Pilot Audit Results for Suspected Malignancy Imaging Pathway
Audit findings from a pilot study on GP access to body CT for suspected malignancy, showing appropriate referrals, cancer detection rates, and non-cancer findings, with insights to streamline the cancer pathway.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
GP access to body CT for suspected malignancy Pilot audit results Dr Allan Green/Dr Stephen Glancy, Radiology, NHS Lothian
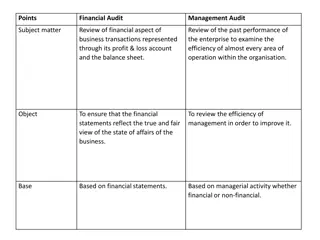
Referrals 28 referrals 1 patient refused scan; 1 request was actually for CT brain; 1 should have been an Ultrasound 25 CT Chest, Abdomen and Pelvis scans performed 88% (22/25) referrals appropriate for pathway, 12% (3/25) should have been arranged by secondary care. 100% (25/25) appropriate for CT scanning
Referral to Scan Mean time from referral to scan 21 days 50.00 45.00 40.00 35.00 30.00 25.00 20.00 15.00 10.00 5.00 0.00
Patients 4.5 Mean age 70.8 12 Male 13 Female 4 3.5 3 2.5 2 1.5 1 0.5 0 <50 50-55 56-60 61-65 66-70 71-75 76-80 81-85 Male Female
Cancer pickup 24% (6/25) definite cancers 2 Lung 2 Pancreas 1 Renal 1 Cervical Positive Negative 5% (1/25) possible cancer 1 Lung Positive Negative
Other findings Overall (14/28) 50% 1 Renal calculi 1 PE 2 Pneumonia 2 Hydronephrosis 1 Rib fractures 2 Vertebral fractures 1 Cirrhosis 1 Asbestos lung disease 1 Pancreatic cysts 1 Pulmonary nodule 1 Lung scarring
Referral to secondary care 20% (5/25) of patients scanned did not then require a secondary care referral Referrals to secondary care Referred Not Referred
25 Patients scanned Further tests 6 Cancer 1 probable 18 No cancer 13 Referred to secondary care 5 Not referred to secondary care 4 Follow up imaging 9 No follow up imaging
Summary Appropriate referrals Significant detection rate of cancers Significant reduction in referral to secondary care Significant relevant non cancer findings Education on using appropriate pathways Potential to significantly streamline the cancer pathway
FAQs How do I refer a patient for CT with a suspected malignancy? Refer to Guidance on RefHelp (URL...) Via SCI Gateway (URL...) What do I do if the CT I request reveals a malignancy? Refer as urgent to the appropriate specialty as normal. If the primary source is unclear, refer to the Cancer of Unknown Primary (CUP) Team or contact CUPTeam@nhslothian.scot.nhs.uk to discuss What do I do if there is an incidental finding on the CT? The report will often guide the referrer as to the most appropriate next step; often no action is required. Specific advice may be available on RefHelp. The reporting radiologist will also be able to advise on specific findings and is happy to be contacted. Renal or hepatic cysts do not generally merit any follow-up unless advised Atelectasis, tiny pulmonary nodules, sub-cm nodes, diverticular disease, bony haemangiomas and Tarlov s cysts are usually incidental findings How do I contact the reporting radiologist? NHS email is usually the easiest way to communicate. The duty radiologist in each department will also be available for advice. What if the patient has a CXR suspicious of malignancy? These patients should NOT be on the Vague Symptoms Pathway. There is an established Fast Track Suspected Lung Cancer Pathway at WGH (LCCWGH@nhslothian.scot.nhs.uk) , SJH (SJH.Respiratory@nhslothian.scot.nhs.uk ) and RIE (0131 242 1867) What if I request an US which shows suspected liver metastases, but no obvious primary? These patients should NOT be on the Vague Symptoms Pathway. Sometimes the Radiology department will arrange further imaging or suggest the appropriate next step. The CUP team are happy to be referred these patients (CUPTeam@nhslothian.scot.nhs.uk).