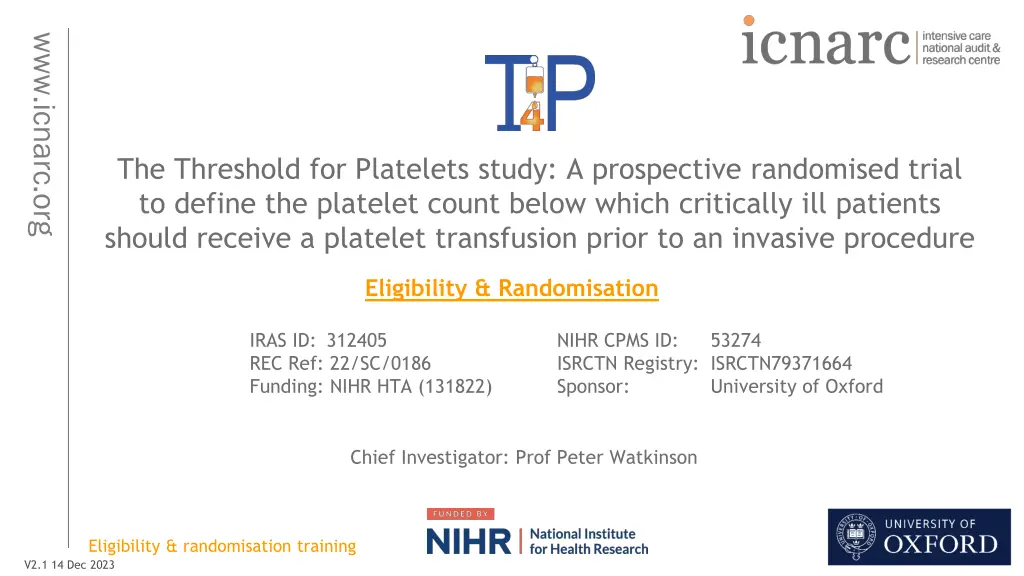
Platelet Threshold Study for Critically Ill Patients
Explore the Threshold for Platelets study, a prospective trial aiming to determine the platelet count necessary for critically ill patients before invasive procedures. Led by Prof. Peter Watkinson from the University of Oxford, this research investigates optimal platelet transfusion thresholds for improved patient outcomes in critical care settings.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
www.icnarc.org The Threshold for Platelets study: A prospective randomised trial to define the platelet count below which critically ill patients should receive a platelet transfusion prior to an invasive procedure Eligibility & Randomisation IRAS ID: 312405 REC Ref: 22/SC/0186 Funding: NIHR HTA (131822) NIHR CPMS ID: ISRCTN Registry: ISRCTN79371664 Sponsor: 53274 University of Oxford Chief Investigator: Prof Peter Watkinson Eligibility & randomisation training V2.1 14 Dec 2023 1
Agenda Trial overview and aim Screening Randomisation Platelet transfusion thresholds Consent/Safety www.icnarc.org Eligibility & randomisation training 2
Aim Define the optimum platelet threshold below which platelets should be transfused prior to an invasive procedure in critically ill patients www.icnarc.org Research question In adults with thrombocytopenia being considered for a platelet transfusion for a low bleeding risk invasive procedure in critical care what is the optimal platelet threshold (<10, <20, <30, <40 <50x109/L) below which platelets should be transfused prior to an invasive procedure Population Intervention & Comparator Outcome in terms of 90-day all-cause mortality? Eligibility & randomisation training 3
Trial design Open label, randomised, Bayesian adaptive, comparative effectiveness trial across five equally-spaced thresholds of thrombocytopaenia: <10x109/L <20x109/L <30x109/L <40x109/L <50x109/L Sample size: 2550 Setting: 66 NHS adult critical care units Recruitment period: Sept 2022 Dec 2025 www.icnarc.org o 1 patient/month/site Eligibility & randomisation training 4
Outcomes Primary o Clinical effectiveness: All-cause mortality at 90 days o Cost-effectiveness: Incremental costs, QALYs and net monetary benefit at 90 days www.icnarc.org Secondary o Mortality at discharge from critical care unit, hospital and at one year o Survival to longest available follow-up o Rates of major and fatal bleeding classified according to the HEME bleeding score o Venous and arterial thromboses in hospital and to one year o Duration of renal, advanced cardiovascular and advanced respiratory support o Length of critical care unit and acute hospital stay o Health related quality of life o Net monetary benefit at one year Eligibility & randomisation training 5
Local governance [localise slide details for your site] Transfusion team involvement o Understanding of trial design and platelet administration according to randomised threshold o Team to be aware of patients randomised to T4P Can be added to receive automated randomisation notification emails Clinical team to send patient details and randomised threshold at randomisation www.icnarc.org o Some teams are able to: Place alert on transfusion system for T4P patients and their allocated threshold Transfusion team will query non-adherence to randomised threshold To act as a polite reminder Eligibility & randomisation training 6
Agenda Trial overview and aim Patient flow o Screening o Randomisation o Platelet transfusion thresholds o Consent o Safety www.icnarc.org Eligibility & randomisation training 7
Patient flow www.icnarc.org Screening Randomisation Safety monitoring Platelet transfusion threshold: Data collection <10x109/L <20x109/L <30x109/L <40x109/L <50x109/L Consent Follow-up Eligibility & randomisation training 8
Eligibility Inclusion criteria 1. Adult (aged 18 years) 2. Accepted for admission or admitted to a participating critical care unit 3. Platelet count <50x109/L 4. Planned to undergo a specified* low bleeding risk invasive procedure OR platelet transfusion being considered for an other procedure www.icnarc.org *Specified low bleeding risk invasive procedures include: o Central venous vascular catheter insertion (including vascular access for renal replacement therapy) o Paracentesis/superficial abdominal fluid collection drainage o Pleural aspiration Eligibility & randomisation training 9
Eligibility Other procedures may be included if the clinician deems these to be a low bleeding risk invasive procedure and a platelet transfusion is being considered for the procedure Arterial catheter insertion Arterial or central venous catheter removal Pleural drain Interventional Radiology Bronchoscopy with or without lavage Wound dressing changes Surgical procedures where the clinical team agree risk of bleeding is low, e.g. re-look laparotomy or wound closure Percutaneous tracheostomy www.icnarc.org Other list is not exhaustive Eligibility & randomisation training 10
Eligibility inclusion criterion 4 Planned to undergo a specified* low bleeding risk invasive procedure o The patient is planned for a specified low bleeding risk invasive procedure OR platelet transfusion being considered for an other procedure o The patient is planned for an invasive procedure imminently, that is considered low bleeding risk and a platelet transfusion is being considered for this procedure In both cases, you are randomising the patient for this procedure, and they must be randomised prior to the procedure www.icnarc.org Eligibility & randomisation training 11
Eligibility Exclusion criteria 1. Ongoing major haemorrhage requiring blood products and/or surgical/radiological intervention www.icnarc.org 2. Intracranial haemorrhage within prior 72 hours 3. Contra-indication to platelet transfusion (such as thrombotic microangiopathies; heparin-induced thrombocytopaenia; immune thrombocytopaenia; congenital platelet function defects) 4. Acute promyelocytic leukaemia (APML) 5. Known advance decision refusing blood/blood component transfusions (e.g. Jehovah s Witnesses) 6. Death perceived as imminent or admission for palliation. 7. Previously randomised into T4P 8. Fulfilled all the inclusion criteria and none of the other exclusion criteria 72 hours Criteria 1 & 2 are dynamic, and if resolved, the patient may be reconsidered for the trial Eligibility & randomisation training 12
Screening Screening begins at the point of the decision to admit to a critical care unit Screen all patients daily until; o Recruitment, i.e. they meet all inclusion and no exclusion criteria o Refusal o Critical care unit discharge Eligibility should be documented in patient s medical notes Including name of low bleeding risk invasive procedure that deemed the patient eligible for inclusion www.icnarc.org Eligibility & randomisation training 13
Eligibility Fulfilled all the inclusion criteria and none of the other exclusion criteria 72 hours what does this mean? www.icnarc.org o Scenario 1 eligible on admission Meet eligibility 48 hours Admission 24 hours 72 hours 96 hours 120 hours 144 hours o Scenario 2 eligible during admission Meet eligibility 96 hours Admission 0 hours 48 hours 72 hours 24 hours Eligibility & randomisation training 14
Who can confirm eligibility A doctor, nurse, or clinical practitioner, as long as they are appropriately qualified, and have undergone study training as documented on the training log. Must still be overall oversight by a medically qualified doctor. o i.e., if the person confirming eligibility is not a doctor, they must receive agreement from the doctor responsible for the patient s care that the patient is suitable to be entered into the trial. Document this in the medical notes. The doctor responsible for the patient s care does not necessarily need to be trial trained. Note: If the doctor, nurse or clinical practitioner, is performing the eligibility/randomisation tasks ONLY, then they do not need to go on the delegation log. They can complete the training log once they have received trial training. www.icnarc.org Eligibility & randomisation training 15
Co-enrolment Observational studies (including those collecting samples) o Permitted without prior agreement www.icnarc.org Interventional studies o Decided on a trial-by-trial basis o Agreements in place with: ABC Tight-K UK-ROX MOSAICC iREHAB EMERALD BigpaK2 ADAPT-SEPSIS SWiFT FLO-ELA PRONTO GenOMICC A2B VitDALIZE MARCH Current co-enrolment agreement list found on T4P FAQs webpages: https://www.icnarc.org/Our-Research/Studies/Current-Studies/T4P/Information-For-Sites/Faqs Eligibility & randomisation training 16
Patient flow www.icnarc.org Screening Randomisation Safety monitoring Platelet transfusion threshold: Data collection <10x109/L <20x109/L <30x109/L <40x109/L <50x109/L Consent Follow-up Eligibility & randomisation training 17
Randomisation Dedicated 24/7 randomisation service o Sealed Envelope o Web randomisation Email T4P@icnarc.org to request an account Can use generic/group or individual email addresses www.icnarc.org Who can randomise? o Trial training required to randomise (documented on training log) o Appropriate clinical staff may be involved solely in the screening and randomisation of patients e.g. out-of-hours staff o GCP training not required to randomise Eligibility & randomisation training 18
Completion of the paper randomisation form is recommended before logging in to Sealed Envelope www.icnarc.org QR code to randomise on mobile device Details required by randomisation service Confirmation of inclusion/exclusion criteria Complete after confirmation of randomisation Enter the name of who confirmed eligibility, the doctor with medical oversight, and who randomised Completed paper randomisation forms should be provided to the research team at the next earliest convenience Eligibility & randomisation training 19
Sealed Envelope how to randomise online www.icnarc.org 1. Log in to Sealed Envelope via: https://www.sealedenvelope.com/access/ 2. Navigate to the Randomise tab Eligibility & randomisation training 20
Sealed Envelope how to randomise online (2) 3. Confirm Inclusion/Exclusion criteria www.icnarc.org Eligibility & randomisation training 21
Sealed Envelope how to randomise online (3) www.icnarc.org 4. Last exclusion criteria requires date and time that patient met all inclusion and none of the exclusion criteria note this should be no more than 72 hours before randomisation 5. Provide full name of person performing randomisation on Sealed Envelope 6. Your hospital name will automatically appear here 7. Once all eligibility criteria have been entered press Randomise Note: Sealed Envelope will only allow you to randomise if all questions have been answered and these indicate that the patient is eligible Eligibility & randomisation training 22
Sealed Envelope how to randomise online (4) www.icnarc.org 9. The randomisation result will appear as a pop-up, select ok to see details behind 8. A declaration will appear, enter your password and press Confirm 10. Trial ID, randomisation result and date/time of randomisation should be entered on the paper randomisation form and in the medical notes Eligibility & randomisation training 23
Randomisation Auto-generated randomisation notification emails o Email T4P@icnarc.org to add recipients www.icnarc.org Errors o Once randomised, patient is in trial and included in analysis consent and data collection must be carried out per protocol o If patient accidentally randomised twice use first randomisation Check email notification if unsure of the status of a randomisation or the Randomisations tab on Sealed Envelope (or contact local team/ICNARC CTU) Do not re-use the second randomisation details Eligibility & randomisation training 24
Patient flow www.icnarc.org Screening Randomisation Safety monitoring Platelet transfusion threshold: Data collection <10x109/L <20x109/L <30x109/L <40x109/L <50x109/L Consent Follow-up Eligibility & randomisation training 25
Possible randomisations (the Intervention) Patients randomised to one of five thresholds for platelet transfusion: www.icnarc.org <10x109/L <20x109/L <30x109/L <40x109/L <50x109/L below which they would receive a single adult equivalent dose (AED) of platelet transfusion delivered before or during a low bleeding risk invasive procedure Eligibility & randomisation training 26
Intervention Example scenarios: www.icnarc.org Platelet count: 38x109/L Platelet count: 38x109/L Randomised threshold: <20x109/L Randomised threshold: <40x109/L Administer platelets prophylactically before/during a low bleeding risk invasive procedure Do not administer platelets prophylactically before/during a low bleeding risk invasive procedure Eligibility & randomisation training 27
Local communication COMMUNICATE the treatment allocation to bedside staff Prescribe as appropriate Ensure appropriate treatment Document in medical notes Leave documents at bedside e.g. Bedside poster displaying allocated threshold [adapt for your site] www.icnarc.org Eligibility & randomisation training 28
Intervention Treatment according to the randomly allocated platelet threshold begins immediately following randomisation o Applies immediately to first procedure (i.e. the procedure that deemed the patient eligible to be randomised) and continues until critical care unit discharge o Applies to all subsequent invasive procedures deemed low bleeding risk o Decision of whether a procedure is deemed low/high bleeding risk should be documented in medical notes If re-admitted to critical care unit during the index hospital stay within 90 days, treatment according to the randomly allocated threshold should be recommenced www.icnarc.org Eligibility & randomisation training 29
Intervention Use most recent platelet count to inform intervention o These may change during course of critical care unit admission o Platelet counts may move across the allocated threshold for subsequent procedures, changing whether platelets are given/not given prophylactically www.icnarc.org Eligibility & randomisation training 30
Intervention Co-interventions o Where a patient is receiving a low bleeding risk invasive procedure, platelet prophylaxis is only permitted according to allocated randomised threshold o However, platelet administration should follow local guidance: For high bleeding risk interventional procedures Where significant bleeding occurs during or after a low bleeding risk invasive procedure Platelets given outside of any procedure www.icnarc.org Eligibility & randomisation training 31
Adherence to the intervention Non-adherence to the intervention will be defined as: o Receipt of platelet transfusion for low bleeding risk invasive procedure when platelet count is above randomised allocated threshold o Platelet transfusion not received for low bleeding risk invasive procedure when platelet count is below randomised allocated threshold www.icnarc.org Reasons for non-adherence should be documented locally Platelet administration deviation CRF to be completed on MACRO (by research staff) Eligibility & randomisation training 32
Team training / communication Ensure staff are aware of trial o They may be managing patients randomised to T4P o Awareness of randomised threshold and procedure inclusion o Discussion point at ward rounds o Including temporary/bank/agency staff o Bedside notices/posters/stickers provided by ICNARC CTU o Ensure clear documentation www.icnarc.org Eligibility & randomisation training 33
FAQs Use of TEG (thromboelastography) o Some units may routinely use TEG/ROTEM measurements to guide transfusion in stable critically ill patients, although this is not evidence based o For the trial use the most recent platelet count and adhere to the platelet threshold allocated on randomisation o If TEG has been used to guide platelet transfusion when platelet count is above the allocated threshold, then this will be a protocol deviation www.icnarc.org Eligibility & randomisation training 34
Patient flow www.icnarc.org Screening Randomisation Safety monitoring Platelet transfusion threshold: Data collection <10x109/L <20x109/L <30x109/L <40x109/L <50x109/L Consent Follow-up Eligibility & randomisation training 35
Research Without Prior Consent Patients likely to lack capacity at time of randomisation Emergency waiver of consent granted by REC (Mental Capacity Act) After randomisation - once patient s medical situation is considered no longer an emergency, the consent procedures should begin: o Consent sought by GCP-trained delegated team member o Expected to be within 24-48 hours of randomisation www.icnarc.org Eligibility & randomisation training 36
Patient flow www.icnarc.org Screening Randomisation Safety monitoring Platelet transfusion threshold: Data collection <10x109/L <20x109/L <30x109/L <40x109/L <50x109/L Consent Follow-up Eligibility & randomisation training 37
Safety monitoring If you consider there are any adverse events or reactions, please discuss with the PI/research team as soon as possible. www.icnarc.org For example: o Bleeding o Serious transfusion related adverse reactions Eligibility & randomisation training 38
FAQs Frequently asked questions and answers about T4P can be found here: https://www.icnarc.org/Our-Research/Studies/Current- Studies/T4P/Information-for-sites/FAQs www.icnarc.org Eligibility & randomisation training 39
Contacts www.icnarc.org Local research team PI: [XXXXX] Lead research nurse: [XXXXX] [any other local details] Eligibility & randomisation training 40
https://www.icnarc.org/Our-Research/Studies/Current-Studies/T4P/homehttps://www.icnarc.org/Our-Research/Studies/Current-Studies/T4P/home Lead Investigators Peter Watkinson (Chief Investigator) Simon Stanworth (Professor/Consultant) Akshay Shah (Research Fellow/Senior Registrar) Tim Walsh (Professor/Consultant) Duncan Young (Retired Professor/Consultant) Richard Grieve (Professor/Health Economist) Matteo Quartagno (Statistician) David Harrison (Head Statistician) Alexina Mason (Statistician) James Doidge (Senior Statistician) Doug Gould (Senior Researcher) Paul Mouncey (Head of Research) Joanna Calder (Patient Representative) www.icnarc.org ICNARC CTU Team Hayley Noble (Trial Manager) Niamh Wood (Research Assistant) Emma Laing (Senior Trial Manager) Julie Camsooksai (Clinical Research Assistant) Walton Charles (Clinical Research Assistant) Carly Au (Senior Data Manager) Nigel Osafo (Data Manager) Lamprini Lampro (Data Manager) Elisa Giallongo (Statistician) Doug Gould (Senior Researcher) Paul Mouncey (Head of Research) Eligibility & randomisation training 41