Pelvic Inflammatory Disease: Definition, Aetiology, and Complications
Pelvic inflammatory disease (PID) is a clinical diagnosis indicating upper genital tract infection and inflammation, primarily affecting the fallopian tubes, leading to various complications if left untreated. This article explores the causes, symptoms, diagnosis, and treatment of PID, emphasizing the importance of early detection and management to prevent long-term health issues.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
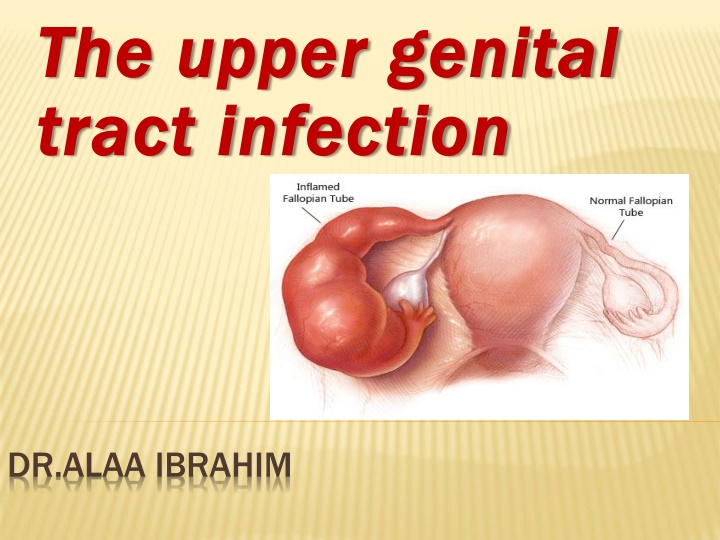
The upper genital The upper genital tract infection tract infection http://blog.shadygrovefertility.com/wp-content/uploads/2012/10/pelvic-inflammatory-disease-pid.jpg DR.ALAA IBRAHIM
Objectives: Objectives: - -Definition of pelvic inflammatory disease Definition of pelvic inflammatory disease - - Aetiology Aetiology and pathogenesis and pathogenesis - - Incidence and mode of transmission Incidence and mode of transmission - - Risk Factors Risk Factors - - Diagnosis Diagnosis - - Treatment Treatment - -complication complication
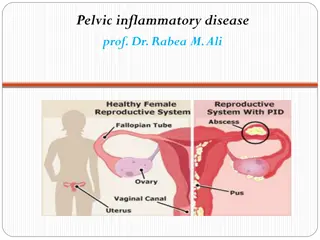
PELVIC INFLAMMATORY DISEASE Definition: Definition: PID is a clinical diagnosis implying that the patient PID is a clinical diagnosis implying that the patient has upper genital tract infection and inflammation has upper genital tract infection and inflammation ,arising from ,arising from endocervix endocervix leading to salpingitis salpingitis, , oophoritis oophoritis, pelvic peritonitis and , pelvic peritonitis and subsequently formation of subsequently formation of tubo abcesses abcesses. . - -Although all may be involved, the organ of Although all may be involved, the organ of importance, with or without abscess formation, is importance, with or without abscess formation, is the fallopian tube. the fallopian tube. leading to endometritis endometritis, , tubo- -ovarian and pelvic ovarian and pelvic
Aetiology Aetiology and pathogenesis and pathogenesis : : 1.Ascending infection from endocervix to the Disease endometrium and fallopian tubes, commonly is caused by sexually transmitted N. gonorrhoeae and C. trachomatis , BV micro- organisms, may also isolated from upper GT. 2-Other causes include abortion, childbirth (because of raw placental site, breaks in the epithelial lining of the cervix and vagina, discharge of both liquor and lochia , degenerated blood clots and fragments of decidua offer a nidus for infection.
When infection spreads upwards from the cervix (entrance to the uterus), it causes one or more of the followings:- - Endometritis Endometritis: inflammation and infection of the endometrium. - Salpingitis Salpingitis: inflammation and infection of the fallopian tubes. - Oophoritis Oophoritis: inflammation and infection of the ovaries. - Salpingo Salpingo- -oophoritis oophoritis.
- Parametritis Parametritis: inflammation and infection of the tissue around the uterus.- - -Tubo Tubo- -ovarian ovarian abscess abscess: a pocket of infected fluid in the ovary and fallopian tube.- - -Pelvic Pelvic peritonitis peritonitis: inflammation and infection of the peritoneum (lining of the inside of the abdomen). - Perihepatits Perihepatits ( Fitz-Hugh Curtis syndrome )
Incidence and mode of transmission Incidence and mode of transmission: : -Direct, lymphatic and Direct, lymphatic and haematogenous haematogenous. . - -Occur in Occur in 2 2% of sexually active women % of sexually active women
Risk Factors Risk Factors: : -Multiple sexual Multiple sexual parteners,and partner(s) partner(s) Lower socioeconomic status. Lower socioeconomic status. STD. STD. Previous diagnosis of pelvic inflammatory disease. Previous diagnosis of pelvic inflammatory disease. intrauterine contraceptive devices for the intrauterine contraceptive devices for the 1 1st st3 3 weeks of insertion. weeks of insertion. HSG. HSG. IVF and IUI. IVF and IUI. parteners,and recent new sexual recent new sexual
Diagnosis: Diagnosis: Pelvic inflammatory disease can be classified into "silent" Pelvic inflammatory disease can be classified into "silent" PID , acute and chronic PID. PID , acute and chronic PID. 1 1. Silent Pelvic Inflammatory Disease: . Silent Pelvic Inflammatory Disease: -This condition results from multiple or continuous low- grade infection in asymptomatic women. - It is an ultimate diagnosis given to women with tubal- factor infertility who lack a history compatible with upper tract infection. -At laparoscopy or laparotomy, these patients may have evidence of prior tubal infection such as adhesions, but for the most part the fallopian tubes are grossly normal.
2 2. Acute Pelvic Inflammatory Disease: . Acute Pelvic Inflammatory Disease: Signs and symptoms: Signs and symptoms: can vary, in women who are symptomatic, symptoms develop during or following menstruation.
the the clinical Criteria clinical Criteria for the Diagnosis of acute PID Diagnosis of acute PID: Pelvic tenderness and cervical excitation Pelvic tenderness and cervical excitation during examination: elicited by quickly displacing the cervix laterally with examining vaginal fingers by bimanual examination. Uterine tenderness Uterine tenderness. Tender Tender adnexal adnexal or palpable ovarian mass. for the
Additional criteria Additional criteria to increase the specificity of the diagnosis specificity of the diagnosis: : to increase the Mucopurulant Mucopurulant vaginal discharge vaginal discharge. Elevated C Elevated C- -reactive protein reactive protein or erythrocyte sedimentation rate(ESR) ESR). Temperature Temperature higher than 38 C. Raised WBC Raised WBC( neutrophilia suggestive of acute inflammatory process), while reduced WBC( neutropenia in sever infection
Definitive criteria: Definitive criteria: Ultrasound Ultrasound -documenting tubo-ovarian abscess Laparoscopy Laparoscopy -visually confirming salpingitis ( tubal wall edema, and purulent exudate issuing from the fimbriated ends and pooling in the cul- de-sac confirm this diagnosis).
Screening for other STI Screening for other STI- especially those with positive results for gonorrhoea and chlamydia or patient at high risk for STI : Microscopy and/or culture for Trichomonas vaginalis. HIV antibody test. Syphillis serology. Urine analysis and urine culture to exclude UTI.
3 3.Chronic Pelvic Inflammatory Disease : .Chronic Pelvic Inflammatory Disease : -This diagnosis is given to women who describe a history of acute PID history of acute PID and who have pelvic pain. - A hydrosalpinx hydrosalpinx might qualify as a criterion for this diagnosis. -It is a histologic histologic diagnosis diagnosis (chronic inflammation) made by a pathologist. Thus, the clinical utility of this diagnosis is limited.
Treatment: Treatment: The primary goal of therapy is to eradicate bacteria, The primary goal of therapy is to eradicate bacteria, relieve symptoms, and prevent relieve symptoms, and prevent adverse squeal Tubal damage or occlusion Tubal damage or occlusion resulting from infection may lead to infertility, rates following one episode approximate 15 %; two episodes, 35 %; and three or more episodes, 75 % ectopic pregnancy ectopic pregnancy -6 to 10-fold and may reach a 10- percent risk for those who conceive. chronic pelvic pain ( chronic pelvic pain (15 to 20 %). recurrent infection recurrent infection (20 to 25 %). abscess formation abscess formation (5 to 15 %). . Intestinal adhesions and obstruction. Intestinal adhesions and obstruction. Reiter Reiter s syndrome (reactive arthritis). s syndrome (reactive arthritis). adverse squeal : :
Guidelines for Treatment of Pelvic Inflammatory Disease: Guidelines for Treatment of Pelvic Inflammatory Disease: Depending on the severity of the infection Depending on the severity of the infection- - 1 1. Outpatient Treatment( oral therapy) in mild . Outpatient Treatment( oral therapy) in mild moderate infection: infection:. -If women do not respond to oral therapy within 72 hours, re- evaluation is indicated and parenteral therapy should be initiated either as an inpatient or as an outpatient . Ceftriaxone, 250 mg single intramuscularly injection Plus Doxycycline, 100 mg orally 2 times daily for 14 days With or without Metronidazole, 500 mg orally 2 times daily for 14 days. moderate Oral Ofloxacin, 400 mg orally 2 times daily for 14 days plus Metronidazole, 500 mg orally 2 times daily for 14 days. Ceftriaxone, 250 mg single intramuscularly injection plus Azithromycin 1 g / week for 2 weeks.
2 2.Inpatient Treatment( .Inpatient Treatment(Parenteral Indications for hospitalization Indications for hospitalization: : recommended for parenteral treatment for at least 24 hours. - -When the diagnosis is uncertain. -pelvic abscess is suspected. -clinical disease is severe. -compliance with an outpatient regimen is in question. -Drug addicts -Generalized peritonitis -Recent intrauterine instrumentation -White blood cell count >15,000/mm3 Parenteral Treatment): Treatment):
Principles of treatment Principles of treatment : : Adequate supporative care. strict watch on fluid balance. parenteral Antibiotics : Antibiotics : Ceftriaxone Ceftriaxone 2 g i.v. every 6 hours, or Cefotetan Cefotetan, 2 g i.v.every 12 hours, + + doxycycline 100 mg orally or intravenously every 12 hours, + + i.v. i.v.metronidazole metronidazole 500 mg twice daily. Should be continued until the patient gets clinically better which is usually within 24 hours, then changed to oral therapy for 14 days. doxycycline, ,
Surgical treatment Surgical treatment: :- - Considered in : 1 -severe cases not respond to treatment. 2 -clear evidence of a pelvic abscess not resolved by antibiotic therapy. - -Laparotomy Laparotomy/laparoscopy: /laparoscopy: 1.early resolution of the disease by division of adhesions and drainage of pelvic abscess. 2. exclude other causes of pain like appendicitis, endometriosis, ovarian pathology- remove affected ovary. - - U/S U/S- -guided guided aspiration aspiration of pelvic fluid collections is less invasive and may be equally effective. - - Depending on age and reproductive history, salpingo salpingo- -oopherectomy oopherectomy done for extensive damage.
Complications of PID: Complications of PID: . Recurrent pelvic inflammatory disease: The condition can return if the initial infection is not entirely cleared, often because the course of antibiotics was not completed of antibiotics was not completed, or because a sexual partner sexual partner has not been tested and treated. If an episode of PID damages the uterus or damages the uterus or fallopian tubes fallopian tubes, it can become easier for bacteria to infect these areas in the future 1 1. Recurrent pelvic inflammatory disease: course
2 2. . Tubo Tubo- -ovarian Abscess ovarian Abscess: : Is an end Is an end- -stage process of acute PID stage process of acute PID, diagnosed when a patient with PID has a pelvic mass that is palpable during bimanual examination. The condition usually reflects an agglutination of pelvic organs (tube, ovary, bowel) forming a palpable complex. Occasionally, an ovarian abscess can result from the entrance of micro- organisms through an ovulatory site.
Treatment Treatment -with an antibiotic regimen a antibiotic regimen administered in ahospital ,75% respond to antimicrobial therapy alone. Failure of medical therapy suggests the need for drainage of the abscess drainage of the abscess . Although drainage may require surgical exploration, percutaneous drainage guided by imaging studies (ultrasound or computed tomography) should be used as an initial option if possible. Trocar drainage, with or without placement of a drain, is successful in up to 90% of cases in which the patient failed to respond to antimicrobial therapy after 72 hours .salpingo salpingo - -oophorectomy oophorectomy in severe damage.
3 3. Long . Long- -term pelvic pain: term pelvic pain: you may be given painkillers to help control your symptoms and tests to determine the cause may be carried out. 4 4.Ectopic pregnancy .Ectopic pregnancy: If PID infects the fallopian tubes, it can scar the lining of the tubes, making it more difficult for eggs to pass through. If a fertilised egg gets stuck and begins to grow inside the tube,
5 5.Infertility .Infertility Blocked or damaged fallopian tubes can sometimes be treated with surgery, but if this is not possible and you want to have children, you may want to consider an assisted conception technique such as in-vitro fertilisation (IVF).
Sausage shape dilated right fallopian tube Sausage shape dilated right fallopian tube (arrow) (arrow)
Doppler ultrasound Doppler ultrasound - -Tubo Tubo ovarian ovarian abcessess abcessess
Laparoscopic Laparoscopic appendicectomy appendicectomy in patient with pelvic inflammatory disease inflammatory disease in patient with pelvic
Liver adhesions in Fitz Liver adhesions in Fitz- -Hugh syndrome syndrome Hugh- -curtis curtis
Fitz Fitz- -Hugh Hugh- -curtis curtis syndrome syndrome
THANK YOU THANK YOU