 3% ( 0.5 mEq/ml) 0-2 mEq/kg/d ( 1st week) 1-3 mEq/kg/d ( >1st week) Potassium Inj Kcl 15% (0.5 mEq/ml) Chloride Inj Nacl/ Inj Kcl - 3 mEq/kg/d Calcium Inj Ca gluconate 10% (9mg/ml ) Day 1 : 3-4 mg/kg/d Day 2 onwards : 6-8 mg/kg/d Phosphate NA - 1-2 mEq/kg Magnesium Inj Mg SO4 50% ( 4 mEq /ml ) 0.3-0.5 mEq/kg 10
Trace elements Trace elements- - Component Commercial Preparation Dose Zinc NA @ 150 400 mEq / kg / d from day 1 Cu Mn Se Celcel 4/5 ( Claris) > 2 weeks of PN Fl Iodine Fe > 3 weeks of PN 11
Vitamins Vitamins- - Commercial preparation Composition Dosage Adult MVI Does not provide Vitamin K, B12, Biotin & Folic acid @ 1.5 ml/kg to lipid solution Inj Vitamin K 10mg/ml 0.5 1 ml/kg I. M. Weekly Inj Vitamin B12 1000mcg/2ml 10 mcg/kg I. M. Weekly 12
Formulation of TPN Formulation of TPN Check list 1. Patent iv line 2. BS, SE, RFT, Ca, pH 3. Urine for glucose 4. Hemodynamic & cardiorespiratory stability Step 1 Total TPN volume = Total fluid intake for the day (drug volume, feed volume, blood products, arterial line volume) Step 2 Fat volume =( __ g/kg/d __ kg) / 0.1 or 0.2 {10%=0.1, 20%= 0.2} Step 3 - Glucose AA volume = ( Total TPN volume Fat volume ) 13
Formulation of TPN ( contd.. ) Formulation of TPN ( contd.. ) Step 4 Additive volume A) AAs = ___g/kg/d __ kg 10 B) Na = ___ mEq /kg/d __ kg 2 { 3% Nacl} or 6.6 { 0.9 % Nacl } C) K = ___ mEq/kg/d __ kg 0.5 D) Ca = 8 ml /kg/d __ kg E) Mg SO4 = 0.25 ml/kg/d __ kg Total additive volume = A + B + C + D + E 14
Formulation of TPN ( contd.. ) Formulation of TPN ( contd.. ) Step 5 Dextrose Volume = ( Glucose AA volume) Additive volume Step 6 Dextrose amount = __ mg/kg/min 60 24 Step 7 Dextrose conc = amount / volume 100 = % dextrose Step 8 1.5 ml/kg/d MVI to fat volume Final TPN Line 1 = Lipids + MVI @ ___ ml/hr Line 2 = Glucose + AAs + Trace elements @ ___ ml/hr 15
Preparation Preparation- - Thorough asepsis Dextrose, AAs, Electrolytes in glass bottle, lipids & MVI in syringe By volumetric infusion pump, bacterial filter No multiple punctures Tubing to be changed every 24 hours Iv extravasation to be assessed early Avoid breakage of TPN line, dedicated lumen, heparin not routinely used TPN should be covered with opaque paper 16
Route of administration Route of administration- - Central line ( UVC ) / PICC line / peripheral line Central Line when? a) > 5 days b) % D > 12.5 c) Osm > 900 mosm / L Adv more conc solution Disadv increased risk of infection Lipids & carb aa mineral solution can be given by same iv line by means of a Y connector It offers protection against phlebitis / potential loss of access sites 17
Monitoring Monitoring Vital signs Temp, Pulse, B. P, Resp Rate, Pulse Oximetry Lab parameters- Parameter BS Frequency 2-3 times (changing GIR), once a day (stable GIR) Urine sugar Once / nursing shift Serum electrolytes Twice weekly, weekly Blood urea Ca, Mg, Po4 Twice weekly, weekly Weekly PCV Weekly LFT Tgs Weekly Weekly 18
Monitoring.. ( Monitoring.. (Contd Contd) ) Anthropometry Frequency Weight Daily at the same time HC Weekly Length Weekly IV site 1 hourly 19
Complications Complications- - Low / excessive carbohydrate infusion -> Hypoglycemia, hyperglycemia, glycosuria,hyperosmolarity, dehydration Protein intolerance -> metabolic acidosis, azotemia, hyperammonemia Lipids -> hyperlipidemia, abnormal platelet adhesion, Increased risk of bilirubin encephalopathy Metabolic bone disease -> phosphorus and mineral deficiency Trace element deficiency (after prolonged TPN) Cholestasis & abnormal liver enzymes PNALD Catheter related -> occlusion, dislodgement, infection 20
Management of common complications Management of common complications- - Hyperglycemia R/O sepsis, any drugs ( eg. Steroids) BS >100 mg/dl : No increase in GIR, BS > 150 mg/ dl : Reduce GIR by 2 BS > 200 mg/dl : Insulin infusion @ 0.05 U /kg/ hr ( max 0.2 U/kg/ hr) PNALD : Serum direct bilirubin 2mg/dl, lipid replacement / restriction, start MEN, decrease AAs to 1gm/kg/d Sepsis : Limit lipid infusion @ 1-2 g/kg/d, monitor Tg levels,antibiotics, low threshold for antifungals, Remove CVC if possible 21
Weaning Weaning Weaning can be gradually begun once enteral feeds have reached 50ml/ kg/ d TPN rate should be decreased in tandem with rate of advancement of enteral feeds Vitamins, Minerals & Proteins can be stopped abruptly when feeds have reached 50% of Total intake Glucose conc should be decreased by 1-2%/ day until GIR of 4mg/kg/min is attained Lipid infusion should be tapered by 1gm/kg/day PN can be stopped once enteral nutrition is tolerated @ 100- 120 ml/kg/d 22
Challenges in India Challenges in India- - Understaffing, Lack of training, & infrastructure Early vs Late TPN -> challenging to recommend in our setting Availability of readymade solutions, Manual mixings & its risks Venous access -> Central vs Peripheral Infections- Overcrowding, understaffing, lack of laminar flow Monitoring -> Challenge, standardised monitoring chart Cost of - central lines, - TPN constituents, - frequent Monitoring, - increased hospital stay 23
Take home message Take home message TPN & enteral nutrition go hand in hand Early & aggressive nutritional strategies can prevent PN growth failure (EUGR ) Start TPN on Day 1 + Enteral nutrition 3-4 gms/kg amino acids -> Day 1 1 gm/kg lipids -> Day 1 2 gm/kg lipids -> Day 2 3 gm/kg lipids -> Day 3 SMOF lipids preferable Na, K, Ca Day 2 onwards Trace elements when available 24
Take home message ( contd..) Take home message ( contd..) Strict aseptic precautions from preparation to delivery TPN till 120 ml/kg feeds are reached Monitoring while on TPN 1. Vital signs 2. Labs 3. Growth parameters Peripheral/ Central lines All preparations for single use only 25
Hours, not days are the longest periods infants should be allowed to not receive nutrition after birth intravenously or enterally . 26
Thank you Thank you 27