Outcomes of Intermediate Left Main Disease on Coronary CT Angiography
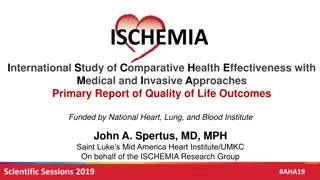
The study evaluates clinical outcomes in patients with intermediate left main disease on coronary CT angiography and assesses the impact of treatment strategies. Excluded participants, study objectives, and population details are discussed within the ISCHEMIA Intermediate LM Substudy. Financial interests and the design of the ISCHEMIA study are also disclosed.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Outcomes with Intermediate Left Main Disease on Coronary CT Angiography ISCHEMIA Intermediate LM Substudy Sripal Bangalore, M.D., John A. Spertus, M.D., Susanna R. Stevens, M.S., Philip G. Jones, M.S., G.B. John Mancini, M.D., Jonathon Leipsic, M.D., Harmony R. Reynolds, M.D., Matthew J. Budoff, M.D., Cameron J. Hague, M.D., JAMES K Min, M.D., William E. Boden, M.D., Sean M. O'Brien, PhD, Robert A. Harrington, M.D., Jeffrey S. Berger, M.D., Roxy Senior, MBBS, MD, DM, Jesus Peteiro, MD, PhD, Neeraj Pandit, M.D., Leonid Bershtein, M.D., Mark A. de Belder, M.D., Hanna Szwed, MD, PhD, Rolf Doerr, M.D., Lorenzo Monti, M.D., Khaled Alfakih, MBBS, MD, Judith S. Hochman, M.D. and David J. Maron, M.D On behalf of the ISCHEMIA Research Group
Disclosure Statement of Financial Interest ISCHEMIA was supported by grants from the NHLBI Devices used in the trial were donated by Abbott Vascular, Medtronic, St. Jude Medical, Volcano, and Omron Healthcare; medications were provided by Amgen, Arbor Pharmaceuticals, AstraZeneca Pharmaceuticals, and Merck Sharp & Dohme.
Extension of Survival in Left Main Disease with Revascularization CABG vs. No CABG trials-1980s Overall Vessel disease 1-2 VD 3 VD Left main N=150 LV function Normal Abnormal Exercise test Normal Abnormal Angina Class O, I, II Class III, IV -4 -2 0 2 4 6 8 10 12 14 16 18 20 Extension of survival (months) Yusuf et al. Lancet 1994;344:563-570.
Left Main Disease Severity and Outcomes with CABG VA Cooperative Trial Pinteraction=0.47 CABG Med P=0.089 P=0.036 100 92 Survival at 42 months (%) 90 83 82 80 70 60 48 50 40 30 20 10 0 >75% 50-75% Left Main Stenosis Severity Takaro et al. Circulation. 1982;66:14 22.
ISCHEMIA Study Design ISCHEMIA excluded patients with left main disease Maron DJ, et al. American Heart Journal. 2018; 201;124-135.
ISCHEMIA Intermediate LM Substudy Study Objectives Evaluate clinical and QoL outcomes in patients with and without intermediate LM disease (25-49%) on coronary CT angiography Evaluate the impact of treatment strategy on clinical and QoL outcomes across the subgroups
ISCHEMIA Intermediate LM Substudy Study Population 515179 randomized participants Excluded: Prior CABG (N=202) No prior CABG (N=4977) Excluded: No CCTA (N=1152) No CAD on CT (N=17) LM stenosis missing (N=4), not present (N=35), or non- evaluable (N=59) Final Cohort (N=3699) LM <25% on CCTA (N=2737) LM 25-49% on CCTA (N=962)
ISCHEMIA Intermediate LM Substudy Study Endpoints Primary Endpoint Time to CV Death, MI, Hospitalization for Unstable Angina, Heart Failure or Resuscitated Cardiac Arrest Secondary Endpoints Time to CV death or MI Angina related Quality of Life Individual components of the primary endpoint
ISCHEMIA Intermediate LM Substudy Baseline Characteristics <25% LM stenosis CON (N=1,358) <25% LM stenosis INV (N=1,379) Intermediate LM CON (N=495) Intermediate LM INV (N=467) Demographics Age (Q1, Q3) 63 (56, 70) 63 (57, 70) 65 (58, 71) 66 (60, 71) Female sex 20.3% 22.6% 19.8% 19.7% Clinical history Hypertension 68.1% 68.9% 73.4% 72.2% Diabetes 39.8% 39.8% 45.5% 42.4% Prior MI 16.7% 17.2% 15.2% 15.0%
ISCHEMIA Intermediate LM Substudy Stress Test Characteristics <25% LM stenosis CON (N=1,358) <25% LM stenosis INV (N=1,379) Intermediate LM CON (N=495) Intermediate LM INV (N=467) Stress imaging overall Severe 72.8% 72.4% 72.1% 70.2% 48.5% 44.3% 45.5% 53.0% 38.7% 41.9% 44.9% Moderate 38.4% 7.7% 8.8% 5.9% Mild 4.6% Exercise tolerance test Severe 27.2% 27.6% 27.9% 29.8% 83.4% 85.8% 85.5% 85.4% 7.6% 8.2% 6.5% Moderate 8.0%
ISCHEMIA Intermediate LM Substudy CCTA Characteristics <25% LM stenosis CON (N=1,358) <25% LM stenosis INV (N=1,379) Intermediate LM CON (N=495) Intermediate LM INV (N=467) Number of diseased vessels ( 50% stenosis) 1 26.9% 28.3% 13.0% 15.3% 2 37.6% 31.5% 24.7% 24.3% 3 35.6% 40.3% 62.3% 60.5% LAD 86.6% 85.7% 92.6% 93.3% Proximal LAD disease RCA 39.6% 39.3% 65.5% 63.3% 66.2% 68.6% 80.0% 79.9% LCX 69.9% 71.4% 83.9% 81.1%
ISCHEMIA Intermediate LM Substudy Invasive Angiographic Characteristics <25% LM stenosis INV (N=1,379) 1.4% Intermediate LM INV (N=467) 7.0% Left main disease* Proximal LAD disease* 33.2% 42.7% 0 vd* 6.1% 3.2% 1 vd* 26.6% 17.2% 2 vd* 31.9% 32.8% 3 vd* 35.4% 46.8% SYNTAX score (Q1, Q3) 15 (8, 23) 21 (12, 29) PCI 61.5% 49.7% DES during first PCI 98.0% 97.1% CABG 18.2% 32.1% IMA to LAD 83.3% 84.6% * Based on stenosis of 50% or greater on QCA
ISCHEMIA Intermediate LM Substudy Aggregate Outcome based on LM severity Primary Endpoint CV Death or MI
ISCHEMIA Intermediate LM Substudy Aggregate Outcomes based on LM severity (25-49% vs. <25% stenosis) HRadj (95% CI) P-value Primary endpoint 1.31 (1.06, 1.61) 0.0123 1.24 (0.99, 1.55) 0.0574 CV death/MI CV death/MI/Stroke 1.30 (1.05, 1.60) 0.0143 CV Death 1.63 (1.11, 2.39) 0.0122 1.22 (0.94, 1.56) 0.1293 Primary MI 1.20 (0.88, 1.62) 0.2498 Non Procedural primary MI Procedural primary MI 1.64 (1.00, 2.67) 0.0487 0.76 (0.08, 6.91) 0.8088 RCA 1.89 (0.88, 4.05) 0.1020 Unstable Angina Heart Failure 2.06 (1.10, 3.84) 0.0239 Stroke 1.82 (1.04, 3.20) 0.0362
ISCHEMIA Intermediate LM Substudy Outcomes by Treatment Group
ISCHEMIA Intermediate LM Substudy Baseline Quality of Life <25% LM stenosis CON (N=1,201) <25% LM stenosis INV (N=1,204) Intermediate LM CON (N=425) Intermediate LM INV (N=400) SAQ-7 Summary Score 75.1 18.1 73.7 19.1 75.2 20.1 76.4 17.4 SAQ-7 Angina Frequency Score 82.1 18.6 80.9 19.7 81.9 21.3 82.7 19.7 SAQ-7 QoL Score 75.1 18.1 73.7 19.1 75.2 20.1 76.4 17.4 SAQ-7 Physical Limitation Score 81.3 22.7 78.9 23.6 80.2 23.7 82.8 21.1 Rose Dyspnea Scale 1.2 1.3 1.2 1.3 1.2 1.3 1.1 1.3 EQ-5D Visual Analog scale 70.2 16.1 69.1 17.0 70.2 16.2 70.2 16.0
ISCHEMIA Intermediate LM Substudy Quality of Life- Treatment Effect SAQ-7 Summary Score SAQ-7 Angina Frequency Score 100 100 90 90 Score Score Treatment strategy Treatment strategy 80 80 Conservative Invasive Conservative Invasive LM stenosis <25% 25-49% LM stenosis <25% 25-49% 70 70 0 3 6 12 18 24 30 36 42 48 0 3 6 12 18 24 30 36 42 48 Month Month
ISCHEMIA Intermediate LM Substudy SAQ Angina Frequency Score-Heterogeneity of Treatment Effect 3- months Daily/weekly angina p = 0.67 <25% stenosis 2.79 (2.00, 3.89) 25-49% stenosis 2.41 (1.32, 4.38) 12- months Monthly angina p = 0.34 <25% stenosis 2.45 (1.92, 3.13) Daily/weekly angina p = 0.80 25-49% stenosis 3.12 (2.02, 4.83) <25% stenosis 2.16 (1.54, 3.05) 1.97 (1.04, 3.72) 36-months 25-49% stenosis No angina p = 0.90 <25% stenosis 1.09 (0.76, 1.57) Daily/weekly angina Monthly angina p = 0.85 p = 0.63 25-49% stenosis 1.04 (0.59, 1.85) <25% stenosis <25% stenosis 1.94 (1.51, 2.50) 1.82 (1.18, 2.81) 0.5 25-49% stenosis 2.04 (1.32, 3.16) 0.25 1 2 4 25-49% stenosis 1.47 (0.68, 3.15) Odds Ratio No angina p = 0.73 Monthly angina p = 0.96 <25% stenosis 1.14 (0.79, 1.64) <25% stenosis 1.41 (1.05, 1.90) 25-49% stenosis 1.28 (0.70, 2.33) 25-49% stenosis 1.39 (0.82, 2.34) 0.25 0.5 1 2 4 No angina p = 0.008 <25% stenosis 1.92 (1.17, 3.14) Odds Ratio 25-49% stenosis 0.57 (0.27, 1.22) 0.25 0.5 1 2 4 Odds Ratio
Summary ISCHEMIA excluded patients with severe left main disease by design Patients with intermediate left main disease in ISCHEMIA: had greater extent of CAD indicating greater atherosclerotic burden had worse prognosis with higher risk of cardiovascular events But similar quality of life including angina-specific quality of life
Conclusions There was no evidence of meaningful heterogeneity of treatment effect across left main severity No difference in INV vs. CON for primary or major secondary clinical outcomes Increase in procedural MI but decrease in non procedural MI with INV Significant and durable benefit of INV at improving angina related QoL in symptomatic patients