OSHA Emergency Temporary Standard - Protecting Healthcare Workers
OSHA has issued an Emergency Temporary Standard to protect healthcare workers from occupational exposure to COVID-19. Covered employers must develop a COVID-19 plan and implement measures to control hazards in the workplace, including patient screening, vaccination encouragement, PPE use, physical distancing, and more.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
COVID-19 INFECTION CONTROL & PREVENTION OSHA EMERGENCY TEMPORARY STANDARC REQUIRED EMPLOYEE TRAINING 7/6/2021
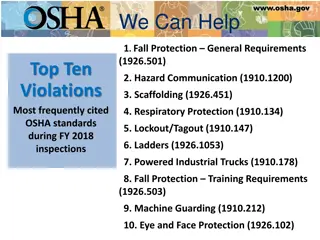
OSHA EMERGENCY TEMPORARY STANDARD THE OCCUPATIONAL SAFETY AND HEALTH ADMINISTRATION (OSHA) IS ISSUING AN EMERGENCY TEMPORARY STANDARD (ETS) TO PROTECT HEALTHCARE AND HEALTHCARE SUPPORT SERVICE WORKERS FROM OCCUPATIONAL EXPOSURE TO COVID-19 IN SETTINGS WHERE PEOPLE WITH COVID-19 ARE REASONABLY EXPECTED TO BE PRESENT. DURING THE PERIOD OF THE EMERGENCY STANDARD, COVERED HEALTHCARE EMPLOYERS MUST DEVELOP AND IMPLEMENT A COVID-19 PLAN TO IDENTIFY AND CONTROL COVID-19 HAZARDS IN THE WORKPLACE. COVERED EMPLOYERS MUST ALSO IMPLEMENT OTHER REQUIREMENTS TO REDUCE TRANSMISSION OF COVID-19 IN THEIR WORKPLACES, RELATED TO THE FOLLOWING: PATIENT SCREENING AND MANAGEMENT THE STANDARD ENCOURAGES VACCINATION BY REQUIRING EMPLOYERS TO PROVIDE REASONABLE TIME AND PAID LEAVE FOR EMPLOYEE VACCINATIONS AND ANY SIDE EFFECTS. STANDARD AND TRANSMISSION-BASED PRECAUTIONS PERSONAL PROTECTIVE EQUIPMENT (PPE) INCLUDING FACEMASKS OR RESPIRATORS IT ALSO ENCOURAGES USE OF RESPIRATORS, WHERE RESPIRATORS ARE USED IN LIEU OF REQUIRED FACEMASKS, BY INCLUDING A MINI RESPIRATORY PROTECTION PROGRAM THAT APPLIES TO SUCH USE. CONTROLS FOR AEROSOL-GENERATING PROCEDURES PHYSICAL DISTANCING OF AT LEAST SIX FEET FINALLY, THE STANDARD EXEMPTS FROM COVERAGE CERTAIN WORKPLACES WHERE ALL EMPLOYEES ARE FULLY VACCINATED AND INDIVIDUALS WITH POSSIBLE COVID-19 ARE PROHIBITED FROM ENTRY; AND IT EXEMPTS FROM SOME OF THE REQUIREMENTS OF THE STANDARD FULLY VACCINATED EMPLOYEES IN WELL-DEFINED AREAS WHERE THERE IS NO REASONABLE EXPECTATION THAT INDIVIDUALS WITH COVID-19 WILL BE PRESENT. WHEN FEASIBLE; PHYSICAL BARRIERS CLEANING AND DISINFECTION VENTILATION; HEALTH SCREENING AND MEDICAL MANAGEMENT TRAINING ANTI-RETALIATION RECORDKEEPING; AND REPORTING.
OSHA EXECUTIVE ORDER OSHA SHALL ISSUE AN ETS IF THE AGENCY DETERMINES THAT EMPLOYEES ARE EXPOSED TO GRAVE DANGER FROM EXPOSURE TO SUBSTANCES OR AGENTS DETERMINED TO BE TOXIC OR PHYSICALLY HARMFUL OR FROM NEW HAZARDS, AND AN ETS IS NECESSARY TO PROTECT EMPLOYEES FROM SUCH DANGER. FOR THE FIRST TIME IN ITS 50-YEAR HISTORY, OSHA FACES A NEW HAZARD SO GRAVE THAT IT HAS KILLED NEARLY 600,000 START PRINTED PAGE 32377PEOPLE IN THE UNITED STATES IN BARELY OVER A YEAR, AND INFECTED MILLIONS MORE (CDC, MAY 24, 2021A). AND THE IMPACT OF THIS NEW ILLNESS HAS BEEN BORNE DISPROPORTIONATELY BY THE HEALTHCARE AND HEALTHCARE SUPPORT WORKERS TASKED WITH CARING FOR THOSE INFECTED BY THIS DISEASE. AS OF MAY 24, 2021, OVER 491,816 HEALTHCARE WORKERS HAVE CONTRACTED COVID-19, AND MORE THAN 1,600 OF THOSE WORKERS HAVE DIED (CDC, MAY 24, 2021B). OSHA HAS DETERMINED THAT EMPLOYEE EXPOSURE TO THIS NEW HAZARD, SARS-COV-2 (THE VIRUS THAT CAUSES COVID-19), PRESENTS A GRAVE DANGER TO WORKERS IN ALL HEALTHCARE SETTINGS IN THE UNITED STATES AND ITS TERRITORIES WHERE PEOPLE WITH COVID-19 ARE REASONABLY EXPECTED TO BE PRESENT. THIS FINDING OF GRAVE DANGER IS BASED ON THE SCIENCE OF HOW THE VIRUS SPREADS AND THE ELEVATED RISK IN WORKPLACES WHERE COVID-19 PATIENTS ARE CARED FOR, AS WELL AS THE ADVERSE HEALTH EFFECTS SUFFERED BY THOSE DIAGNOSED WITH COVID-19, AS DISCUSSED IN GRAVE DANGER (SECTION IV.A. OF THIS PREAMBLE). OSHA HAS ALSO DETERMINED THAT AN ETS IS NECESSARY TO PROTECT HEALTHCARE AND HEALTHCARE SUPPORT EMPLOYEES IN COVERED HEALTHCARE SETTINGS FROM EXPOSURES TO SARS-COV-2, AS DISCUSSED IN NEED FOR THE ETS (SECTION IV.B. OF THIS PREAMBLE). WORKERS FACE A PARTICULARLY ELEVATED RISK OF EXPOSURE TO SARS-COV-2 IN SETTINGS WHERE PATIENTS WITH SUSPECTED OR CONFIRMED COVID-19 RECEIVE TREATMENT OR WHERE PATIENTS WITH UNDIAGNOSED ILLNESSES COME FOR TREATMENT (E.G., EMERGENCY ROOMS, URGENT CARE CENTERS), ESPECIALLY WHEN PROVIDING CARE OR SERVICES DIRECTLY TO THOSE PATIENTS. THROUGH ITS ENFORCEMENT EFFORTS TO DATE, OSHA HAS ENCOUNTERED SIGNIFICANT OBSTACLES, REVEALING THAT EXISTING STANDARDS, REGULATIONS, AND THE OSH ACT'S GENERAL DUTY CLAUSE ARE INADEQUATE TO ADDRESS THE COVID-19 HAZARD FOR EMPLOYEES COVERED BY THIS ETS. THE AGENCY HAS DETERMINED THAT A COVID-19 ETS IS NECESSARY TO ADDRESS THESE INADEQUACIES.
HOW CORONAVIRUS SPREADS PERSON-TO-PERSON SPREAD THE VIRUS IS THOUGHT TO SPREAD MAINLY FROM PERSON-TO-PERSON. BETWEEN PEOPLE WHO ARE IN CLOSE CONTACT WITH ONE ANOTHER (WITHIN ABOUT 6 FEET). THROUGH RESPIRATORY DROPLETS PRODUCED WHEN AN INFECTED PERSON COUGHS OR SNEEZES. THESE DROPLETS CAN LAND IN THE MOUTHS OR NOSES OF PEOPLE WHO ARE NEARBY OR POSSIBLY BE INHALED INTO THE LUNGS. CAN SOMEONE SPREAD THE VIRUS WITHOUT BEING SICK? PEOPLE ARE THOUGHT TO BE MOST CONTAGIOUS WHEN THEY ARE MOST SYMPTOMATIC (THE SICKEST). SOME SPREAD MIGHT BE POSSIBLE BEFORE PEOPLE SHOW SYMPTOMS; THERE HAVE BEEN REPORTS OF THIS OCCURRING WITH THIS NEW CORONAVIRUS, BUT THIS IS NOT THOUGHT TO BE THE MAIN WAY THE VIRUS SPREADS. SPREAD FROM CONTACT WITH CONTAMINATED SURFACES OR OBJECTS IT MAY BE POSSIBLE THAT A PERSON CAN GET COVID-19 BY TOUCHING A SURFACE OR OBJECT THAT HAS THE VIRUS ON IT AND THEN TOUCHING THEIR OWN MOUTH, NOSE, OR POSSIBLY THEIR EYES, BUT THIS IS NOT THOUGHT TO BE THE MAIN WAY THE VIRUS SPREADS.
ALL EMPLOYEE PRE-SHIFT SCREENING PROCESS THE EMPLOYEE WILL BE ASKED TO IMMEDIATELY PLACE A MASK ON AND SANITIZE THEIR HANDS ALL EMPLOYEES WILL BE SCREENED PRIOR TO ALLOWING YOU TO PASS THROUGH THE ENTRY CHECKPOINT. EMPLOYEES WILL NOT BE ABLE TO PASS ENTRY CHECKPOINT UNTIL SCREENING IS COMPLETED AND THEY ARE NEGATIVE FOR SYMPTOMS OR FEVER HAVE EMPLOYEE ANSWER ALL QUESTIONS/ SCREEN FOR SYMPTOMS OF RESPIRATORY ILLNESS AND TAKE THE EMPLOYEES TEMPERATURE. IF EMPLOYEE ANSWERS NO TO ALL SCREENING QUESTIONS, THE SCREENER SHOULD ALLOW THE EMPLOYEE TO PROCEED PAST THE CHECKPOINT AREA. EMPLOYEE MAY BEGIN WORK SHIFT. ALL EMPLOYEES MUST WEAR A MASK WITH THE NOSE PINCHED THROUGHOUT THEIR SHIFT. IF EMPLOYEE ANSWERS YES TO ANY OF THE SCREENING QUESTIONS THE EMPLOYEE SHOULD IMMEDIATELY BE ASKED TO LEAVE THE FACILITY TO SELF-ISOLATE AT HOME AND CONTACT THEIR SUPERVISOR AND INFECTION PREVENTIONIST FOR FURTHER DIRECTION. INFECTION PREVENTIONIST SHOULD NOTIFY THE LOCAL HEALTH DEPARTMENT AS REQUIRED. IF DEVELOPING ANY NEW SYMPTOMS (COUGH, SHORTNESS OF BREATH, FEVER) PLEASE DO THE FOLLOWING: IF AT WORK: IMMEDIATELY STOP DIRECT PATIENT CARE, PERFORM HAND HYGIENE, ENSURE YOU HAVE YOUR A MASK ON , NOTIFY YOUR SUPERVISOR AND INFECTION PREVENTIONIST GO HOME AND SELF ISOLATE. INFECTION PREVENTIONIST WILL IDENTIFY INDIVIDUALS OR EQUIPMENT YOU MAY HAVE BEEN IN CONTACT WITH FOR DISINFECTING AND DISCUSSION OF CONTACT. IF AT HOME: STAY HOME, SELF-ISOLATE AND LET YOUR MANAGER KNOW YOU ARE NOT COMING TO WORK. IF YOUR CONDITION WORSENS CONSULT A MEDICAL PROFESSIONAL. THE INFECTION PREVENTIONIST WILL PROVIDE FURTHER DIRECTION FOR TESTING AND MONITORING SYMPTOMS.
RETURN TO WORK INFORMATION FOR EMPLOYEES IF EXPERIENCING SYMPTOMS OR YOU HAVE HAD A EXPOSURE TO SOMEONE THAT HAS TESTED POSITIVE FOR COVID-19 PLEASE CALL THE FACILITY INFECTION PREVENTIONIST FOR DIRECTION AND DISCUSSION ABOUT THE MOST CURRENT RETURN TO WORK GUIDLEINES SET FORTH BY THE CDC AND IDPH
STANDARD AND TRANSMISSION BASED PRECAUTIONS RESPIRATORY HYGIENE/COUGH ETIQUETTE
STANDARD AND TRANSMISSION BASED PRECAUTIONS RESPIRATORY HYGIENE/COUGH ETIQUETTE ENVIRONMENTAL CLEANING AND DISINFECTION REPROCESSING OF REUSABLE RESIDENT MEDICAL EQUIPMENT (E.G., CLEANING AND DISINFECTION OF GLUCOMETERS PER DEVICE AND DISINFECTANT MANUFACTURER S INSTRUCTIONS FOR USE)
STANDARD AND TRANSMISSION BASED PRECAUTIONS RESPIRATORY HYGIENE/COUGH ETIQUETTE ALL STAFF MUST WEAR MASKS AT ALL TIMES WHILE IN THE FACILITY DURING THIS COVID-19 PANDEMIC. THE FACEMASK SHOULD BE REMOVED AND DISCARDED IF SOILED, DAMAGED, OR HARD TO BREATHE THROUGH. IF THE COUNTY COVID RATE RISES ABOVE 5% FACEMASKS AND EYE PROTECTION ARE REQUIRED AT ALL TIMES IN PATIENT CARE AREAS. TAKE CARE NOT TO TOUCH THEIR FACEMASK. IF YOU TOUCH OR ADJUST THEIR FACEMASK THEY MUST IMMEDIATELY PERFORM HAND HYGIENE. LEAVE THE PATIENT CARE AREA IF THEY NEED TO REMOVE THE FACEMASK. COVER YOUR MOUTH AND NOSE WITH A TISSUE WHEN COUGHING OR SNEEZING USE IN THE NEAREST WASTE RECEPTACLE TO DISPOSE OF THE TISSUE AFTER USE PERFORM HAND HYGIENE (E.G., HAND WASHING WITH NON-ANTIMICROBIAL SOAP AND WATER, ALCOHOL-BASED HAND RUB, OR ANTISEPTIC HANDWASH) AFTER HAVING CONTACT WITH RESPIRATORY SECRETIONS AND CONTAMINATED OBJECTS/MATERIALS
TRANSMISSION-BASED PRECAUTIONS UTILIZE APPROPRIATE TRANSMISSION-BASED PRECAUTIONS: FOR A RESIDENT ON CONTACT PRECAUTIONS: STAFF MUST DON GLOVES AND ISOLATION GOWN BEFORE CONTACT WITH THE RESIDENT AND/OR HIS/HER ENVIRONMENT FOR A RESIDENT ON DROPLET PRECAUTIONS: STAFF MUST DON A FACEMASK WITHIN SIX FEET OF A RESIDENT, AND DON GLOVES AND ISOLATION GOWN BEFORE CONTACT WITH THE RESIDENT AND/OR HIS/HER ENVIRONMENT FOR A RESIDENT WITH AN UNDIAGNOSED RESPIRATORY INFECTION: STAFF MUST FOLLOW STANDARD, CONTACT, AND DROPLET PRECAUTIONS (I.E., FACEMASK, GLOVES, ISOLATION GOWN) WITH EYE PROTECTION WHEN CARING FOR A RESIDENT UNLESS THE SUSPECTED DIAGNOSIS REQUIRES AIRBORNE PRECAUTIONS (E.G., TUBERCULOSIS) FOR A RESIDENT WITH KNOWN OR SUSPECTED COVID-19: STAFF WEAR GLOVES, ISOLATION GOWN, EYE PROTECTION, AND AN N95 OR HIGHER-LEVEL RESPIRATOR IF AVAILABLE. A FACEMASK IS AN ACCEPTABLE ALTERNATIVE IF A RESPIRATOR IS NOT AVAILABLE. ADDITIONALLY, AT THIS TIME DUE TO COVID-19 INCREASING COMMUNITY TRANSMISSION, STAFF MUST PRACTICE UNIVERSAL USE OF FACEMASKS WHILE IN THE FACILITY (BASED ON AVAILABILITY). WHEN COVID-19 IS IDENTIFIED IN THE FACILITY, STAFF MUST WEAR ALL RECOMMENDED PPE (I.E., GLOVES, GOWN, EYE PROTECTION AND RESPIRATOR OR FACEMASK) FOR THE CARE OF ALL RESIDENTS ON THE UNIT (OR FACILITY-WIDE BASED ON THE LOCATION OF AFFECTED RESIDENTS), REGARDLESS OF SYMPTOMS (BASED ON AVAILABILITY). DEDICATED OR DISPOSABLE NONCRITICAL RESIDENT-CARE EQUIPMENT (E.G., BLOOD PRESSURE CUFFS, BLOOD GLUCOSE MONITOR EQUIPMENT) IS USED, OR IF NOT AVAILABLE, THEN STAFF MUST CLEAN EQUIPMENT AND DISINFECT ACCORDING TO MANUFACTURERS INSTRUCTIONS USING AN EPA-REGISTERED DISINFECTANT FOR HEALTHCARE SETTING PRIOR TO USE ON ANOTHER RESIDENT OBJECTS AND ENVIRONMENTAL SURFACES THAT ARE TOUCHED FREQUENTLY AND IN CLOSE PROXIMITY TO THE RESIDENT (E.G., BED RAILS, OVER-BED TABLE, BEDSIDE COMMODE, LAVATORY SURFACES IN RESIDENT BATHROOMS) ARE CLEANED AND DISINFECTED WITH AN EPA-REGISTERED DISINFECTANT FOR HEALTHCARE SETTING (EFFECTIVE AGAINST THE ORGANISM IDENTIFIED IF KNOWN) AT LEAST DAILY AND WHEN VISIBLY SOILED SIGNAGE ON THE USE OF SPECIFIC PPE (FOR STAFF) ARE POSTED IN APPROPRIATE LOCATIONS IN THE FACILITY (E.G., OUTSIDE OF A RESIDENT S ROOM, WING, AND/OR FACILITY-WIDE) PLEASE ASK THE DON OR EXECUTIVE DIRECTOR IF YOU HAVE ANY QUESTIONS ABOUT PROCESSES/PROTOCOLS FOR TRANSMISSION-BASED PRECAUTIONS INTERDISCIPLINARY TEAM MEMBERS WILL PERFORM TBC OBSERVATION MONITORING FOR COMPLIANCE.
TRANSMISSION-BASED PRECAUTIONS AEROSOL GENERATING PROCEDURES SOME PROCEDURES PERFORMED ON RESIDENTS WITH KNOWN OR SUSPECTED COVID-19 COULD GENERATE INFECTIOUS AEROSOLS (I.E., AEROSOL GENERATING PROCEDURES (AGPS)). IN PARTICULAR, PROCEDURES THAT ARE LIKELY TO INDUCE COUGHING (E.G., SPUTUM INDUCTION, OPEN SUCTIONING OF AIRWAYS) SHOULD BE PERFORMED CAUTIOUSLY. DISCUSS NECESSITY AND ALTERNATIVE TREATMENT OF THESE ORDERS WITH PHYSICIAN AND IF PERFORMED, THE FOLLOWING MUST OCCUR: STAFF IN THE ROOM SHOULD WEAR AN N95 OR HIGHER-LEVEL RESPIRATOR, EYE PROTECTION, GLOVES, AND AN ISOLATION GOWN. THE NUMBER OF STAFF PRESENT DURING THE PROCEDURE SHOULD BE LIMITED TO ONLY THOSE ESSENTIAL FOR RESIDENT CARE AND PROCEDURE SUPPORT. AGPS SHOULD IDEALLY TAKE PLACE IN AN AIRBORNE INFECTION ISOLATION ROOM (AIIR). IF AN AIIR IS NOT AVAILABLE AND THE PROCEDURE IS MEDICALLY NECESSARY, THEN IT SHOULD TAKE PLACE IN A PRIVATE ROOM WITH THE DOOR CLOSED. CLEAN AND DISINFECT THE ROOM SURFACES PROMPTLY AND WITH APPROPRIATE DISINFECTANT. USE DISINFECTANTS ON LIST N OF THE EPA THE FACILITY HAS VERIFIED THAT WE ARE USING APPROPRIATE CLEANERS AND DISINFECTANTS ON THE WEBSITE FOR EPA-REGISTERED DISINFECTANTS THAT HAVE QUALIFIED UNDER EPA S EMERGING VIRAL PATHOGENS PROGRAM FOR USE AGAINST SARS-COV-2 OR OTHER NATIONAL RECOMMENDATIONS
ENVIRONMENTAL CLEANING AND DISINFECTION DEFINITIONS CLEANING REFERS TO THE REMOVAL OF DIRT AND IMPURITIES, INCLUDING GERMS, FROM SURFACES. CLEANING ALONE DOES NOT KILL GERMS. BUT BY REMOVING THE GERMS, IT DECREASES THEIR NUMBER AND THEREFORE ANY RISK OF SPREADING INFECTION. DISINFECTING WORKS BY USING CHEMICALS TO KILL GERMS ON SURFACES. THIS PROCESS DOES NOT NECESSARILY CLEAN DIRTY SURFACES OR REMOVE GERMS. BUT KILLING GERMS REMAINING ON A SURFACE AFTER CLEANING FURTHER REDUCES ANY RISK OF SPREADING INFECTION.
ENVIRONMENTAL CLEANING AND DISINFECTION USE APPROPRIATE HAND HYGIENE, PPE (E.G., GLOVES), AND ISOLATION PRECAUTIONS DURING CLEANING AND DISINFECTING PROCEDURES. PAY CLOSE ATTENTION TO FREQUENT CLEANING AND DISINFECTION OF HIGH-TOUCH SURFACES IN PATIENT-CARE AREAS (E.G., BED RAILS, CARTS, BEDSIDE COMMODES, BEDRAILS, DOORKNOBS, OR FAUCET HANDLES). WE USE EPA-REGISTERED HOSPITAL DISINFECTANTS APPROPRIATE FOR THE SURFACE TO BE DISINFECTED.
ENVIRONMENTAL CLEANING AND DISINFECTION LINENS, CLOTHING, AND OTHER ITEMS THAT GO IN THE LAUNDRY DO NOT SHAKE DIRTY LAUNDRY; THIS MINIMIZE THE POSSIBILITY OF DISPERSING VIRUS THROUGH THE AIR. WASH ITEMS AS APPROPRIATE. IF POSSIBLE, LAUNDER ITEMS USING THE WARMEST APPROPRIATE WATER SETTING FOR THE ITEMS AND DRY ITEMS COMPLETELY. DIRTY LAUNDRY THAT HAS BEEN IN CONTACT WITH AN ILL PERSON CAN BE WASHED WITH OTHER PEOPLE S ITEMS. CLEAN AND DISINFECT HAMPERS OR OTHER CARTS FOR TRANSPORTING LAUNDRY.
ENVIRONMENTAL CLEANING AND DISINFECTION ADDITIONAL CONSIDERATIONS: CLEANING STAFF WILL CLEAN NONCRITICAL MEDICAL EQUIPMENT SURFACES WITH A DETERGENT/DISINFECTANT. THIS MAY BE FOLLOWED WITH AN APPLICATION OF AN EPA-REGISTERED HOSPITAL DISINFECTANT, IN ACCORDANCE WITH DISINFECTANT LABEL INSTRUCTIONS. CLEANING STAFF WILL USE BARRIER PROTECTIVE COVERINGS AS APPROPRIATE FOR NONCRITICAL EQUIPMENT SURFACES THAT ARE TOUCHED FREQUENTLY WITH GLOVED HANDS DURING THE DELIVERY OF PATIENT CARE; LIKELY TO BECOME CONTAMINATED WITH BLOOD OR BODY SUBSTANCES; OR DIFFICULT TO CLEAN CLEANING STAFF WILL KEEP HOUSEKEEPING SURFACES (E.G., FLOORS, WALLS, AND TABLETOPS) VISIBLY CLEAN ON A REGULAR BASIS AND CLEAN UP SPILLS PROMPTLY. CLEANING STAFF MAY USE DETERGENT AND WATER AS THEY ARE CONSIDERED ADEQUATE FOR CLEANING SURFACES IN NONPATIENT-CARE AREAS (E.G., ADMINISTRATIVE OFFICES). CLEANING STAFF WILL CLEAN AND DISINFECT HIGH-TOUCH SURFACES (E.G., DOORKNOBS, BED RAILS, LIGHT SWITCHES, AND SURFACES IN AND AROUND TOILETS IN PATIENTS ROOMS) ON A MORE FREQUENT SCHEDULE THAN MINIMAL TOUCH HOUSEKEEPING SURFACES. CLEANING STAFF WILL CLEAN WALLS, BLINDS, AND WINDOW CURTAINS IN PATIENT-CARE AREAS WHEN THEY ARE VISIBLY DUSTY OR SOILED.
PHYSICAL DISTANCING TO STOP THE SPREAD OF CORONAVIRUS, HEALTH AND GOVERNMENT OFFICIALS RECOMMEND AVOIDING LARGE GATHERINGS, LIMITING FACE TO FACE INTERACTIONS, AND MAINTAINING A DISTANCE OF 6 FEET FROM OTHER PEOPLE. THIS REDUCES THE CHANCE OF CONTACT WITH THOSE KNOWINGLY OR UNKNOWINGLY CARRYING THE INFECTION.
HAND HYGIENE WASH YOUR HANDS, WASH YOUR HANDS, WASH YOUR HANDS IF ALCOHOL-BASED HAND RUB (ABHR) IS AVAILABLE, USE IT ROUTINELY FOR HAND HYGIENE IF THERE ARE SHORTAGES OF ABHR, STAFF NEED TO BE PERFORMING HAND HYGIENE USING SOAP AND WATER INSTEAD WASH HANDS WITH SOAP AND WATER WHEN YOUR HANDS ARE VISIBLY SOILED (E.G., BLOOD, BODY FLUIDS) IF AT ANY TIME HAND HYGIENE SUPPLIES (E.G., ABHR, SOAP, PAPER TOWELS) ARE NOT READILY AVAILABLE PLEASE CALL YOUR EXECUTIVE DIRECTOR IMMEDIATELY
HAND HYGIENE WASH YOUR HANDS, WASH YOUR HANDS, WASH YOUR HANDS ALWAYS PERFORM HAND HYGIENE (EVEN IF GLOVES ARE USED) IN THE FOLLOWING SITUATIONS: BEFORE AND AFTER CONTACT WITH THE RESIDENT; AFTER CONTACT WITH BLOOD, BODY FLUIDS, OR VISIBLY CONTAMINATED SURFACES; AFTER REMOVING PERSONAL PROTECTIVE EQUIPMENT (E.G., GLOVES, GOWN, FACEMASK); AND BEFORE PERFORMING A PROCEDURE SUCH AS AN ASEPTIC TASK (E.G., INSERTION OF AN INVASIVE DEVICE SUCH AS A URINARY CATHETER, MANIPULATION OF A CENTRAL VENOUS CATHETER, AND/OR DRESSING CARE WHEN ASSISTING OUR RESIDENTS PLEASE ENSURE THEY PERFORM HAND HYGIENE AFTER TOILETING AND BEFORE MEALS
PERSONAL PROTECTIVE EQUIPMENT (PPE) UTILIZE PPE APPROPRIATELY INCLUDING, BUT NOT LIMITED TO, THE FOLLOWING: GLOVES ARE TO BE WORN IF POTENTIAL CONTACT WITH BLOOD OR BODY FLUID, MUCOUS MEMBRANES, OR NON-INTACT SKIN; GLOVES ARE TO BE REMOVED AFTER CONTACT WITH BLOOD OR BODY FLUIDS, MUCOUS MEMBRANES, OR NON-INTACT SKIN; GLOVES ARE TO BE CHANGED AND HAND HYGIENE IS PERFORMED BEFORE MOVING FROM A CONTAMINATED BODY SITE TO A CLEAN BODY SITE DURING RESIDENT CARE; AND AN ISOLATION GOWN IS TO BE WORN FOR DIRECT RESIDENT CONTACT IF THE RESIDENT HAS UNCONTAINED SECRETIONS OR EXCRETIONS. PPE IS TO BE APPROPRIATELY REMOVED AND DISCARDED AFTER RESIDENT CARE, PRIOR TO LEAVING ROOM (EXCEPT IN THE CASE OF EXTENDED USE OF PPE PER NATIONAL/LOCAL RECOMMENDATIONS), FOLLOWED BY HAND HYGIENE? IF WE ARE EXTENDING THE USE OF PPE ENSURE YOU ARE FOLLOWING FURTHER GUIDANCE PROVIDED BY OUR CLINICAL LEADERSHIP TEAM/ IF IT IS REUSED, ENSURE IT IS CLEANED/DECONTAMINATED/MAINTAINED PRIOR TO USE IF PPE IS NOT AVAILABLE OR ACCESSIBLE AT ANY TIME CALL YOUR EXECUTIVE DIRECTOR IMMEDIATELY THE FACILITY IS WORKING DILIGENTLY TO HAVE SUFFICIENT PPE SUPPLIES AVAILABLE TO FOLLOW INFECTION PREVENTION AND CONTROL GUIDELINES IN THE EVENT OF PPE SHORTAGES, THE FACILITY WILL FOLLOW PROCEDURES OUTLINED BY THE LOCAL HEALTH DEPARTMENT, IDPH, CDC, HFS, AHCA, AND OTHER AVAILABLE HEALTHCARE COALITIONS FOR CONSERVING AND OBTAINING PPE TO ADDRESS THIS ISSUE AS WELL AS ASKING OUR LOCAL GOVERNMENT OFFICIALS FOR ASSISTANCE. ENSURE ALL PPE IS AVAILABLE PRIOR TO STARTING RESIDENT CARE IF NOT READILY AVAILABLE OR ACCESSIBLE OBTAIN PPE SUPPLIES FROM STORAGE AREAS BEFORE PROVIDING CARE. CONTACT EXECUTIVE DIRECTOR FOR REPLACEMENT SUPPLIES IF NOT AVAILABLE IN SUPPLY STORAGE AREA- THE FACILITY HAS SUFFICIENT PPE TO MANAGE
PERSONAL PROTECTIVE EQUIPMENT (PPE) PPE CONSERVATION INFORMATION: FACILITIES ARE IN COMMUNICATION WITH LOCAL HEALTHCARE COALITIONS, FEDERAL, STATE, AND LOCAL PUBLIC HEALTH PARTNERS (E.G., PUBLIC HEALTH EMERGENCY PREPAREDNESS AND RESPONSE STAFF) REGARDING IDENTIFICATION OF ADDITIONAL SUPPLIES. FACILITIES HAVE ALREADY IMPLEMENTED OTHER ENGINEERING AND ADMINISTRATIVE CONTROL MEASURES INCLUDING: REDUCING THE NUMBER OF PATIENTS GOING TO THE HOSPITAL OR OUTPATIENT SETTINGS EXCLUDING HCP NOT ESSENTIAL FOR PATIENT CARE FROM ENTERING THEIR CARE AREA REDUCING FACE-TO-FACE HCP ENCOUNTERS WITH PATIENTS EXCLUDING VISITORS TO PATIENTS WITH CONFIRMED OR SUSPECTED COVID-19 COHORTING PATIENTS AND HCP MAXIMIZING USE OF TELEMEDICINE HCP WITH REQUIRED EDUCATION AND TRAINING, INCLUDING HAVING THEM DEMONSTRATE COMPETENCY WITH DONNING AND DOFFING, WITH ANY PPE ENSEMBLE THAT IS USED TO PERFORM JOB RESPONSIBILITIES, SUCH AS PROVISION OF PATIENT CARE EXTENDED USE OF FACEMASKS IS THE PRACTICE OF WEARING THE SAME FACEMASK FOR REPEATED CLOSE CONTACT ENCOUNTERS WITH SEVERAL DIFFERENT PATIENTS, WITHOUT REMOVING THE FACEMASK BETWEEN PATIENT ENCOUNTERS. THE FACEMASK SHOULD BE REMOVED AND DISCARDED IF SOILED, DAMAGED, OR HARD TO BREATHE THROUGH. HCP MUST TAKE CARE NOT TO TOUCH THEIR FACEMASK. IF THEY TOUCH OR ADJUST THEIR FACEMASK THEY MUST IMMEDIATELY PERFORM HAND HYGIENE. HCP SHOULD LEAVE THE PATIENT CARE AREA IF THEY NEED TO REMOVE THE FACEMASK. RESTRICT FACEMASKS TO USE BY HCP, RATHER THAN PATIENTS FOR SOURCE CONTROL. HAVE PATIENTS WITH SYMPTOMS OF RESPIRATORY INFECTION USE TISSUES OR OTHER BARRIERS TO COVER THEIR MOUTH AND NOSE.
PERSONAL PROTECTIVE EQUIPMENT (PPE) PPE CONSERVATION INFORMATION: (CONTINUED) USE ISOLATION GOWN ALTERNATIVES THAT OFFER EQUIVALENT OR HIGHER PROTECTION. SEVERAL FLUID-RESISTANT AND IMPERMEABLE PROTECTIVE CLOTHING OPTIONS ARE AVAILABLE IN THE MARKETPLACE FOR HCP. THESE INCLUDE ISOLATION GOWNS AND SURGICAL GOWNS. WHEN SELECTING THE MOST APPROPRIATE PROTECTIVE CLOTHING, EMPLOYERS SHOULD CONSIDER ALL OF THE AVAILABLE INFORMATION ON RECOMMENDED PROTECTIVE CLOTHING, INCLUDING THE POTENTIAL LIMITATIONS. NONSTERILE, DISPOSABLE PATIENT ISOLATION GOWNS, WHICH ARE USED FOR ROUTINE PATIENT CARE IN HEALTHCARE SETTINGS, ARE APPROPRIATE FOR USE BY HCP WHEN CARING FOR PATIENTS WITH SUSPECTED OR CONFIRMED COVID-19. IN TIMES OF GOWN SHORTAGES, SURGICAL GOWNS SHOULD BE PRIORITIZED FOR SURGICAL AND OTHER STERILE PROCEDURES. CURRENT U.S. GUIDELINES DO NOT REQUIRE USE OF GOWNS THAT CONFORM TO ANY STANDARDS. SHIFT GOWN USE TOWARDS CLOTH ISOLATION GOWNS. REUSABLE (I.E., WASHABLE) GOWNS ARE TYPICALLY MADE OF POLYESTER OR POLYESTER-COTTON FABRICS. GOWNS MADE OF THESE FABRICS CAN BE SAFELY LAUNDERED ACCORDING TO ROUTINE PROCEDURES AND REUSED. CARE SHOULD BE TAKEN TO ENSURE THAT HCP DO NOT TOUCH OUTER SURFACES OF THE GOWN DURING CARE. LAUNDRY OPERATIONS AND PERSONNEL MAY NEED TO BE AUGMENTED TO FACILITATE ADDITIONAL WASHING LOADS AND CYCLES SYSTEMS ARE ESTABLISHED TO ROUTINELY INSPECT, MAINTAIN (E.G., MEND A SMALL HOLE IN A GOWN, REPLACE MISSING FASTENING TIES), AND REPLACE REUSABLE GOWNS WHEN NEEDED (E.G., WHEN THEY ARE THIN OR RIPPED) CONSIDER THE USE OF COVERALLS. COVERALLS TYPICALLY PROVIDE 360-DEGREE PROTECTION BECAUSE THEY ARE DESIGNED TO COVER THE WHOLE BODY, INCLUDING THE BACK AND LOWER LEGS, AND SOMETIMES THE HEAD AND FEET AS WELL. WHILE THE MATERIAL AND SEAM BARRIER PROPERTIES ARE ESSENTIAL FOR DEFINING THE PROTECTIVE LEVEL, THE COVERAGE PROVIDED BY THE MATERIAL USED IN THE GARMENT DESIGN, AS WELL AS CERTAIN FEATURES INCLUDING CLOSURES, WILL GREATLY AFFECT THE PROTECTIVE LEVEL. HCP UNFAMILIAR WITH THE USE OF COVERALLS MUST BE TRAINED AND PRACTICED IN THEIR USE, PRIOR TO USING DURING PATIENT CARE.
PERSONAL PROTECTIVE EQUIPMENT (PPE) PPE CONSERVATION INFORMATION: (CONTINUED) EXTENDED USE OF ISOLATION GOWNS. CONSIDERATION CAN BE MADE TO EXTEND THE USE OF ISOLATION GOWNS (DISPOSABLE OR CLOTH) SUCH THAT THE SAME GOWN IS WORN BY THE SAME HCP WHEN INTERACTING WITH MORE THAN ONE PATIENT KNOWN TO BE INFECTED WITH THE SAME INFECTIOUS DISEASE WHEN THESE PATIENTS HOUSED IN THE SAME LOCATION (I.E., COVID-19 PATIENTS RESIDING IN AN ISOLATION COHORT). THIS CAN BE CONSIDERED ONLY IF THERE ARE NO ADDITIONAL CO-INFECTIOUS DIAGNOSES TRANSMITTED BY CONTACT (SUCH AS CLOSTRIDIOIDES DIFFICILE) AMONG PATIENTS. IF THE GOWN BECOMES VISIBLY SOILED, IT MUST BE REMOVED AND DISCARDED AS PER USUAL PRACTICESPDF ICON. RE-USE OF CLOTH ISOLATION GOWNS. DISPOSABLE GOWNS ARE NOT TYPICALLY AMENABLE TO BEING DOFFED AND RE-USED BECAUSE THE TIES AND FASTENERS TYPICALLY BREAK DURING DOFFING. CLOTH ISOLATION GOWNS COULD POTENTIALLY BE UNTIED AND RETIED AND COULD BE CONSIDERED FOR RE-USE WITHOUT LAUNDERING IN BETWEEN. IN A SITUATION WHERE THE GOWN IS BEING USED AS PART OF STANDARD PRECAUTIONS TO PROTECT HCP FROM A SPLASH, THE RISK OF RE-USING A NON-VISIBLY SOILED CLOTH ISOLATION GOWN MAY BE LOWER. HOWEVER, FOR CARE OF PATIENTS WITH SUSPECTED OR CONFIRMED COVID-19, HCP RISK FROM RE-USE OF CLOTH ISOLATION GOWNS WITHOUT LAUNDERING AMONG (1) SINGLE HCP CARING FOR MULTIPLE PATIENTS USING ONE GOWN OR (2) AMONG MULTIPLE HCP SHARING ONE GOWN IS UNCLEAR. THE GOAL OF THIS STRATEGY IS TO MINIMIZE EXPOSURES TO HCP AND NOT NECESSARILY PREVENT TRANSMISSION BETWEEN PATIENTS. ANY GOWN THAT BECOMES VISIBLY SOILED DURING PATIENT CARE SHOULD BE DISPOSED OF AND CLEANED. PRIORITIZE GOWNS. GOWNS SHOULD BE PRIORITIZED FOR THE FOLLOWING ACTIVITIES: DURING CARE ACTIVITIES WHERE SPLASHES AND SPRAYS ARE ANTICIPATED, WHICH TYPICALLY INCLUDES AEROSOL GENERATING PROCEDURES DURING THE FOLLOWING HIGH-CONTACT PATIENT CARE ACTIVITIES THAT PROVIDE OPPORTUNITIES FOR TRANSFER OF PATHOGENS TO THE HANDS AND CLOTHING OF HEALTHCARE PROVIDERS, SUCH AS: DRESSING, BATHING/SHOWERING, TRANSFERRING, PROVIDING HYGIENE, CHANGING LINENS, CHANGING BRIEFS OR ASSISTING WITH TOILETING, DEVICE CARE OR USE, WOUND CARE
PERSONAL PROTECTIVE EQUIPMENT (PPE) PPE CONSERVATION INFORMATION: (CONTINUED) EXTENDED USE OF ISOLATION GOWNS. SHIFT EYE PROTECTION SUPPLIES FROM DISPOSABLE TO RE-USABLE DEVICES (I.E., GOGGLES AND REUSABLE FACE SHIELDS). ENSURE APPROPRIATE CLEANING AND DISINFECTION BETWEEN USERS IF GOGGLES OR REUSABLE FACE SHIELDS ARE USED. PRIORITIZE EYE PROTECTION FOR SELECTED ACTIVITIES SUCH AS: DURING CARE ACTIVITIES WHERE SPLASHES AND SPRAYS ARE ANTICIPATED, WHICH TYPICALLY INCLUDES AEROSOL GENERATING PROCEDURES. DURING ACTIVITIES WHERE PROLONGED FACE-TO-FACE OR CLOSE CONTACT WITH A POTENTIALLY INFECTIOUS PATIENT IS UNAVOIDABLE. WHEN COUNTY COVID POSITIVITY RATES ARE GREATER THAN 5% EYE PROTECTION AND FACE MASKS ARE REQUIRED. ADHERE TO RECOMMENDED MANUFACTURER INSTRUCTIONS FOR CLEANING AND DISINFECTION. WHEN MANUFACTURER INSTRUCTIONS FOR CLEANING AND DISINFECTION ARE UNAVAILABLE, SUCH AS FOR SINGLE USE DISPOSABLE FACE SHIELDS, CONSIDER: WHILE WEARING GLOVES, CAREFULLY WIPE THE INSIDE, FOLLOWED BY THEOUTSIDE OF THE FACE SHIELD OR GOGGLES USING A CLEAN CLOTH SATURATED WITH NEUTRAL DETERGENT SOLUTION OR CLEANER WIPE. CAREFULLY WIPE THE OUTSIDE OF THE FACE SHIELD OR GOGGLES USING A WIPE OR CLEAN CLOTH SATURATED WITH EPA-REGISTERED HOSPITAL DISINFECTANT SOLUTION. WIPE THE OUTSIDE OF FACE SHIELD OR GOGGLES WITH CLEAN WATER OR ALCOHOL TO REMOVE RESIDUE. FULLY DRY (AIR DRY OR USE CLEAN ABSORBENT TOWELS). REMOVE GLOVES AND PERFORM HAND HYGIENE.
VISITATION SCREENING AND RESTRICTION OF VISITATION THE VISITORS WILL BE ASKED TO IMMEDIATELY PLACE A MASK ON AND SANITIZE THEIR HANDS ALL VISITORS WILL BE SCREENED PRIOR TO ALLOWING YOU TO PASS THROUGH THE ENTRY CHECKPOINT. VISITORS WILL NOT BE ABLE TO PASS ENTRY CHECKPOINT UNTIL SCREENING IS COMPLETED AND THEY ARE NEGATIVE FOR SYMPTOMS OR FEVER HAVE VISITOR ANSWER ALL QUESTIONS/ SCREEN FOR SYMPTOMS OF RESPIRATORY ILLNESS AND TAKE THE VISITORS TEMPERATURE. IF VISITORS ANSWERS NO TO ALL SCREENING QUESTIONS, THE SCREENER SHOULD ALLOW THE VISITOR TO PROCEED PAST THE CHECKPOINT AREA FOR VISIT. ALL VISITORS MUST WEAR A MASK WITH THE NOSE PINCHED THROUGHOUT THEIR VISIT IF VISITOR ANSWERS YES TO ANY OF THE SCREENING QUESTIONS THE VISITOR SHOULD IMMEDIATELY BE ASKED TO LEAVE THE FACILITY TO SELF-ISOLATE AT HOME AND CONTACT THEIR
RESIDENT CARE AND HEALTH SCREENING THE FACILITY RESTRICTING RESIDENTS (TO THE EXTENT POSSIBLE) TO THEIR ROOMS EXCEPT FOR MEDICALLY NECESSARY PURPOSES. CLINICAL TEAM MEMBERS COMPLETE A TEMPERATURE AND PULSE OXIMETER READING AT LEAST ONCE DAILY ON ALL RESDIENTS. IF THERE IS A CASE IN THE FACILITY, AND RESIDENTS HAVE TO LEAVE THEIR ROOM, THE RESIDENT MUST WEAR FACEMASK, PERFORM HAND HYGIENE, LIMIT THEIR MOVEMENT IN THE FACILITY, AND PERFORM PHYSICAL DISTANCING (EFFORTS ARE MADE TO KEEP THEM AT LEAST 6 FEET AWAY FROM OTHERS). IF PPE SHORTAGE IS AN ISSUE, FACEMASKS SHOULD BE LIMITED TO RESIDENTS DIAGNOSED WITH OR HAVING SIGNS/SYMPTOMS OF RESPIRATORY ILLNESS OR COVID-19. CLOTH FACE MASKS MAY BE USED BY RESIDENTS. THE FACILITY FOLLOWS THE MOST CURRENT GUIDELINES ON GROUP OUTINGS, GROUP ACTIVITIES, AND COMMUNAL DINING AT THIS TIME THE FACILITY HAS IMMEDIATELY ISOLATED RESIDENTS WITH KNOWN OR SUSPECTED COVID-19 IN A PRIVATE ROOM (IF AVAILABLE), OR TAKEN OTHER ACTIONS BASED ON NATIONAL (E.G., CDC), STATE, OR LOCAL PUBLIC HEALTH AUTHORITY RECOMMENDATIONS ANY RESIDENT WHO DEVELOPS SEVERE SYMPTOMS OF ILLNESS AND REQUIRES TRANSFER TO A HOSPITAL FOR A HIGHER LEVEL OF CARE, THE FACILITY MUST ALERT EMERGENCY MEDICAL SERVICES AND THE RECEIVING FACILITY OF THE RESIDENT S DIAGNOSIS (SUSPECTED OR CONFIRMED COVID-19) AND PRECAUTIONS TO BE TAKEN BY TRANSFERRING AND RECEIVING STAFF AS WELL AS PLACE A FACEMASK ON THE RESIDENT DURING TRANSFER (AS SUPPLY ALLOWS) FOR RESIDENTS WHO NEED TO LEAVE THE FACILITY FOR CARE (E.G. DIALYSIS, ETC.), THE FACILITY MUST NOTIFY THE TRANSPORTATION AND RECEIVING HEALTH CARE TEAM OF THE RESIDENT S SUSPECTED OR CONFIRMED COVID-19 STATUS? THE FACILITY HAVE RESIDENTS WHO MUST LEAVE THE FACILITY REGULARLY FOR MEDICALLY NECESSARY PURPOSES (E.G., RESIDENTS RECEIVING HEMODIALYSIS AND CHEMOTHERAPY) WEAR A FACEMASK (IF AVAILABLE) WHENEVER THEY LEAVE THEIR ROOM, INCLUDING FOR PROCEDURES OUTSIDE OF THE FACILITY. UNVACCINATED RESIDENTS THAT LEAVE THE BUILDING WILL BE QUARANTINED IF REQUIRED PER THE CURRENT GUIDANCE
VENTILATION/PHYSICAL BARRIERS PLANT OPERATIONS HAS EVALUATED THE VENTILATION AND PHYSICAL BARRIER NEEDS OF THE FACILITY AND HAS IMPLEMENTED INTERVENTIONS NECESSARY TO COMPLY WITH CURRENT GUIDANCE
VACCINATION THE FACILITY ENCOURAGES AND OFFERS THE COVID VACCINATION THROUGH PHARMACY CLINICS THAT COME TO THE FACILITY AND BY SENDING EMPLOYEES TO AN OFF-SITE VACCINATION PROVIDER
ANTI-RETALIATION PARAGRAPH (O) INCLUDES PROVISIONS TO ENSURE EMPLOYEES ARE AWARE OF THEIR RIGHTS UNDER THE STANDARD, AND THAT THEY ARE PROTECTED FROM RETALIATION FOR EXERCISING THOSE RIGHTS. SPECIFICALLY, THE PARAGRAPH REQUIRES THAT EMPLOYERS INFORM EACH EMPLOYEE OF THEIR RIGHT TO THE PROTECTIONS REQUIRED BY THE STANDARD (SEE PARAGRAPH (O)(1)(I)). EMPLOYERS ARE ALSO REQUIRED TO INFORM EACH EMPLOYEE OF THE PROHIBITION ON EMPLOYERS DISCHARGING OR IN ANY MANNER DISCRIMINATING AGAINST ANY EMPLOYEE FOR EXERCISING THEIR RIGHT TO THE PROTECTIONS REQUIRED BY THE STANDARD, OR FOR ENGAGING IN ACTIONS THAT ARE REQUIRED BY THE STANDARD (SEE PARAGRAPH (O)(1)(II)). IN ADDITION, IT EXPLICITLY PROHIBITS EMPLOYERS FROM DISCHARGING OR IN ANY MANNER DISCRIMINATING AGAINST ANY EMPLOYEE FOR EXERCISING THEIR RIGHT TO THE PROTECTIONS REQUIRED BY THE STANDARD, OR FOR ENGAGING IN ACTIONS THAT ARE REQUIRED BY THE STANDARD (SEE PARAGRAPH (O)(2)).
COVID-19 PANDEMIC RECORD KEEPING ALL RECORDS, SCREENING, EDUCATION, AND POLICIES RELATED THE TO COVID-19 PANDEMIC WILL BE SAFELY STORED FOR 30 YEARS PER THE CURRENT REQUIREMENT.