Non-Androgenic Male Reproductive Effects of Phthalates
Explore the significance of non-androgenic male reproductive effects caused by phthalates, focusing on fetal testis seminiferous cord effects across various species. Recommendations include studying species with different responses to anti-androgenic effects and investigating mechanistic differences in steroidogenesis. Understanding the long-term consequences of exposure is crucial for developing effective strategies to mitigate risks.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
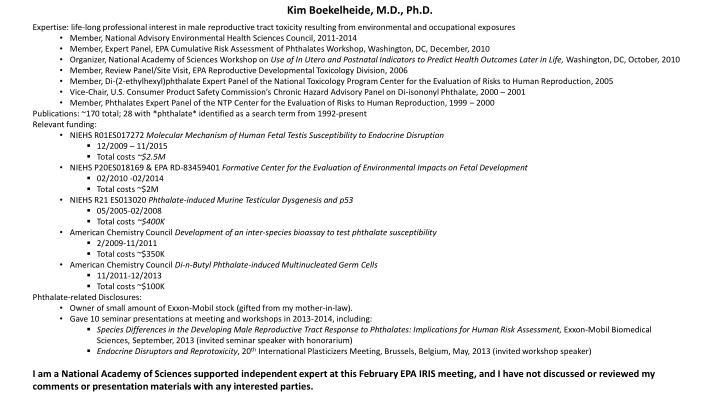
Kim Boekelheide, M.D., Ph.D. Expertise: life-long professional interest in male reproductive tract toxicity resulting from environmental and occupational exposures Member, National Advisory Environmental Health Sciences Council, 2011-2014 Member, Expert Panel, EPA Cumulative Risk Assessment of Phthalates Workshop, Washington, DC, December, 2010 Organizer, National Academy of Sciences Workshop on Use of In Utero and Postnatal Indicators to Predict Health Outcomes Later in Life, Washington, DC, October, 2010 Member, Review Panel/Site Visit, EPA Reproductive Developmental Toxicology Division, 2006 Member, Di-(2-ethylhexyl)phthalate Expert Panel of the National Toxicology Program Center for the Evaluation of Risks to Human Reproduction, 2005 Vice-Chair, U.S. Consumer Product Safety Commission s Chronic Hazard Advisory Panel on Di-isononyl Phthalate, 2000 2001 Member, Phthalates Expert Panel of the NTP Center for the Evaluation of Risks to Human Reproduction, 1999 2000 Publications: ~170 total; 28 with *phthalate* identified as a search term from 1992-present Relevant funding: NIEHS R01ES017272 Molecular Mechanism of Human Fetal Testis Susceptibility to Endocrine Disruption 12/2009 11/2015 Total costs ~$2.5M NIEHSP20ES018169 & EPA RD-83459401 Formative Center for the Evaluation of Environmental Impacts on Fetal Development 02/2010 -02/2014 Total costs ~$2M NIEHS R21 ES013020 Phthalate-induced Murine Testicular Dysgenesis and p53 05/2005-02/2008 Total costs ~$400K American Chemistry Council Development of an inter-species bioassay to test phthalate susceptibility 2/2009-11/2011 Total costs ~$350K American Chemistry Council Di-n-Butyl Phthalate-induced Multinucleated Germ Cells 11/2011-12/2013 Total costs ~$100K Phthalate-related Disclosures: Owner of small amount of Exxon-Mobil stock (gifted from my mother-in-law). Gave 10 seminar presentations at meeting and workshops in 2013-2014, including: Species Differences in the Developing Male Reproductive Tract Response to Phthalates: Implications for Human Risk Assessment, Exxon-Mobil Biomedical Sciences, September, 2013 (invited seminar speaker with honorarium) Endocrine Disruptors and Reprotoxicity, 20th International Plasticizers Meeting, Brussels, Belgium, May, 2013 (invited workshop speaker) I am a National Academy of Sciences supported independent expert at this February EPA IRIS meeting, and I have not discussed or reviewed my comments or presentation materials with any interested parties.
Science Question 5. Relevance of non-androgen related male reproductive effects A consensus has developed that phthalate-induced fetal testis seminiferous cord effects are conserved across species In general, the seminiferous cord effects are less well understood than the anti-androgenic effects o Vulnerable developmental windows of exposure and dose-response are less certain o Consequences of exposure are less certain Potential overlap of effects due to anti-androgenic and seminiferous cord mechanisms o Measures of effect are less certain Multinucleated germ cells (MNGs) are an easily measured biomarker of effect since these end-stage degenerating cells die, they do not inform us regarding later life consequences of exposure MNG induction across various doses and multiple days Heger et al., Environ health Perspect 120:1137 (2012) Recommendations Need studies of species (like mice) with less of an anti-androgenic response o To investigate the mechanistic differences in steroidogenesis across species o To determine later life consequences of seminiferous cord effects Need additional mechanistic studies of human fetal testis response to phthalates
Science Question 4. Use of phthalate mechanistic data A consensus has developed that the phthalate-induced fetal testis anti-androgenic response varies across species, with rats more sensitive than either mice or humans In mice, this relative resistance to phthalate-induced anti-androgenicity has been shown to be pharmacodynamic, not pharmacokinetic C57Bl C57Bl mouse exposure gd 13-17 C3H C57Bl C57Bl Furr et al., Tox Sci 140:403 (2014) In humans, a relative resistance to phthalate-induced anti-androgenicity has been demonstrated with several human fetal testis xenotransplants models and in vitro cultures Xenotransplant model: 500 mg/kg di-n-butyl phthalate daily by gavage for 2 weeks sham (ungrafted) average Spade et al., Tox Sci 138:148 (2014)
Science Question 2. Considering phthalate syndrome effects as a single outcome altered Leydig Cell function altered Sertoli Cell function lowered Testosterone/Insl3 production impaired germ cell development seminiferous cord Decreased sperm production and infertility (Testis germ cell cancer) Reduced Leydig cell function Cryptorchidism/gubernacular malformations Hypospadias/malformed external genitalia Nipple/areolae retention Underdeveloped or absent reproductive organs (Wolffian duct abnormalities) interstitium Sertoli Cells support Germ Cells Leydig Cells produce Testosterone Germ Cells become sperm
Science Question 3. Biologically relevant level of change in testosterone concentration