Physiology of Male Reproduction and Hormonal Control of Spermatogenesis
Delve into the intricate workings of male reproductive physiology with a focus on the hormonal regulation of spermatogenesis. Explore the processes governing male fertility and the intricate balance of hormones that orchestrate the creation of sperm. Gain insights into the physiological mechanisms crucial for understanding male reproductive health and function.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Physiology of Male Reproduction and Hormonal Control of Spermatogenesis General Semester 2nd
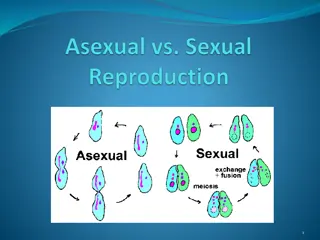
Spermatogenesis Spermatogenesis: The process by which stem cells develops into mature spermatozoa. There are three phases: Spermatocytogenesis (Mitosis), Meiosis, and Spermiogenesis.
Spermatocytogenesis Spermatocytogenesis (also called Mitosis): Stem cells (Type A spermatogonia; singular = spermatogonium) divide mitotically to replace themselves and produce cells that starts the differentiation. (Type B spermatogonia). structurally have spherical or oval nuclei. Spermatogonia
Cell Division Meiosis: Cells in prophase of the first meiotic division are primary spermatocytes. They are characterized by highly condensed chromosomes giving the nucleus a coarse chromatin pattern and an intermediate position in the seminiferous epithelium. Primary spermatocytes go through the first meiotic division spermatocytes. The cells then proceed through this stage and complete the second meiotic division. Because this stage is short there are few secondary spermatocytes to be seen in sections. Meiosis is basically the process by which the diploid number of chromosomes present in spermatogonia (the stem cells) is reduced to the haploid spermatozoa. and become secondary number present in mature
The products of the second meiotic division are called spermatids. They are spherical cells with interphase nuclei, positioned epithelium. Since spermatids metamorphosis into spermatozoa, they occur in early through late stages. You are not responsible for distinguishing the different stages of spermatids, but you are required to identify a spermatid. All of these progeny cells remain attached to each other by cytoplasmic bridges. The bridges remain until sperm are fully differentiated. high go in the through a
Spermiogenesis This is the metamorphosis of spherical spermatids into elongated spermatozoa. No further mitosis or meiosis occurs. During spermiogenesis, flagellar apparatus forms, and most excess cytoplasm (the residual body) is separated and left in the Sertoli cell. Spermatozoa are released into the lumen of the seminiferous tubule. A small amount of excess cytoplasm (the cytoplasmic droplet) is shed later in the epididymis. the acrosome forms, the
Spermiogenesis It is the process of metamorphosis from a round cell with typical organelles to a highly specialized, elongated cell well adapted for traversing the male and female reproductive tracts and achieving fertilization of an egg. Transition: Spermatid to spermatozoan
Sertoli Cell & Developing Sperm Cells: An interaction The Interaction At all stages of differentiation, the spermatogenic cells are in close contact with Sertoli cells which are thought to provide structural and metabolic support to the developing sperm cells. A single Sertoli cell extends from the basement membrane to the lumen of the seminiferous tubule although its cytoplasm is difficult to distinguish at the light microscopic level. They are characterized by the presence of a vesicular, oval, basally positioned nucleus which contains a prominent nucleolus. The nuclear envelope often contains a definite fold. The significance of the very close association of the two types of cells is unknown. Sertoli cells are endocrine cells - they secrete the polypeptide hormone, inhibin. Inhibin acts at the level of the pituitary to reduce the secretion of follicle stimulating hormone.
Blood-testis barrier . Large molecules cannot pass from the blood into the lumen of a seminiferous tubule due to the presence of tight junctions between adjacent Sertoli cells. The spermatogonia are in thebasal compartment and the more mature forms such as primary and secondary spermatocytes and spermatids are in the adluminal compartment. The function of the blood-testis barrier (red highlight in diagram above) may be to prevent an auto-immune reaction. Mature sperm (and their antigens) arise long after immune tolerance is established; therefore, a male animal is capable of making antibodies against his own sperm. Injection of sperm antigens causes inflammation of the testis (autoimmune orchitis) and reduced fertility. Thus, the blood-testis barrier may reduce thelikelihood that sperm proteins willinduceanimmuneresponse. Hormonal Control of Spermatogenesis
Note The contents and pictures have been prepared by extensive browsing in internet using various websites .