PERIPHERAL PRECOCITY
Precocious puberty is the early onset of puberty, with peripheral precocity being one of its classifications. This condition results from excess secretion of sex hormones outside of the hypothalamic-pituitary-gonadal axis, leading to early development of secondary sexual characteristics. Learn about the causes, characteristics, and prevalence of peripheral precocious puberty.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
PERIPHERAL PRECOCITY Peripheral precocious puberty Gonadotropin-independent precocious puberty Dr. Payam Samei
References 1. Williams 2016 2. Sperling 2014 3. Up to Date 2017
INTRODUCTION Precocious puberty is the onset of pubertal development at an age that is 2 to 2.5 standard deviations (SD) earlier than population norms.
DEFINITION Precocious puberty is traditionally defined as the onset of secondary sexual characteristics before the age of eight years in girls and nine years in boys.
DEFINITION Definition of precocious puberty is problematic, at least in girls; Not only depend on age ; Clinical features Race/ethnicity Presence/absence of obesity
DEFINITION (Age of Puberty) Caucasian girls seven years of age African-American girls six years of age. (controversial)
DEFINITION There is a strong female predominance of children with precocious puberty. Children referred for evaluation of precocious puberty, 87 percent were female.
EPIDEMIOLOGY Prevalence rate should be around 2 percent, or 2 in every 100 children.
CLASSIFICATION Central precocious puberty Peripheral precocity Benign or non-progressive pubertal variants
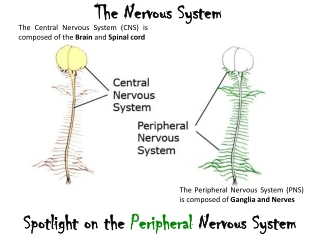
Central precocious puberty (CPP) Central precocious puberty is caused by early maturation of the hypothalamic-pituitary-gonadal axis.
CPP In these patients, the sexual characteristics are appropriate for the child's gender (isosexual).
Peripheral precocity Peripheral precocity : Excess secretion of sex hormones (estrogens or androgens) from the gonads or adrenal glands Exogenous sources of sex steroids Ectopic production of gonadotropin from a germ cell tumor (eg, human chorionic gonadotropin, hCG)
Peripheral precocity Further characterization is based upon whether the sexual characteristics are appropriate for the child's gender (isosexual) or inappropriate, with virilization of girls and feminization of boys (contrasexual).
Peripheral precocity Follicle-stimulating hormone (FSH) and luteinizing hormone (LH) levels are suppressed (in the prepubertal range) and do not increase substantially with gonadotropin-releasing hormone (GnRH) stimulation.
Peripheral precocity The approach to treatment for peripheral precocity depends on the cause. GnRH agonist therapy is ineffective, in contrast to patients with central precocious puberty (CPP).
Benign or non-progressive pubertal variants Benign pubertal variants : Isolated breast development in girls (premature thelarche) Isolated androgen-mediated sexual characteristics (such as pubic and/or axillary hair, acne, and apocrine odor)
Peripheral precocity Girls only Boys only Girls and boys
Girls only Ovarian cysts Ovarian tumor
Boys only Leydig cell tumor hCG-secreting germ cell tumors Familial male-limited precocious puberty
Girls and boys Exogenous sex steroids (estradiol and testosterone creams) McCune-Albright syndrome (girls>boys) Primary hypothyroidism Congenital adrenal hyperplasia (untreated) Virilizing adrenal tumor
Ovarian cysts A large functioning follicular cyst of the ovaries is the most common cause of peripheral precocity in girls. Affected patients often present with breast development, followed by an episode of vaginal bleeding, which occurs due to estrogen withdrawal once the cyst has regressed.
Ovarian cysts Chronic abdominal aching pain, either periumbilical or localized to a lower quadrant, may be present.
Ovarian cysts These cysts may appear and regress spontaneously, so conservative management is usually appropriate. Large cysts may predispose to ovarian torsion.
Ovarian cysts An ovarian mass that is: Purely cystic Few internal echoes No complex features (septation, increased solid tissue, or calcification) Almost certainly benign and can be managed by observation.
Ovarian cysts A follow-up ultrasound examination in four to eight weeks should be performed. If the cyst has not resolved and the ultrasonic characteristics are still reassuring, then continued observation is appropriate as long as the girl remains asymptomatic.
Ovarian cysts Torsion : Nausea Vomiting Pallor Leukocytosis (with left shift) Followed by less severe localized pain
Ovarian cysts Autonomously functioning ovarian follicular cysts, whether recurrent or manifesting in an isolated episode, often respond to treatment with oral medroxyprogesterone acetate, which seems to prevent recurrence, to accelerate involution of the follicular cysts, and to reduce the risk of torsion.
Ovarian cysts The use of a potent aromatase inhibitor such as letrozole to reduce estradiol secretion is another potential approach to treatment.
Ovarian tumors Ovarian tumors are a rare cause of peripheral precocity in girls. Granulosa cell tumors, the most common type, typically present as isosexual precocity.
Leydig cell tumors Leydig cell tumor should be considered in any boy with asymmetric testicular enlargement. These testosterone-secreting tumors are almost always benign and are readily cured by surgical removal
hCG-secreting germ cell tumors Germ-cell tumors secrete hCG, which in boys activates LH receptors on the Leydig cells, resulting in increased testosterone production.
hCG-secreting germ cell tumors The increase in testicular size (usually only to an early pubertal size) is less than expected for the serum testosterone concentration and degree of pubertal development. This is because most of the testis is made up of tubular elements whose maturation depends upon FSH.
hCG-secreting germ cell tumors In girls, hCG-secreting tumors do not lead to precocious puberty because activation of both FSH and LH receptors is needed for estrogen biosynthesis.
hCG-secreting germ cell tumors All males with anterior mediastinal germinomas should have a karyotype because these tumors may be associated with Klinefelter syndrome.
Familial male-limited precocious puberty (Familial testotoxicosis) Activating mutation in the LH receptor gene, which results in premature Leydig cell maturation and testosterone secretion. Inherited as an autosomal dominant.
Familial testotoxicosis Affected boys typically present between one to four years of age.
Primary hypothyroidism Children with severe, long-standing primary hypothyroidism occasionally present with precocious puberty. (Van Wyk Grumbach syndrome)
Primary hypothyroidism In girls, this syndrome is often characterized by : Galactorrhea : Often not spontaneous; a few drops of milky fluid may become apparent only upon milking the subareolar ductal tissue. Multicystic ovaries : Often demonstrable by ultrasonography. Recurrent vaginal bleeding
Primary hypothyroidism In boys present with: Premature testicular enlargement
Primary hypothyroidism A unique diagnostic feature of the Van Wyk Grumbach syndrome is the combination of delayed bone age with apparent sexual precocity.
Primary hypothyroidism Boys with this syndrome have macroorchidism without significant virilization.
Primary hypothyroidism A proposed mechanism is cross-reactivity and stimulation of the FSH receptor by high serum thyrotropin (TSH) concentrations, given that both TSH and FSH share a common alpha subunit. The signs of pubertal development regress with thyroxine therapy.
Exogenous sex steroids Feminization, including gynecomastia in boys, has been attributed to excess estrogen exposure from creams, ointments, and sprays. Caretakers using these topical estrogens to treat menopausal symptoms may inadvertently expose children to the hormones.
Exogenous sex steroids A short course of application of estrogen cream is used to treat labial adhesions, but long courses may lead to breast development or even withdrawal bleeding.
Exogenous sex steroids In addition to breast development, pigmentation of the areolae and the linea alba and the appearance of pubic hair may be seen in children exposed to dermal estrogen.
Exogenous sex steroids FDA guidelines define a limit of not more than 1% of normal daily estrogen production in prepubertal children as a safe intake of estrogen: Boys : 0.43 ng/day Girls : 3.24 ng/day
Exogenous sex steroids Children who touch the skin or the towels of men using androgen gel therapy may themselves develop virilization.