NEW TREATMENT OPTIONS IN ASTHMA
Asthma affects millions worldwide, impacting quality of life and requiring effective treatment strategies. Prof. Ferah Ece discusses the stepwise approach to asthma management, emphasizing the importance of regular assessment, treatment adjustment, and response review. By implementing appropriate controller medications and relievers based on symptom severity, patients can achieve better asthma control and lead active lives. Explore the latest advancements in asthma care to improve outcomes and reduce exacerbations.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
NEW TREATMENT OPTIONS IN ASTHMA Prof. Ferah Ece, MD, FCCP IstinyeUniversity School of Medicine Department of Chest Diseases Liv Hospital
I have no financial or other conflicts of interest to report
Asthma is one of the most common chronic diseases worldwide with more than 300 million affected individuals with enormous socioeconomic impact with approximately 10% having severe or uncontrolled asthma When asthma is well-controlled, patients can Avoid troublesome symptoms during the day and night Need little or no reliever medication Have productive, physically active lives Have normal or near-normal lung function Avoid serious asthma flare-ups (also called exacerbations, or severe attacks)
Asthma treatment is planned in 3 ways: 1) Assess 2) Adjust treatment (pharmacological and non-pharmacological) 3) Review the response After assessing the patient with asthma, regular daily controller treatment should be initiated. After starting initial treatment response should be reviewed within 1-3 months. If asthma has been well controlled for 3 months, decreasing the dose should be considered
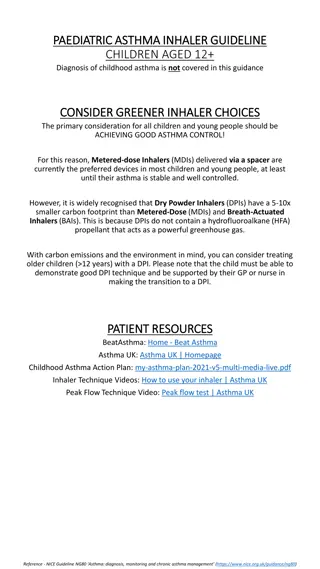
Stepwise approach Step 1 ) as-needed inhaled short-acting beta2-agonist (SABA) This option should be reserved for patients with infrequent symptoms (less than twice a month) of short duration, and with no risk factors for exacerbations Step 2 ) low-dose controller + as-needed inhaled SABA Low dose ICS reduces symptoms and reduces risk of exacerbations and asthma-related hospitalization and death Step 3 ) one or two controllers + as-needed inhaled reliever preferred options are either combination low dose ICS/LABA maintenance with as-needed SABA, OR combination low dose ICS/formoterol maintenance and reliever regimen Step 4 ) two or more controllers + as-needed inhaled reliever preferred option is combination low dose ICS/formoterol as maintenance and reliever regimen, or combination medium dose ICS/LABA with as-needed SABA Step 5 ) higher level care and/or add-on treatment Add-on tiotropium for patients 12 years with history of exacerbations, Add-on anti-IgE (omalizumab) for patients with severe allergic asthma, Add-on anti-IL5 (mepolizumab (SC) or reslizumab (IV)) for severe eosinophilic asthma ( 12 yrs)
SALFORD Trial open-label, randomised, controlled, two-arm effectiveness trial ICS/vilanterol improved asthma control
Management of severe asthma Optimize dose of ICS/LABA Complete resistance to ICS is rare Consider therapeutic trial of higher dose Consider low dose maintenance oral corticosteroids Monitor for and manage side-effects, including osteoporosis Add-on treatments without phenotyping Tiotropium - reduces exacerbations (history of exacerbations, age 12 years) Theophylline, LTRA limited benefit Phenotype-guided treatment Severe allergic asthma: add-on omalizumab (anti-IgE) Severe eosinophilic asthma: add-on mepolizumab or reslizumab (anti-IL5) Sputum-guided treatment to reduce exacerbations and/or steroid dose Aspirin-exacerbated respiratory disease: consider add-on LTRA Non-pharmacological interventions Consider bronchial thermoplasty for selected patients Comprehensive adherence-promoting program
Why the search for new drugs Asthma has a complex pathogenesis Patients who aren t controlled even by oral steroids need an alternative Need a drug which can reduce the dose of steroid or replace it
New approaches to treatment Novel class of bronchodilators New antiinflammatory therapies Immunomodulatory therapies
Novel class of bronchodilators 1) Magnesium sulphate Reduces cytosolic calcium in airway smooth muscle bronchodilation Can be given by iv/nebulisation Not suitable to be employed alone as clinical benefit is small
2) Atrial natriuretic peptide (ANP) and related peptide Urodilatin Urodilatin is paracrine regulator for sodium and water homeostasis Bronchodilator effect comparable to SABA Useful for additional bronchodilation in severe asthma 3) Vasoactive Intestinal Peptide (VIP) analogs VIP binds to VIP receptor type-1 (VPAC1) (smooth muscles of blood vessels) and VIP receptor type-2 (VPAC2)(airway smooth muscle), stimulates adenyl cyclase Potent bronchodilator but is rapidly metabolised, SE high More stable analog of VIP (RO 25-1533) selectively stimulates VPAC2 but effect is not prolonged smooth muscle relaxation
New anti-inflammatory drugs 1) NF-kB inhibitors NF is a transcription factor regulating inflammatory genes in asthma When NF is inhibited susceptibility to infections 2) Mitogen activated protein kinase inhibitors MAP kinase pathways are involved in inflammation Inhibit synthesis of inflammatory mediators but severe toxicity
Others 1) Anticholinergics 2) Bronchial thermoplasty 3) Antibiotics
Tiotropium (Spiriva) Long-acting muscarinic antagonist (LAMA) In use for over decade as one of the mainstays of COPD therapy Asthma approved as a second indication by the FDA Included in the GINA guidelines as a possible add-on at step 5 Image result for spiriva respimat inhalation spray Spiriva Respimat Inhalation Spray Once daily 2.5 mcg dose
When added to an inhaled glucocorticoid, tiotropium improved symptoms and lung function in patients with inadequately controlled asthma.
The study was designed to compare the effectiveness of tiotropium + ICS vs LABA + ICS in delaying time to first exacerbation The findings do not support the superiority of LABA + ICS Compared with tiotropium + ICS for black patients with asthma.
Bronchial thermoplasty It is a potential treatment option for adult patients whose asthma remained uncontrolled despite optimal therapy regimens Bronchoscopic procedure in which bronchial smooth muscle mass is reduced by (essentially) RF ablation Series of 3 procedures Carries an increased risk of asthma exacerbation immediately after the procedure
Randomized 109 patients on highdose ICS/LABA (step 4 or 5 per GINA guidelines) to maintenance therapy with azithromycin or placebo
Overall, there was no benefit seen with azithromycin therapy However, subgroup analysis showed that patients with noneosinophilic asthma had fewer exacerbations this result suggests azithromycin may be an effective option for the neutrophilic/Th-1 phenotype (COPD is also neutrophilic)
Immunomodulatory therapies 1) Immunosuppressive therapy (methotrexate, cyclosporine, gold salts, etc.) Not employed any more (greater SEs and lesser efficacy) 2) Specific immunotherapy subcutaneous immunotherapy (SCIT) sublingual immunotherapy (SLIT) 3) Anti IgE therapy
Omalizumab (Xolair) Applies to a more discrete patient population Anti-IgE mAb Criteria: Skin or serum allergen testing positive for a year-round allergen such as dust mites, molds, animal dander, etc An elevation in total serum IgE
4) Interleukin-5 Antagonists Monoclonal Antibody Add on for maintenance treatment of poorly controlled moderate to severe eosinophilic asthma
The future treatments for asthma is based on the essential idea of personalized medicine Personalised medicine involves seeking the best ratio between efficacy and feasibility using clinical characteristics (called phenotypes ) or guided by biomarkers (called endotypes ) relevant to the underlying pathogenesis of asthma
Endotype- based strategies Phenotype- based strategies Atopic status Th2-orientated therapies Non-Th2- dedicated drugs Cough/sputum Low-dose azithromycin regimen Chronic airway obstruction IL-5 IL-13 GATA3 Aspirin sensitivity
The classification of asthma into phenotypes and endotypes allows for the use of targeted therapies Interleukin-5 is the most important growth, differentiation, and activating factor for human eosinophils Varricchi G, et al. Curr Opin Allergy Clin Immunol (2016) 16:186 200
Phenotyping The only significant exception is the broad division of patients based on the presence or absence of significant eosinophilia The currently available novel/targeted therapies are essentially all directed at the eosinophilic phenotype
Mepolizumab (Nucala) Humanized monoclonal antibody against interleukin-5 (IL-5) Image result for nucala Subcutaneous injection Every 4 week dosing 12 years and older Reduces severe asthma attacks hospitalization prednisone usage GSK May 2016
SIRIUS trial 135 adults with severe eosinophilic asthma on oral glucocorticoids Compared to placebo: Reduction in steroid dose (50%) Reduced exacerbation rate (32%) ACQ score improvement was statistically significant
MENSA trial 576 patients with history of frequent exacerbations randomized to mepolizumab or placebo Statistically significant: Reduction in significant exacerbations (ED/hospitalization) Increase in FEV1 (~100mL), SGRQ and ACQ scores
Reslizumab (Cinqair) Image result for cinqair IV over 20-50 minutes every 4 weeks 18 years and older Severe asthma w/ eosinophilic phenotype Teva Pharmaceuticals / 2016
Targeted therapy with reslizumab appears to be effective and safe in the treatment of adults with severe eosinophilic asthma and represents one step closer to precision medicine.
Reslizumab reduces exacerbation rates and improves lung function and patient-reported outcomes in patients with eosinophilic asthma receiving therapy per Steps 4 and 5 of the GINA guidelines.
Other noteworthy mAb Benralizumab (Benra/AstraZeneca) It is a humanized, anti-eosinophilic monoclonal antibody against IL-5 receptor alfa, which is expressed on the surface of eosinophils and basophils No FDA app.
Change from baseline in FEV1 for patients receiving benralizumab + high-dose ICS/LABA
N Engl J Med. 2017 Jun 22;376(25):2448-2458 Benralizumab showed significant benefits, as compared with placebo, on oral glucocorticoid use and exacerbation rates. These effects occurred without a sustained effect on the FEV1. (Funded by AstraZeneca; ZONDA ClinicalTrials.gov number, NCT02075255.)
Compared to mepolizumab and reslizumab, the possible advantages of benralizumab are less frequent dosing and a potential to reduce exacerbations irrespective of the blood eosinophil count
PLoS ONE 11(11): e0166833. doi:10.1371/journal. Nov 22, 2016 20 RCTs investigating the effect of anti-interleukin 5 monoclonal antibodies in patients with asthma. The results suggest that anti-interleukin 5 therapy was well tolerated and could significantly improve AQLQ score, FEV1, FEV1% of predicted value, and decrease asthmatic exacerbation, blood and sputum eosinophil levels
For asthma, currently available anti-inflammatory agents (GCs and the biological therapeutics anti-IgE, IL-5 or IL-13) target pro- inflammatory mediator pathways Common lung diseases such as asthma and COPD are characterized by unrestrained and chronic inflammation that fails to resolve. Resolution is an active process with highly regulated cellular and biochemical events that terminates acute inflammation. Levy BD, et al. Clin Chest Med. 2012 September ; 33(3): 559 570
Specialised pro-resolving mediators (SPM) (such as lipoxins, protectins, resolvins and maresins) play main role in inflammation resolution including inhibition of neutrophil migration, enhancement of macrophage phagocytosis of apoptotic neutrophils, suppression of pro-inflammatory cytokines and chemokines The majority of individuals with asthma have chronic inflammation of the airways that does not resolve. There is still limited understanding of why the asthmatic airway inflammation fails to resolve. The reduction in pro-resolving activity may be the cause. Duvall MG, et al. Eur J Pharmacol. 2016 August 15; 785: 144 155
Insights into these chemical mediators and their signaling pathways provide an opportunity to develop agonists of resolution as a potential novel class of therapeutics. Thus, bioactive stable analog mimetics of these mediators may offer new therapeutic strategies for asthma and airway inflammation associated diseases. currently under phase I/II study
Further trials are necessary to determine the most effective asthma treatment drug to distinguish which patients will respond to particular treatment Further studies in the context of inflammation resolution is likely to inform potential new avenues for therapeutic intervention in asthma
it has been suggested that targeted anti-eosinophilic strategies may unmask or even accelerate progression of certain tumors in few patients with hypereosinophilic syndrome (71). Therefore, future surveillance and real-life studies will be needed to further confirm the safety of reslizumab in long-term treatment of patients with severe eosinophilic asthma.