Overview of Hydatid Liver Disease
Hydatid liver disease is caused by the larva of Echinococcus granulosus, common in Mediterranean countries. The disease involves three layers: adventitia, ectocyst, and endocyst, with hydatid fluid characterized by its crystal-clear appearance. Clinical features range from being symptomless to complications like suppuration and ruptured cysts. Diagnosed through imaging and serological tests, treatment options include surgical excision and scolicidal agents. Complications of surgical treatment should be carefully managed to avoid adverse outcomes. Liver tumors, including benign and malignant types, also present diagnostic challenges and treatment considerations.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
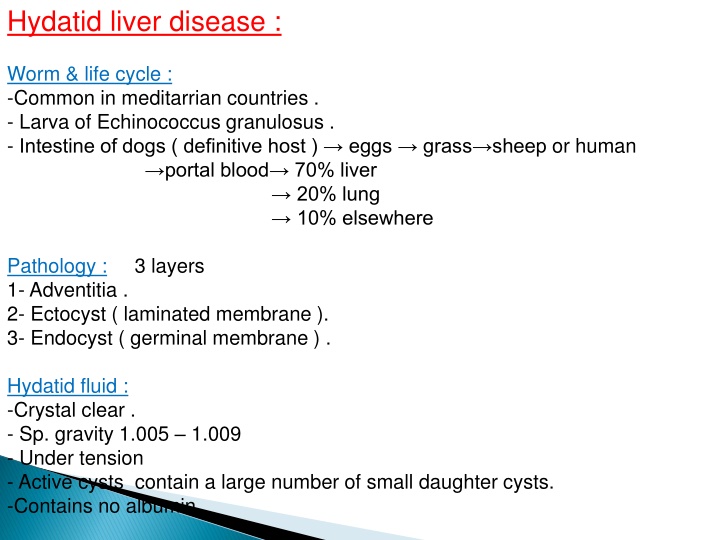
Hydatid liver disease : Worm & life cycle : -Common in meditarrian countries . - Larva of Echinococcus granulosus . - Intestine of dogs ( definitive host ) eggs grass sheep or human portal blood 70% liver 20% lung 10% elsewhere Pathology : 3 layers 1- Adventitia . 2- Ectocyst ( laminated membrane ). 3- Endocyst ( germinal membrane ) . Hydatid fluid : -Crystal clear . - Sp. gravity 1.005 1.009 - Under tension - Active cysts contain a large number of small daughter cysts. -Contains no albumin
Clinical features : 1- symptomless 2- Abdominal mass . 3- Pressure manifestation ; - Discomfort - Fullness & dyspepsia. - Jaundice 4- Complications ; - Suppuration - Ruptured .. daughter hydatids intrabiliary jaundice acute cholangitis Peritoneal present as an acute abdomen after minor abdominal trauma. pleural cavity Course of the disease : 1) Dead - calcified cyst . 2) Enlarged gradually become manifested by its size and may float in the peritoneal cavity DDx mesenteric, pancreatic or renal cyst. 3) Complication e.g. Rupture , infection .
Dx : 1) US .multiloculated cyst 2) CT. scan & MRI . floating membrane within the cysts 3) Serological & immunological tests : a) Antibodies to hytadid antigen by ELISA . b) Casoni s test 75% +ve . c) Compliment fixation test . Rx : - Surgical Rx ; 1) open surgical Rx A. Excision of the cysts B.Deroofing with evacuation of contents . C. less likely liver resection. 2)Laparoscopic surgery might be beneficial Scolicidal agents : 1- Ethanol alcohol 95% . 2- Hypertonic saline 3- Silver nitrate 0.5% . 3- povidone iodine . Medical Rx ; 1) mebendazol 40 50 mg/kg. 2) Albendazol 10 15 mg/kg. 3) praziquantel 40 mg/kg
Complication of surgical treatment of hydatid cysts : 1) Biliary leak fistula 2) Supuration subhepatic , subphrenic or intrahepatic abscess 3) Liver tissue damage and bleeding 4) Recurrence 5) Missed small deep cyst 6) Injuries of adjacent organs 7) Cholangitis 8) Anaphylactic shock 9) Contamination of peritoneal cavity. (careful, Albendazole& praziquantel) 10) Wound infection
Liver tumours :. I - Benign tumour. II - Malignant tumour. I - Benign : A Haemangioma : (vascular lesion) - Most common . - Often multiple of cavernous type . - symptom less . - If too large mass compressible . -They have little if any malignant potential. Dx: -U/S diagnostic abnormal plexus of vessels. -CT peripheral nodular enhancement on arterial phase then centripetal enhancement so it is delayed or slow contrast enhancement due to small vessel uptake. - P/c biopsy should be avoided may bleed profusely Rx : - If small & asymptomatic No Rx - If large and symptomatic Rx is controversial (Embolisation , Lobe or segmental ressection or DXT to size) . Indication of Rx : 1) Arterio venous shunting embarrass heart function . 2) Misdiagnosis of malignant vascular tumour .
B B Hepatic adenoma : -premalignant -Women with contraceptive pills . -Develops in otherwise normal liver tissue. Hepatic adenoma : Dx: -U/S &CT well circumscribed solid tumours. But, unfortunately difficult to differentiate from malignant tumours radiologically. So -Angiography well developed peripheral arterialisation of the tumours Rx Rx . . Lobe or segmental resection is Rx of choice. (premalignant) C C Focal nodular hyperplasia (FNH): Focal nodular hyperplasia (FNH): -Focal overgrowth of functioning liver tissue supported by fibrous tissue stroma (hepatocytes & kupffer cells) - Middle age female with no association with underlying liver disease -Unusual & Unknown aetilogy . Dx - -U/S solid tumour, CT central scarring & well-vascularised lesion (not specific) -Sulphur colloid liver scan FNH +ve (kupffer cells) but adenoma & primary or metastatic tumours -ve ( kupffer cells ) Dx
II Malignant liver tumours : Primary cancer : 1- Hepatocellular carcinoma ( HCC ) : - one of the commonest tumour in the world specially UK - Association with chronic liver disease HBV & HCV screening by U/S and AFP. -Middle age 3rd 4th decades Male: female 8:1. - 80% of primary liver malignancy and 80% of HCC occur in cirrhotic liver. - May be multicentric . - Fetoprotein . Clinical features : -S&S of CLD: malaise and weakness , jaundice , ascites , portal hypertension. - S&S of Cancer : Mass ; wt. , anorexia ,,. Dx : CT. , US. , biopsy . Rx: 1. surgical resection (lobe or segment/s) 2. Liver transplantation (size, site and availability of donors)
2 2- - Cholangiocarcinoma : - Elderly age. Patients with PSC - Fibrotic tumors stricture often fibrous at the confluence of R&L hepatic ducts jaundice. - Distal b.d. CC polypiod obstruct the lumen of b.d. Clinical features : -Painless obstructive jaundice -Enlarged tender liver , wt. , fever , asthenia Dx -U/S dilated intrahepatic but not extra-hepatic b.d. -Cholangiography hilar stricture Brush cytology tissue dx (2/3). -CT ? Mass ( if infiltration liver parenchyma) - Angioraphy (local spread to PV or HA). Cholangiocarcinoma :
Rx Surgical resection + Chemo and radiotherapy Prognosis Very poor
Secondary liver Much more common -Multiple usually Sources : Intra abdominal : ovaries Extra abdominal: Breast & Sarcoma . Dx: 1. Dx of liver tumours as described before (U/S, CT .etc) 2. Dx the primary- clinical exam, chest CT, bone scan, colonoscopy . etc. Rx: 1.Surgical resection 2. If not resectable systemic chemo (5 FU & folinic acid) Px: The 5-year survival rate after resection of solitary colorectal metas. is 35% Secondary liver tumours tumours (Hepatic Deposits): (Hepatic Deposits): Intra abdominal : - GIT (colorectal), -Pancreas -Uterus & Extra abdominal: - Melanoma, Carcinoid tumours,
2 2- - Cholangiocarcinoma : - Elderly age. Patients with PSC - Fibrotic tumors stricture often fibrous at the confluence of R&L hepatic ducts jaundice. - Distal b.d. CC polypiod obstruct the lumen of b.d. Clinical features : -Painless obstructive jaundice -Enlarged tender liver , wt. , fever , asthenia Dx -U/S dilated intrahepatic but not extra-hepatic b.d. -Cholangiography hilar stricture Brush cytology tissue dx (2/3). -CT ? Mass ( if infiltration liver parenchyma) - Angioraphy (local spread to PV or HA). Cholangiocarcinoma :