Oregon Out-of-Hospital Birth Coverage Guidance and Data Overview
"Discover the evidence-based policy considerations and data on out-of-hospital births in Oregon, including attendance statistics, training requirements, and public health data analysis. Explore insights for informed decision-making in planned out-of-hospital births."
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Planned Out-of-Hospital Birth Draft Coverage Guidance for EbGS Consideration April 4, 2019 Center For Evidence-based Policy
Overview Update to 2015 coverage guidance process February 2019: General background Today s meeting: Review of evidence June EbGS meeting: Review of guidelines and discussion of draft coverage recommendations 2 Center For Evidence-based Policy
Background: Out-of-Hospital Birth in Oregon In 2017, planned out-of-hospital births accounted for 1,758 (4.0%) of the 44,160 births in Oregon 60% of out-of-hospital births in the mother s home 40% in freestanding birth centers In addition to the CDC birth certificate question on intention of home birth (planned or unplanned), Oregon House Bill 2380 (2011) adds additional information: Did you go into labor planning to deliver at home or at a freestanding birthing center? 3 Center For Evidence-based Policy
Background: Out-of-Hospital Birth in Oregon Planned Attendant for Planned Out-of-Hospital Births, 2017 Attendant Number Percent Medical Doctors and Doctors of Osteopathy (MD/DO) Naturopathic Physicians (ND) Certified Nurse Midwives (CNM) Licensed Direct-Entry Midwives (LDM) Unlicensed Direct-Entry Midwives Other TOTAL 0 0% 238 548 794 136 42 1,758 14% 31% 45% 8% 2% 100% Other constitutes other family members, friends Planned hospital births, 79% MD/DO attended, 21% attended by CNM Eligible for OHA reimbursement for OOHB: MD/DO, ND, CNM, LDM 4 Center For Evidence-based Policy
Background: Out-of-Hospital Birth in Oregon Training and Licensing Requirements for Birth Attendants Unlicensed Direct-Entry Midwives Licensed Direct- Entry Midwives (LDEMs) Certified Nurse Midwives (CNMs) Naturopathic Doctors (NDs) Osteopathic or Allopathic Doctors (DO/MDs) Accredited Training Program * *or equiv. training Undergraduate Degree Graduate Degree Postgraduate Training Settings Home Home, birth center Home, birth center, hospital Oregon State Board of Nursing Home, birth center Hospital (mostly) Licensing Board None Board of Direct- Entry Midwifery Board of Naturopathic Medicine Oregon Medical Board 5 Center For Evidence-based Policy
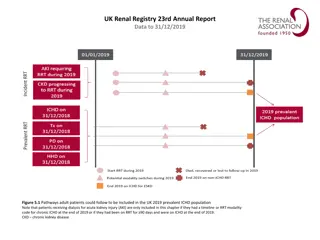
Oregon Public Health Data Case review of 8 fetal and early neonatal deaths among planned out-of-hospital births in 2012 4 fetal, 4 early neonatal 6 of the 8 would not meet current HERC low-risk criteria for coverage of out-of-hospital birth > 41 weeks gestational age (4) Twin pregnancy (2) Morbid obesity (1) No or inadequate prenatal care (2) Pre-existing or pregnancy-related maternal disease (2) 6 Center For Evidence-based Policy
Oregon Public Health Data 2012-2017 review of planned out-of-hospital births Low-risk women: single gestation, no cesarean history, at 37 to 41 weeks gestation Demographics, geography, transfer rates Transfers counted as planned out-of-hospital births Perinatal death: death at 20 weeks to first 6 days of life Birth attendant type not reported 7 Center For Evidence-based Policy
Oregon Public Health Data 1.7 per 1,000 pregnancies for planned in-hospital birth 2.0 per 1,000 pregnancies for planned out-of-hospital birth 8 Center For Evidence-based Policy
Evidence Review Center For Evidence-based Policy
Scope Statement Population Pregnant women Interventions Planned out-of-hospital birth (home or birth center) Comparators Planned birth in a hospital 10 Center For Evidence-based Policy
Scope Statement Critical Outcomes Delivery mode (cesarean, operative vaginal delivery, spontaneous vaginal delivery) Perinatal mortality Serious neonatal morbidity (e.g., seizures, NICU admission, low Apgar scores, hypoxic ischemic encephalopathy, sepsis) Serious maternal harm (e.g., postpartum hemorrhage, serious infection, mortality) Important Outcomes Breastfeeding 11 Center For Evidence-based Policy
Key Questions 1. What is the comparative effectiveness of planned out-of- hospital birth compared to hospital birth? 2. Does the comparative effectiveness of planned out-of-hospital birth vary by: a. Patient characteristics (demographics) b. Risk factors (pregnancy or pre-pregnancy) and comorbidities c. Setting (including home, out-of-hospital birth center) d. Location (U.S. vs. non-U.S.) 12 Center For Evidence-based Policy
Key Questions 3. What are the harms of planned out-of-hospital birth compared to hospital birth? 4. Do the harms of planned out-of-hospital birth vary by: a. Patient characteristics (demographics) b. Risk factors (pregnancy or pre-pregnancy) and comorbidities c. Setting (including home, out-of-hospital birth center) d. Location (U.S. vs. non-U.S.) e. Provider characteristics Contextual questions, guidelines, and policies scheduled for June meeting 13 Center For Evidence-based Policy
Findings Center For Evidence-based Policy
Evidence Sources 42 comparative observational studies 7 U.S. of good (1), fair (2), poor (4) methodological quality 35 Non-U.S. of good (5), fair (9), poor (21) methodological quality 14 noncomparative observational studies, all poor methodological quality 7 U.S. studies 6 non-U.S. studies 1 used combination of Canadian and U.S. data 15 Center For Evidence-based Policy
Evidence Findings- Overview U.S. comparative data U.S. noncomparative data GRADE table with U.S. and non-U.S. comparisons Subgroup findings Limitations 16 Center For Evidence-based Policy
Mode of Delivery: U.S. Studies 2 studies Snowden et al., 2015 (Oregon, 2012 to 2013) Good-quality study Planned home or birth center births (n = 3,804) compared to planned hospital (n = 75,923) Thornton et al., 2017 (43 states, 2006 to 2011) Poor-quality study Planned birth center (n = 8,776) compared to planned hospital delivery (n = 2,527) 17 Center For Evidence-based Policy
Mode of Delivery: U.S. Studies Snowden et al., 2015 Planned home or birth center vs. planned hospital NNT Nonoperative Vaginal Delivery 93.8% vs. 71.9% Adjusted risk difference 27.5, 95% CI 24.9 to 30.2, p < 0.001 3 95% CI, 3 to 4 Cesarean Delivery 5.3% vs. 24.7% Adjusted risk difference -24, 95% CI -26.6 to -21.4, p < 0.001 4 95% CI, 3 to 4 Thornton et al., 2017 Planned birth center vs. planned hospital NNT/NNH Cesarean Delivery 4.14% vs. 4.99% aOR 0.63, 95% CI 0.50 to 0.79, p = not reported NNT 117 NNH: number needed to harm; NNT: number needed to treat 18 Center For Evidence-based Policy
Perinatal or Neonatal Mortality: U.S. 4 studies Grunebaum, McCullough, Arabin et al., 2017 (U.S., 2008 to 2012) Poor-quality study; planned home birth (CNM or other midwife) vs. hospital (midwife) Grunebaum, McCullough, Sapra et al., 2017 (U.S., 2009 to 2013 ) Fair-quality study; all planned home births (n = 96,815) compared to hospital birth (midwife) (n = 1,077,197) Snowden et al., 2015 (Oregon, 2012 to 2013) Good-quality study; planned home or birth center births (n = 3,804) compared to planned hospital (n = 75,923) Thornton et al., 2017 (43 states, 2006 to 2011) Poor-quality study; planned birth center (n = 8,776) compared to planned hospital delivery (n = 2,527) 19 Center For Evidence-based Policy
Perinatal or Neonatal Mortality: U.S. Grunebaum, McCullough, Arabin et al., 2017 Grunebaum, McCullough, Sapra et al., 2017 Snowden, 2015 Planned home vs. planned hospital attended by a midwife NNH Neonatal death 0 to 27 days 2012 to 2013: 0.16% vs. 0.06%, aOR 2.87 (1.10 to 4.30), adjusted risk difference 0.077, 95% CI 0.013 to 0.140 1,298 (714 to 7,692) 2009 to 2013: 0.12% vs. 0.03%, standardized mortality ratio (SMR) 4.13, 95% CI 3.38 to 4.88 1,111 2008 to 2012: 0.127% vs. 0.035% RR 3.62, 95% CI 3 to 4.4 1,087 20 Center For Evidence-based Policy
Perinatal or Neonatal Mortality: US Standardized mortality ratio (SMR): Observed deaths in a study population Expected deaths in a standard population >1: increased risk of death ; < 1: protective For Grunebaum, McCullough, Sapra et al., 2017, standard population is hospital deliveries attended by a midwife Report controlling for age, parity, post-term dates More an adjusted risk ratio than SMR 21 Center For Evidence-based Policy
Perinatal or Neonatal Mortality: U.S. Snowden et al., 2015 Planned home or birth center vs. planned hospital NNH 20 weeks, intrapartum, through 27 days of life 0.39% vs. 0.18% Adjusted risk difference 0.158, 95% CI 0.055 to 0.261, p = 0.003 633 (383 to 1,818) Thornton et al., 2017 Planned birth center vs. planned hospital NNH Intrapartum or newborn death 0.03% vs. 0.04% OR 0.86, 95% CI 0.09 to 8.3, p = 0.99 Calculated RR 0.96, 95% CI 0.54 to 1.70 Not applicable 22 Center For Evidence-based Policy
Neonatal Morbidity: U.S. 3 studies Li et al., 2017 (South Carolina, 2003 to 2013) Poor-quality study Planned home (n = 661) vs. planned birth center (n = 1,233) vs. planned clinic (n = 9) vs. planned hospital (n =547,523) Snowden et al., 2015 (Oregon, 2012 to 2013) Good-quality study Planned home or birth center births (n = 3,804) compared to planned hospital (n = 75,923) Thornton et al., 2017 (43 states, 2006 to 2011) Poor-quality study Planned birth center (n = 8,776) compared to planned hospital delivery (n = 2,527) 23 Center For Evidence-based Policy
Neonatal Morbidity: U.S. Snowden et al., 2015 Li et al., 2017 Planned home or birth center vs. planned hospital NNH or NNT NICU Admission 1.7% vs. 2.9% Adjusted risk difference: 0.85 less, 95% CI -1.57 to -0.14, NNT = 117 Apgar < 4 0.6% vs. 0.4% Adjusted risk difference: 0.18 more, 95% CI 0.00 to 0.37 Not applicable Apgar < 7 (Both at 5 minutes) 2.3% vs. 1.8% Adjusted risk difference: 0.50 more, 95% CI 0.07 to 0.93 NNH =200 107 to 1,428 Neonatal Seizures 0.13% vs. 0.04% Adjusted risk difference; 0.07 more, 95% CI 0.02 to 0.13 NNH = 1,428 Seizures: 0.05% vs. 0.02%; Calculated RR 2.2, 0.3 to 15.77 Convulsions: 0.37% vs. 0.23%; Calculated RR 1.57, 95% CI 0.74 to 3.2 Not applicable 24 Center For Evidence-based Policy
Neonatal Morbidity: U.S. Snowden et al., 2015 Li et al., 2017 Planned home or birth center vs. planned hospital NNH or NNT Ventilator Support 3.8% vs. 3.3% Adjusted risk difference 0.97 to 1.05 aOR 1.36, 95% CI 1.14 to 1.62 NNH = 95 to 113 25 Center For Evidence-based Policy
Neonatal Morbidity: U.S. Thornton et al., 2017 Planned birth center vs. planned hospital NNH or NNT Apgar score 3 to 7 (at 5 minutes) Not applicable aOR 1.60, 95% CI 0.82 to 3.16 Composite (mortality, hypoxic injury, low Apgar, seizure, respiration support, and meconium aspiration syndrome) Not applicable aOR 1.44, 95% CI 0.95 to 1.82 Short-term positive pressure ventilation < 10 minutes aOR 1.31, 95% CI 0.95 to 1.82 Not applicable 26 Center For Evidence-based Policy
Maternal Harm: U.S. 2 studies Snowden et al., 2015 (Oregon, 2012 to 2013) Good-quality study Planned home or birth center births (n = 3,804) compared to planned hospital (n = 75,923) Thornton et al., 2017 (43 states, 2006 to 2011) Poor-quality study Planned birth center (n = 8,776) compared to planned hospital delivery (n = 2,527) 27 Center For Evidence-based Policy
Maternal Harm: U.S. Studies Snowden et al., 2015 Planned home or birth center vs. planned hospital NNT/NNH Third or fourth degree perineal laceration 0.9% vs. 1.3% adjusted risk difference 0.54 less, 95% CI 0.98 to 0.11, p = 0.02 NNT: 185 (102 to 909) Blood transfusion 0.6% vs. 0.4% adjusted risk difference 0.27 more, 95% CI 0.08 to 0.46, p = 0.006 NNH: 370 (217 to 1,250) Thornton et al., 2017 Planned birth center vs. planned hospital NNT/NNH Postpartum Hemorrhage (no volume definition) 4.63% vs. 6.18% aOR 1.25, 95% CI 0.99 to 1.58 Not applicable 28 Center For Evidence-based Policy
Breastfeeding: U.S. 2 studies MacDorman & Declercq, 2016 (U.S., 2004 to 2014) Poor-quality study Planned home (n = 29,021) vs. planned birth center (n = 18,047) vs. planned hospital birth (n = 3,773,115) Thornton et al., 2017 (43 states, 2006 to 2011) Poor-quality study Planned birth center (n = 8,776) compared to planned hospital delivery (n = 2,527) 29 Center For Evidence-based Policy
Breastfeeding: U.S. Studies MacDorman & Declercq, 2016 Planned home vs. planned birth center vs. planned hospital NNT/NNH Breastfeeding initiation 97.9% vs. 98.1% vs. 80.8% NNT 4 to 5 Thornton, 2017 Planned birth center vs. planned hospital NNT Breastfeeding at discharge 94.5% vs. 72.2% aOR 9.12, 95% CI 7.45 to 11.16 4 30 Center For Evidence-based Policy
Evidence: Noncomparative Studies High levels of heterogeneity in the outcomes reported Many studies excluded high-risk populations High rates of unassisted vaginal deliveries across studies Studies generally reported greater risks of maternal and neonatal harms for nulliparous women and women with a previous history of cesarean or instrument-assisted vaginal delivery Breech presentation, multiple gestation, and high-risk maternal conditions (e.g., hypertension) were associated with higher risks of adverse neonatal events 31 Center For Evidence-based Policy
GRADE Table Findings GRADE table includes only fair- to good-quality studies U.S.-based evidence reported separately from non-U.S Strength of evidence reflects all studies Center For Evidence-based Policy
GRADE Table Planned home or birth center vs. Planned hospital U.S. Studies Non-U.S. Studies Nonoperative Vaginal Delivery 1 study 93.8% vs. 71.9% RD= 27.5 more NNT = 3 aOR 5.63, 95% CI 4.84 to 6.55 3 studies 81% to 92.8% vs. 64.7% to 86% RD = 3.0 to 19.0 NNT range from 5 to 33 aOR range from 1.57 to 3.61 Cesarean Delivery 1 study 5.3% vs. 24.7% RD = 19.4 more NNT = 5 aOR = 0.18, 95% CI 0.16 to 0.22 2 studies 2.8% to 4.0% vs. 11.1% to 11.7% RD range from 7.6 to 8.3 more NNT range from 12 to 13 aOR range from 0.31 to 0.76 33 Center For Evidence-based Policy
GRADE Table: Mode of Delivery Low confidence that planned out-of-hospital birth is associated with improved delivery mode outcome compared to planned in-hospital birth, based on 4 good- or fair-methodological-quality observational studies, 1 from U.S. 34 Center For Evidence-based Policy
GRADE Table Planned home or birth center vs. Planned hospital U.S. Studies Non-U.S. Studies Perinatal or Neonatal Mortality Neonatal death from 0 to 27 days (2 studies) 0.12% to 0.16% vs. 0.03% to 0.06% RD from 0.09 to 0.1 more NNH range from 1,111 to 1,000 SMR 4.13, 95% CI 3.38 to 4.88; aOR 2.87, 95% CI 1.10 to 7.47 Intrapartum or neonatal death from 0 to 7 days (2 studies) 0.06% to 0.15% vs. 0.01% to 0.18% Adjusted odds ratios not statistically significant across both studies Perinatal death ( 20 weeks through 27 days of life) (1 study) 0.39% vs. 0.18%; RD = 0.15, NNH= 666; aOR 2.43, 95% CI 1.37 to 4.30 35 Center For Evidence-based Policy
GRADE Table: Perinatal or Neonatal Mortality Very low confidence that planned out-of-hospital birth is associated with increase perinatal or neonatal mortality, based on 4 good- or fair-quality observational studies, 2 from U.S. 36 Center For Evidence-based Policy
GRADE Table: Neonatal Morbidity Planned home or birth center vs. Planned hospital U.S. Studies Non-U.S. Studies Apgar < 7 at 5 minutes 1 study (Oregon) 2.3% vs. 1.8% aOR = 1.31, 95% CI 1.04 to 1.66 1 study 1.2% vs. 2.8% aOR 0.57, 95% CI 0.25 to 1.35 1 study (Oregon) 0.6% vs. 0.4% aOR = 1.56, 95% CI 0.98 to 2.47 No non-U.S. studies reported this outcome Apgar < 4 at 5 minutes 37 Center For Evidence-based Policy
GRADE Table: Neonatal Morbidity Planned home or birth center birth vs. Planned hospital birth U.S. Studies Non-U.S. Studies Neonatal Seizures 1 study (Oregon) 0.13% vs. 0.04% RD 0.06 to 0.07 (2 different methods) NNH 1,428 to 1,666 aOR 3.60, 95% CI 1.36 to 9.50 No non-U.S. studies reported this outcome 38 Center For Evidence-based Policy
GRADE Table: Neonatal Morbidity Planned home or birth center birth vs. Planned hospital birth U.S. Studies Non-U.S. Studies Birthplace Composite (stillbirth after onset of labor care, neonatal death 0 to 7 days, neonatal encephalopathy, meconium aspiration syndrome, brachial plexus injury, fractured humerus or clavicle) No U.S. studies reported this outcome 2 studies 0.05% to 3.5% for planned home or birth center birth vs. 0.05% to 4.4% for planned hospital birth Adjusted odds ratios not statistically significantly different across both studies 39 Center For Evidence-based Policy
GRADE Table: Neonatal Morbidity Planned home or birth center birth vs. Planned hospital birth U.S. Studies Non-U.S. Studies NICU Admission 1 study 1.7% vs. 2.9% RD = 0.95 to 0.85 less NNT = 105 to 117 aOR 0.71, 95% CI 0.55 to 0.92 No non-U.S. studies reported this outcome Ventilator Support 1 study 3.8% vs. 3.3% RD: 0.97 to 1.05 more NNH = 95 to 103 aOR 1.36, 95% CI 1.14 to 1.62 No non-U.S. studies reported this outcome 40 Center For Evidence-based Policy
GRADE Table: Neonatal Morbidity Very low confidence that planned out-of-hospital birth associated with increased neonatal morbidity, based on 4 good- or fair-quality observational studies, 1 from U.S. 41 Center For Evidence-based Policy
GRADE Table: Maternal Harm Planned home or birth center birth vs. Planned hospital birth U.S. Studies Non-U.S. Studies Postpartum hemorrhage of 1000 ml No U.S. studies of this outcome 4 studies 0.38% to 29.2% vs. 1.04% to 39.9% Range of finding across 3 with analysis aOR =0.88, 95% CI 0.52 to 1.47 aRR 1.10, 95% CI 0.67 to 1.79 aOR =0.4, 95% CI 0.3 to 0.6 Blood transfusion 1 study 0.6% vs. 0.4% RD 0.27 to 0.28 more NNH = 357 to 370 aOR 1.91, 95% CI 1.25 to 2.93 1 study Home 0.5% vs. Hospital 1.2% aOR 0.72, 95% CI 0.47 to 1.12 Birth center 0.6% vs. Hospital 1.2% RD 0.6 less, NNT =166 aOR 0.48, 95% CI 0.32 to 0.73 42 Center For Evidence-based Policy
GRADE Table: Maternal Harm Estimate of Effect for Outcome/Confidence in Estimate U.S. Studies Non-U.S. Studies Third or fourth degree perineal laceration 1 study 2 studies 0.9% vs. 1.3% 1.9% to 4.9% vs. 3.2% to 4.2% RD to 0.45 to 0.54 less RD 0.45 to 0.54 less NNT = 185, adjusted 222 NNT = 76 to 166 aOR 0.69 (95% CI 0.49 to 0.98) aOR 0.77, 95% CI 0.57 to 1.05 to aOR 0.90, 95% CI 0.56 to 1.45 43 Center For Evidence-based Policy
GRADE Table: Maternal Harm Very low confidence that planned out-of-hospital birth associated with less risk of third or fourth degree lacerations compared to planned in-hospital birth, evidence on risk of blood transfusion was conflicting (increased in U.S, similar or less from non-U.S. studies), and no U.S. findings on post-partum hemorrhage based on 5 good- or fair-quality observational studies, 1 from U.S.) 44 Center For Evidence-based Policy
GRADE Table: Breastfeeding Estimate of Effect for Outcome/Confidence in Estimate U.S. Studies Non-U.S. Studies No U.S. studies with long-term outcomes identified Exclusive breastfeeding at 6 months postpartum 4% to 22% for planned home or birth center birth vs. 1% to 9% for planned hospital birth ARD = 3 to 13 NNT = 7 to 33 aOR 2.24, 95% CI 1.14 to 4.03 (very low confidence that exclusive breastfeeding at 6 months was more common for planned home or birth center birth compared to planned home birth, based on 1 fair-quality observational study) 45 Center For Evidence-based Policy
Subgroup Considerations Center For Evidence-based Policy
2015 CG High-Risk Groups: Prior Cesarean Delivery 2 U.S. Studies Grunebaum, McCullough, Sapra et al., 2017 (fair quality); Tilden et al., 2017 (fair quality) Grunebaum, McCullough, Sapra et al., 2017 Planned home vs. planned hospital NNH Neonatal death 0 to 27 days Women with a prior cesarean delivery SMR 8.33, 95% CI 2.59 to 14.07 Not able to calculate 47 Center For Evidence-based Policy
2015 CG High-Risk Groups: Prior Cesarean Delivery Tilden, 2017 Planned home or birth center vs. planned hospital NNH or NNT NICU Admission 1.11% vs. 3.10%, aOR 0.40, 95% CI 0.29 to 0.57, p < 0.001 NNT =50 Apgar < 4 0.73% vs. 0.40%, aOR 1.77, 95% CI 1.12 to 2.79, p = 0.016 NNH = 303 Apgar < 7 (both at 5 minutes) 4.42% vs. 2.68%, aOR 1.62, 95% CI 1.35 to 1.96, p < 0.001 NNH = 57 Neonatal Seizures 0.19% vs. 0.02%, aOR 8.53, 95% CI 2.87 to 25.4, p = 0.003 NNH = 588 Ventilator Support 0.38% vs. 0.29%, aOR 1.36, 95% CI 0.75 to 2.46, p = 0.31 Not applicable Neonatal Mortality 0.13% vs. 0.08%, aOR 2.10, 95% CI 0.73 to 6.05, p > 0.05 Not applicable 48 Center For Evidence-based Policy
2015 CG High-Risk Groups: Breech Position Fair-quality study conducted in the U.S. (Grunebaum, McCullough, Sapra et al., 2017) Breech presentation: SMR 8.14, 95% 2.17 to 14.11 Cephalic presentation: SMR 3.61, 95% CI 2.92 to 4.31 49 Center For Evidence-based Policy
Additional Subpopulations: Parity, Gestational Age, Maternal Age 2 studies Grunebaum, McCullough, Sapra et al., 2017, U.S., 2009 to 2013 Fair-quality Neonatal death (0 to 27 days) all planned home vs. hospital (midwife attended) Grunebaum, McCullough, Arabin et al., 2017, U.S., 2008 to 2012 Poor-quality Neonatal death (0 to 27 days) planned home birth group (attended by a certified nurse or other midwife) vs. hospital (midwife attended) 50 Center For Evidence-based Policy