Paediatric Occupational Therapy in Childhood Cancer: Strategies & Challenges
Discover the intricacies of paediatric occupational therapy in childhood cancer, from managing brain tumors to coping strategies. Explore the impact of treatments like radiotherapy and chemotherapy on children's physical and emotional well-being, along with potential side effects and long-term considerations.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
3rd National Conference for Occupational Therapists Working in Diverse Settings 5th September 2018 From Managing Brain Tumours to Empowering Children s Self- Identity Deciphering the role of paediatric occupational therapy in acute oncology Mubeena Tarzi, Specialist Paediatric Occupational Therapist @MubeenatheOT
Overview Introduction to the service and the complexity of treating children with cancer Occupational Therapy for children with cancer Processes and strategies for coping in a new role
Paediatric Occupational Therapy in Oncology Mainly working with children with cancer Adult OT department MDT working and meetings Service specialist radiotherapy centre Very complex care provision for patients
Types of Cancer in Children Children s Cancer and Leukaemia Group
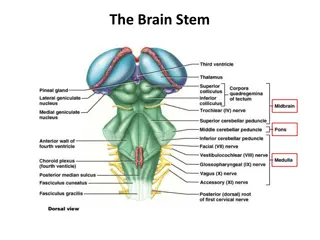
Brain Tumours Presentation Headaches Vomiting Fits Balance & ataxia Irritability Delayed or arrested puberty Losing interest Fatigue Head tilt Balance & ataxia Weakness Diagnosis CT scan MRI scan Brain angiogram scan Lumbar puncture Blood tests Biopsy
Radiotherapy: short term side effects Fatigue Growth and development Puberty Hair loss Intellectual development Skin sensitivity Cognitive impairment Feeling nauseous Emotional difficulties Reduced appetite
Radiotherapy: long term side effects Growth and development Puberty Intellectual development and cognitive impairment Emotional difficulties Risk of secondary tumours
Chemotherapy: side effects Reduced no. of blood cells produced - bruising, bleeding, infections - isolation, barrier nursing Neuropathy / Neurotoxicity Nausea & Vomiting = Weight Loss Diarrhoea & feeding problems Mucositis Hair Loss Seizures / Neurological changes
Side effects Chemotherapy Cont: Fatigue Deconditioning Cognition / Attention Hearing/Vision Loss Headaches Pain Steroids: Increased appetite Weight gain Mood changes/irritable Osteopenia
Late Effects of Cancer Treatments Late effects in childhood cancer survivors may affect the following: Organs, tissues, and body function Growth and development Mood, feelings and actions Cognition - thinking, learning, and memory Social and psychological adjustment Risk of secondary cancers and/or relapse
Psychosocial Aspects Visual effects Fatigue Pain Grief Loss of identity Ricky s OT sessions Peer group Variable family support Suicidal ideation Puberty, sexuality and fertility
Background Information Difficulties: Diagnosis: Significant Bulbar Palsy Grade Posterior Fossa Convergent squint Brain Tumour Ataxia Right side and centrally Grade III Anaplastic Reduced power Right UL + LL Ependymoma Increased tone Left LL > UL Surgical resection local Strong head preference Left PICU Oral secretions++ Tracheostomy Family live in static caravan
Functional Presentation Required full head and trunk support to sit Able to roll from her supine to side Tolerates short periods in prone Enjoys flashing and musical toys locates with eyes and head positioning Able to maintain grasp of object in each hand L>R Bangs and swings objects around Right thumb abducted - resting in palm
Longer-term Acute OT input 1. Followed up community referrals seating, splinting and housing 2. Rehab sessions focusing on upper limb function crossing midline, CIMT, grasp, release, exploring toys with both hands, back extensors, supported sitting on a mat, choosing between two toys, communication skills. 3. Respecting the cancer journey timing of interventions 4. Therapeutic relationship getting to know patients and families 5. Windows of opportunity for rehabilitation during radiotherapy 6. Managing expectations with rehab, seating and housing complicated discharge plans! 7. Ongoing dialogue between acute services and liaison with community services
Community OT input Long term Rehab setting Pre-assessment at hospital, support with transfer to Tadworth, prepare families. Undertake rehab therapy once transferred to rehab setting. Social Service House not suitable for double side access cot or seating. Did not accept referral considered it a health issue. Health Completed home visit completed initial home setup plan Supported with liaison with Social Services OTs Wheelchair services Fast-tracked Snappi referral
Processes and strategies for navigating new waters It takes 9 months try not to run away in your first week Learning theory Living with imposter syndrome you are an evolving therapist Learn about other people s role in the team collaboration Write down ideas to develop the service Learning about the therapeutic environment Networking with other OTs filling in service gaps, CYPF, RCOT
References and Resources Brain tumours in children - Macmillan Cancer Support 2016 Children and young people with cancer: Guidance for occupational therapists (COT 2010) Children and Young People with Cancer:A Parent s Guide (2014) Children s Cancer and Leukaemia Group CLIC Sargent My child has a brain or spinal tumour - A guide for parents and carers www.cclg.org.uk Occupational therapy in Oncology and Palliative Care 2nd Ed. (2006) The Brain Tumour Charity www.thebraintumourcharity.org.uk
Thanks for listening.. .get in touch @MubeenatheOT