Overview of Upper Gastrointestinal Infections: Causes and Clinical Presentation
Explore viral infections of the upper GI tract, focusing on Cytomegalovirus (CMV), a common opportunistic pathogen. Learn about symptoms, diagnostic approaches, and endoscopic findings associated with CMV infection in the upper GI tract.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Upper gastrointestinal infections Omar Ahmed , MSc, M.D, Ph.D.
Outlines 1-Introduction 2-What are the components of upper GI tract? 3-GI tract may be the primary site of infection or affected secondarily in multisystemic or disseminated infections. 4-Upper GI infections are classified according to etiology into 4 categories; -Viral -Bacterial -Parasitic -Fungal
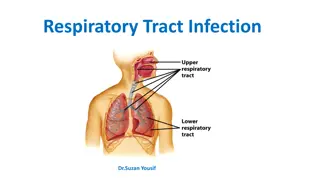
Introduction The upper gastrointestinal (GI) tract, including the esophagus, stomach and small intestine, is subject to a vast array of pathogens. While some may be a reflection of disseminated infection, others produce disease specific to the upper GI tract. This review focuses on the most common infectious disorders of the upper GI tract that may be encountered by gastroenterologists and general practioners.
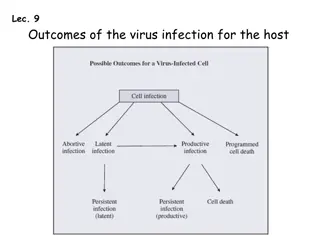
A) Viral infections of the upper gastrointestinal tract The type of viral infection and the manifestations of disease vary with the site of infection and the immune status of the patient. This include: 1-Cytomegalovirus 2-Herpesvirus 3-HIV
1) Cytomegalovirus Cytomegalovirus (CMV) may be seen throughout the upper GI tract. CMV most commonly presents as an opportunistic pathogen in patients with a suppressed immune system such as persons with acquired immune deficiency syndrome (AIDS) or those with history of solid organ or bone marrow transplantation. Primary infections in healthy persons are generally self-limited. Symptoms vary with the immune status of the patient and the site of infection.
C/P: The most common clinical symptoms are diarrhea, abdominal pain, fever and weight loss.1 A rare but important entity associated with CMV infection is hypertrophic gastropathy and protein-losing enteropathy. Investigations: 1- C.B.C: Atypical lymphocytosis may be detected 2-Serological diagnosis depends on the detection of CMV-specific IgM antibody plus a fourfold rise or seroconversion of IgG 3- PCR
4-Diagnostic upper endoscopy: Patients with CMV infection have endoscopic abnormalities that include ulcers (most common),1 erythema, hemorrhage, and inflammatory masses that may be segmental and patchy. The ulcers may be single or multiple, superficial or deep. 5-Biobsy: The characteristic inclusions may be seen on routine H&E preparations and can be either intracytoplasmic or intranuclear. Nuclear inclusions are consist of a basophilic inclusion surrounded by a clear halo, imparting the classic owl s eye appearance
Treatment: Only symptomatic treatment is required in the immunocompetent patient. Immunocompromised individuals: ganciclovir 5 mg/kg IV twice daily or with oral valganciclovir 900 mg twice daily for at least 14 days. Foscarnet or cidofovir is also used in CMV treatment of immunocompromised patients who are resistant to or intolerant of ganciclovir-based therapy.They can be given intravitreally if required
1) Herpes simplex virus Like CMV, Herpes simplex virus (HSV) infection may be seen throughout the GI tract and occur in both immunocompromised and immunocompetent patients. Within the upper GI tract, the most common site of infection is the oesophagus. Patients with herpetic oesophagitis may present with dysphagia, odynophagia, chest pain, nausea, vomiting, fever and bleeding. Particularly in immunocompromised persons, herpetic oesophagitis may be accompanied by life-threatening disseminated infection at the time of diagnosis. In immunocompetent patients, herpetic infection is often self-limited
Investigations: 1-Diagnosis is often made clinically. However in suspected cases demonstration of virus in vesicular fluid, usually by direct immunofluorescence or PCR may be done. 2-Upper Endoscopy: Ulcers are the most common endoscopic finding, usually associated with exudate.
Treatment: Oral lesions in an immunocompetent individual may be treated with topical aciclovir. All severe manifestations should be treated, regardless of the time of presentation by Aciclovir 5 mg/kg 3 times daily IV for 7 10 days or Oral aciclovir 400 mg 4 times daily for 7 10 days.
3) HIV Chronic idiopathic oesophageal ulcers have been described in association with human immunodeficiency virus (HIV). The HIV p24 core protein has been detected in ulcerated mucosa, suggesting that HIV is capable of producing ulcers in the absence of other pathogens, although the causative ability of the virus remains controversial. The diagnosis of idiopathic HIV-associated oesophageal ulcer should only be made when other pathogens have been excluded. More recently, these similar lesions have also been described in patients who have undergone bone marrow and solid organ transplants as well.
Histological abnormalities of the bowel mucosa have been noted in HIV-positive patients both with and without diarrhoea. The histologic features may mimic celiac disease, including villous blunting, crypt hypertrophy, increased intraepithelial lymphocytes and lamina propria expansion by mononuclear cells
B) Bacterial infections of the upper gastrointestinal tract 1-Bacterial food poisoning: (a)Staph. Aureus: It is transmitted via the hands of food handlers to foodstuffs such as dairy products, including cheese, and cooked meats. Nausea and profuse vomiting develop within 1 6 hours. Diarrhoea may not be marked. Most cases settle rapidly but severe dehydration can occasionally be life-threatening. Antiemetics and appropriate fluid replacement are the mainstays of treatment.
(b) Bacillus cereus: Ingestion of the pre-formed heat-stable exotoxins of B. cereus causes rapid onset of vomiting and some diarrhoea within hours of food consumption, which resolves within 24 hours. Fried rice and freshly made sauces are frequent sources; If viable bacteria are ingested and toxin formation takes place within the gut lumen, then the incubation period is longer (12 24hours) and watery diarrhoea and cramps are the predominant symptoms. The disease is self-limiting but can be quite severe. Rapid and judicious fluid replacement is required.
(c) Clostridium Perfringens: If contaminated meat products are incompletely cooked and stored in anaerobic conditions, C. perfringens spores germinate and viable organisms multiply. Subsequent reheating of the food causes release of enterotoxin. Symptoms (diarrhea and cramps) occur some 6 12 hours following ingestion. The illness is usually self-limiting. Clostridial necrotising enteritis (CNE) or pigbel is an often-fatal type of food poisoning caused by a -toxin of C. perfringens, type C.
(d) Salmonella enterica: Salmonella enterica serovars other than Salmonella Typhi and Paratyphi can cause gastroenteritis. kingdom. Two serovars are most important worldwide: Salmonella Enteritidis and Salmonella Typhimurium. Transmission is by contaminated water or food, particularly poultry, egg products and minced beef, direct person-to-person spread or the handling of exotic pets such as salamanders, lizards or turtles. The incubation period of Salmonella gastroenteritis is 12 72 hours and the predominant feature is diarrhoea, sometimes with passage of blood. Antibiotics are not indicated for uncomplicated Salmonella gastroenteritis but are prescribed for bacteraemia.
(e) Yersinia enterocolitica: Yersinia enterocolitica, commonly found in pork, causes mild to moderate gastroenteritis and can produce significant mesenteric adenitis after an incubation period of 3 7 days. It predominantly causes disease in children but adults may also be affected. The illness resolves slowly
2-Mycobacterial tuberculosis: Tuberculosis can affect multiple organs of the upper GI tract with symptomology associated site of involvement. Clinical features of GI tuberculosis are non-specific but include weight loss, fever, abdominal pain and diarrhea. Most reported cases of esophageal M. tuberculosis, which may present with dysphagia, occur as part of disseminated disease in patients with pulmonary T.B infection.
In primary GI tuberculosis, the ileum is the most commonly involved site, with the duodenum and gastro-oesophageal much less frequently involved. Strictures and ulcers, often occurring in tandem, are the most common endoscopic findings, in addition to thickened mucosal folds and inflammatory nodules. The ulcers are often circumferential and transverse. Multiple and segmental lesions with skip areas are common in the small bowel, mimicking Crohn s disease. Large inflammatory masses, usually involving the ileocaecum, may be seen. The characteristic histological lesion of tuberculosis is caseating granulomas that are often confluent and may be present at any level of the gut wall.
3-Mycobacterium avium-intracellulare complex (MAI): MAI is the most common mycobacterium isolated from the GI tract and it is most frequently found in the small bowel.Atypical mycobacterial infection has only been rarely reported in the oesophagus or stomach.Symptoms include diarrhoea, abdominal pain, fever and weight loss, and often reflect systemic infection. Endoscopy is usually normal, although white nodules, small ulcers or haemorrhages may be present. The bacilli stain with acid-fast stains, as well as PAS and GMS stains. Culture and PCR assays may also be helpful.
4-Whipple disease (Tropheryma whippelii): The small bowel is the most commonly affected site in Whipple disease. Clinically, infection presents in middle-aged white males with chronic weight loss, arthritis, malabsorption and lymphadenopathy. Many patients also have significant neuropsychiatric manifestations. Endoscopically, mucosal folds are thickened and coated with yellow-white plaques, often with surrounding erythema and friability.
-Biopsy from duodenum shows foamy cells which are stained positive with PAS stain. -PCR is also diagnostic Treatment: Meropenam/ceftriaxone IV for 14 days followed by Trimetoprim/ sulphamethoxasole for 12 months
5-Helicobacter Pylori: H. pylori is a curved, Gram negative rod that produces urease. Evidence suggests that H. pylori is transmitted by fecal oral route and oral-oral route. H. pylori colonizes the antrum, body, and fundus of the stomach and causes active chronic gastritis, which is characterized by histological increases in mucosal neutrophils and round cells. H. pylori infection affects 90% of patients with duodenal ulcers and 70 90% of those with gastric ulcers. H. pylori is a predisposing factor for developing gastric adenocarcinoma and gastric lymphoma of mucosa associated lymphoid tissue (MALT) and is a WHO recognized carcinogen.
C/P: 1-Asymptomatic: as many as 85 percent of affected individuals will never experience symptoms of any sort. 2-Non specific manifestations: as epigastric pain especially in the morning and in between meals, nausea, vomiting, belching and anorexia. 3-Manifestations of complications; -Peptic ulcer disease manifested by severe epigastric pain, hematemesis or melena -Gastric adenocarcinoma and MALToma
Investigations: H. pylori can usually be diagnosed with one of three minimally invasive tests: 1-Blood antibody tests can detect whether specific defensive proteins, known as antibodies, have been produced by the immune system in response to the bacteria. 2-Stool antigen tests look for direct evidence of the infection in a stool sample by detecting a specific protein, known as an antigen, on the surface of the bacteria. 3-Carbon urea breath tests are performed by breathing into a prepared packet 10 to 30 minutes after swallowing a tablet containing urea (a chemical comprised of nitrogen and a minimally radioactive carbon). H. pylori produces an enzyme that breaks down urea into ammonia and carbon dioxide (CO2). Excessive levels of CO2 will trigger a positive reaction, confirming the presence of the bacteria.
4-Invasive tests Biopsy specimens obtained by endoscopy are examined using traditional stains such as Giemsa, Warthin Starry silver, or hematoxylin eosin stains. Newer molecular tests are available to diagnose H. pylori. Biopsy tests may give false negative results in patients who are bleeding acutely, on proton pump inhibitors (PPIs), or who have recently taken antibiotics.
Treatment: Typically speaking, H. pylori is not treated if it does not cause symptoms. If an H. pylori infection causes symptomatic disease, the treatment would be focused on the eradication of the infection by the following regimens: First-line therapy involves a 14-day course of the antibiotics clarithromycin and amoxicillin used in combination with an oral proton pump inhibitor(PPI). Second-line therapy would involve a 14-day course of the antibiotics tetracycline and metronidazole, an oral PPI, and bismuth subsalicylate tablets Sequential therapy involves two separate courses of therapy. The first is conducted over five days with amoxicillin and an oral PPI. This is followed by a second five-day course comprised of clarithromycin, amoxicillin, and an oral PPI.
C) Parasitic infections of the upper gastrointestinal tract (1) Protozoan infections 1-Giardia lamblia: -Infection with Giardia lamblia is found worldwide and is common in the tropics. It particularly affects children, tourists and immunosuppressed individuals and infection usually occurs by ingesting contaminated water. -Incubation period of 1 3 weeks -C/P: Diarrhea, abdominal pain, weakness, anorexia, nausea and vomiting. On examination, there may be abdominal distension and tenderness. Chronic diarrhoea and malabsorption may occur, with bulky stools.
Investigations: Stool analysis: it should be obtained at 2 3-day intervals for detection of cysts. Stool antigen test. Duodenal or jejunal aspiration by endoscopy gives a higher diagnostic yield. The string test may be used for detection of trophozoites. Treatment: a single dose of tinidazole 2 g, or metronidazole 400 mg 3 times daily for 10 days, or nitazoxanide 500 mg orally twice daily for 3 days
2-Cryptosporidium parvum and hominis: Cryptosporidium spp. are coccidian protozoal parasites of humans and domestic animals. Infection is acquired by the faecal oral route through contaminated water supplies. The incubation period is approximately 7 10 days and is followed by watery diarrhoea and abdominal cramps. The illness is usually self-limiting but in immunocompromised patients, especially those with HIV, the illness can be devastating, with persistent severe diarrhoea and substantial weight loss
Investigations: Stool examination: it should be stained using acid fast stain for detection of oocysts. Stool antigen test. ELIZA for antigen detection PCR Duodenal biopsy by endoscopy can detect oocyte Treatment: -Immunocompetent patient: Nitazoxanide and symptomatic treatment -Immunocompromised patient: A combination of paromomycin and azithromycin may be partially effective, and enhancing the immune status is the most crucial part.
3-Cyclospora cayetanensis: Cyclospora cayetanensis is a globally distributed coccidian protozoal parasite of humans. Infection is acquired by ingestion of contaminated water and recent food-borne outbreaks have been associated with raspberries and coriander (cilantro). The incubation period of approximately 2 11 days is followed by diarrhoea with abdominal cramps, which may remit and relapse. Although usually self-limiting, the illness may last as long as 6 weeks, with significant weight loss and malabsorption, and is more severe in immunocompromised individuals.
Investigation: Detection of oocysts on faecal microscopy or PCR of stool. Treatment : co-trimoxazole 960 mg twice daily for 7 days.
4-Cystoisospora belli: It is a coccidian protozoal parasite of humans that infects epithelial cells of small intestine. Transmission: Infection occurs by ingestion of sporocysts-containing oocysts. C/P: acute, nonbloody diarrhea with crampy abdominal pain, which can last for weeks and result in malabsorption and weight loss. In immunocompromised patients, and in infants and children, the diarrhea can be severe. Eosinophilia may be present (differently from other protozoan infections)
Investigation: Detection of immature oocysts on faecal microscopy or PCR of stool. Doudenal or jejunal biopsy by endoscopy Treatment : Co-trimoxazole is treatment of choice
(2) Intestinal trematodes: -Fasiolopsis Buski; Pathogenesis 1- Infective stage encysted metacercaria attached to edible water plants, such as the water caltrop and chestnuct 2- Definitive host man and pig 3- I.H. 2 ndplanorbis snail 4- Habitat small intestine esp. duodenum 5- Mode of infection ingestion of edible water plants contaminated by encysted metacercaria
Clinical features 1- Asymptomatic in most infections 2- Most severe in children 3- Epigastric pain, vomiting and diarrhea , initially alternating with constipation but later becoming persistent 4- In severe infection (1000-2000 flukes) diarrhea may be severe with intestinal hemorrhage and perforated intoxication [cause of death] 5- In severe cases malabsorption , wasting, edema of the face and lower limbs and ascites Investigations 1- Detection of characteristic eggs in faeces (smear&conc.) 2- Sometimes, adult flukes can be detected in faeces or vomitus Treatment praziquantel
(2) Intestinal cestodes: A-Taenia saginata Pathogenesis 1- Infective stage cysticercus bovis in beef 2- Definitive host man 3- Habitat small intestine 4- I.H. cattle 5- Mode of infection - Ingestion of cysticercus bovis in raw or improperly cooked beef (steaks, hamburgers, kabab) adult in 3 months
Clinical features 1- Digestive disturbances (intestinal irritation) - Nausea, vomiting, diarrhea, colic and anorexia and weight loss 2- Neurological manifestations: headache, insomnia or convulsions caused by 4- Mechanical obstruction : by a rolled mass of worms 5- Appendicitis or cholangitis : caused by stray segments of the worms 6- Perianal irritation and itching and worry of the patient: due to migration of the segments out of the anus
Investigations: 1- Detection of eggs - Faecal smear or - Anal swabs 2-Detection of gravid segments in stool Treatment: 1- Praziquantel (The drug of choice) - Single oral dose of 10 m g/kg body weight 2- Niclosamide (Yomesan) - Single oral dose of 2 gm (4 tab.) for adults and 1 gm for children 3-Quinacrine HCL (Atebrine)
B-Taenia solium Pathogenesis 1- Infective stage cysticercus cellulosae in pork 2- Definitive host man 3- Habitat small intestine 4- I.H. pig (muscles of the tongue, shoulder, neck and diaphragm) 5- Mode of infection - Ingestion of cysticercus cellulosae in undercooked pork ( adult) Clinical features 1- Similar to T.saginata (but no perianal itching) + 2- Cysticercosis - When man ingests eggs of T.solium the larval stage (cysticercus cellulosae) develops in the extraintestinal tissues leading to a condition known as cysticercosis
Diagnosis similar to T.saginata Treatment [doses similar to D.latum but] 1- Praziquantel and niclosamide - Should be avoided 2- Quinacrine HCL (Atebrine) - It is preferable because it leads to expulsion of the intact worms
C-Diphyllobothrium latum Pathogenesis 1- Infective stage plerocercoid larva in fish muscles 2- Definitive host man dogs and cats fish eating animals 3- Habitat small intestine 4- I.H. - 1 st Cyclops (procercoid larva) - 2 nd fresh water fishes 5- Mode of infection - Ingestion of plerocercoid larva in raw or improperly cooked or unsalted fresh water fishes (adult in 6 weeks)
Clinical features are similar to T.saginata in addition to Pernicious anemia (Macrocytic hyperchromic): - As the parasite competes with the host for the available supply of vitamin B12 leading to its deficiency - Also caused by some toxins secreted by the parasite Diagnosis: 1- Stool examination - Show operculated eggs or - Worm segments 2- CBC pernicious anemia Treatment: as T.saginata
D-Hymenolepis nana and Diminuta Pathogenesis 1- Infective stage - Egg (H.nana only) - Cesticercoid larva in body cavity of vectors (in both) 2- Definitive host man ( rare in H.diminuta) & rat, mice 3- Habitat small intestine 4- I.H. man (H.nana), various insects (fleas, beetles) 5- Mode of infection: - Direct ingestion of eggs along contaminated food, water and hands ( in both) - Internal and external autoinfection (H.nana) - Ingestion of cysticercoids in infected insects along contaminated food and drink (H.nana)
Clinical features 1- Asymptomatic in light infection 2- Intestinal disturbances (irritation) - Vomiting, recurrent diarrhea, abdominal pain, anorexia 3- Nervous manifestations - Dizziness, insomnia and convulsions due to absorption of metabolic by-products Diagnosis - Detection of eggs in faecal smear
Treatment 1- Praziquantel(The drug of choice) - 25 mg /kg single oral dose is highly effective - Treatment should be repeated after 10 days 2- Niclosamide - 2 gm/day for 5-7 daysand it affects adult worms only - Treatment should be repeated after 3 weeks 3- Treat all members of the family at the same time
(3) Intestinal nematodes: 1-Ascaris Pathogenesis 1- Infective stage - Mature egg with the 2 ndstage rhabditiform larva 2- Definitive host man 3- Habitat small intestine 4- Mode of infection - Ingestion of mature eggs containing the 2 nd stage larva with contaminated food (green raw vegetables), water or hands
Clinical features 1- Migrating larvae (Ascaris pneumonitis) Fever, cough with sputum, dyspnea, wheeze and urticaria 2- Adult worms - Abdominal colic, distension, dyspepsia, diarrhea or constipation - Anorexia or polyphagia - Lactose intolerance and malabsorptionof vitamin A and other micronutrients may occure malnutrion - By-products of living or dead worms: Fever, urticaria, ashma, insomnia or even epileptiform attacks may occur esp. in children - Intestinal obstruction or volvulus - Wandering adult worms may be extensive and possibly pass to different ectopic sites as appendix, common bile duct, ..