Platelet Transfusion Threshold Study: Issues and Uncertainties
Explore the ongoing study on defining the platelet count threshold for critically ill patients requiring platelet transfusions before invasive procedures. Learn about the challenges, risks, and potential benefits associated with prophylactic platelet transfusions in ICU settings. Gain insights into the factors influencing platelet counts, bleeding prediction, and the delicate balance between benefits and risks in patient care.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
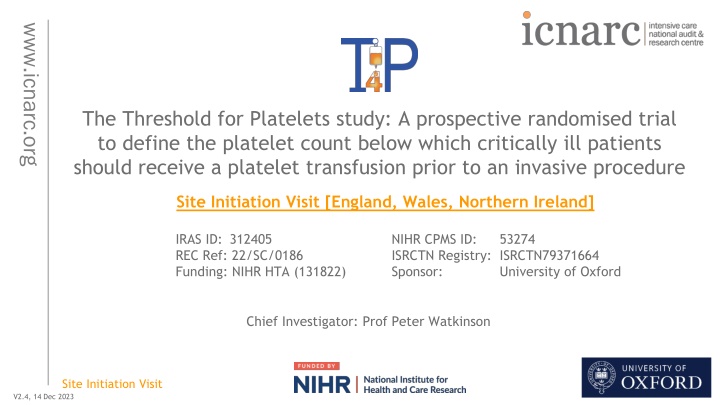
www.icnarc.org The Threshold for Platelets study: A prospective randomised trial to define the platelet count below which critically ill patients should receive a platelet transfusion prior to an invasive procedure Site Initiation Visit [England, Wales, Northern Ireland] IRAS ID: 312405 REC Ref: 22/SC/0186 Funding: NIHR HTA (131822) NIHR CPMS ID: ISRCTN Registry: ISRCTN79371664 Sponsor: 53274 University of Oxford Chief Investigator: Prof Peter Watkinson Site Initiation Visit V2.4, 14 Dec 2023 1
Agenda Background and trial design Governance Patient flow Support/resources www.icnarc.org Site Initiation Visit 2
Agenda Background and trial design Governance Patient flow Support/resources www.icnarc.org Site Initiation Visit 3
The problem: prophylactic platelet transfusions www.icnarc.org Thrombocytopenia is common in ICU patients (<50x109/L): 5-20% Multifactorial aetiology (sepsis, liver failure, cancer) ~9% will receive a platelet transfusion mainly for prophylaxis 2ndbiggest user of platelets (after cancer services) No high quality data to inform this practice! Evidence from non-ICU patients (PATCH, PLaNET-2) suggests harm Site Initiation Visit 4
What are the issues? Platelet count is a poor predictor of bleeding Assumption that transfusion will consistently raise platelet counts www.icnarc.org Modified by transfusion factors - storage age, ABO-matching Patient factors underlying illness (sepsis, cancer) Other effects of platelets immunomodulation Bleeding rates are low (0.1-3%) -> appropriate outcome measure? Arnold DM et al. Res Pract Thromb Haemost 2017; 1: 103-11 Gottschall J et al. Transfusion 2020; 60: 46 Shah A et et al. Transfus Med 2020; 30: 515-17 Aubron C et al. Crit Care 2018; 22: 185 Warner MA et al, Anesth Analg 2019l 128: 288-95 Site Initiation Visit 5
Uncertainties between benefits and risks www.icnarc.org Potential Risks Increased mortality? (critically ill neonates, intracranial bleed) Worse organ failure Transfusion reactions (x2 common with platelets) Potential Benefits Haemostasis Certain subgroups may benefit e.g. trauma, marrow failure Site Initiation Visit 6
Neonates: Primary outcome www.icnarc.org <25 (n=331) <50 (n=329) Odds ratio (95% CI) p-value PlaNeT 2 Major/severe bleed or mortality by day 28 61/329 (19%) 85/324 (26%) 1.57 0.02 (1.06 - 2.32) Number needed to harm = 100/(26-19) = 14.3 For every 14.3 patients treated with <50 strategy, 1 extra MB or death would be expected Adjusted for gestational age, presence of IUGR and centre Site Initiation Visit 7
PACER NEJM 2023 www.icnarc.org More than half of bleeding events were grade 2 bleeding that results in minor interventions to stop, such as prolonged manual compression >20 min Site Initiation Visit 8
Inconsistent guideline recommendations www.icnarc.org Site Initiation Visit 9
Surveys demonstrate variation in practice www.icnarc.org Transfusion Medicine, Volume: 30, Issue: 6, Pages: 515-517, First published: 12 October 2020, DOI: (10.1111/tme.12728) Site Initiation Visit 10
Aim Define the optimum platelet threshold below which platelets should be transfused prior to an invasive procedure in critically ill patients www.icnarc.org Research question Population In adults with thrombocytopenia being considered for a platelet transfusion for a low bleeding risk invasive procedure in critical care what is the optimal platelet threshold (<10, <20, <30, <40 <50x109/L) below which platelets should be transfused prior to an invasive procedure Intervention & Comparator Outcome in terms of 90-day all-cause mortality? Site Initiation Visit 11
Trial design Open label, randomised, Bayesian adaptive, comparative effectiveness trial across five equally-spaced thresholds of thrombocytopaenia: <10x109/L <20x109/L <30x109/L <40x109/L <50x109/L Recruitment www.icnarc.org o 42 months recruitment with 66 participating sites o Projected recruitment rate of 1 patient/month/site o First site opened 27 September 2022 Internal pilot runs for first 12 months of recruitment o Progression criteria: Sites open Recruitment rate Adherence to assigned platelet threshold Site Initiation Visit 12
The threshold response curve www.icnarc.org 5 treatment arms: different thresholds for transfusion Optimum threshold for transfusion Survival We will use the 5 treatment groups to model a threshold-response curve to find the optimum threshold (which may fall in-between the different thresholds assigned) Platelet count threshold Site Initiation Visit 13
Outcomes Primary o Clinical effectiveness: All-cause mortality at 90 days o Cost-effectiveness: Incremental costs, QALYs and net monetary benefit at 90 days www.icnarc.org Secondary o Mortality at discharge from critical care unit, hospital and at one year o Survival to longest available follow-up o Rates of major and fatal bleeding classified according to the HEME bleeding score o Venous and arterial thromboses in hospital and to one year o Duration of renal, advanced cardiovascular and advanced respiratory support o Length of critical care unit and acute hospital stay o Health related quality of life o Net monetary benefit at one year Site Initiation Visit 14
Agenda Background and trial design Governance Patient flow Support/resources www.icnarc.org Site Initiation Visit 15
Central governance Funder: NIHR Health Technology Assessment (HTA) Programme Sponsor: University of Oxford CTU: ICNARC HRA/HCRW Approval and REC favourable opinion in place www.icnarc.org Oversight by: o Trial Management Group o Independent Trial Steering Committee o Independent Data Monitoring and Ethics Committee Interim analysis at 830, 1340 and 1850 patients Site Initiation Visit 16
Local governance Site research team led by Principal Investigator (PI) o NIHR Associate PI scheme www.icnarc.org Provided electronically: Local Information Pack (LIP) Investigator Site File (ISF) Site Initiation Visit 17
Local governance Transfusion team involvement o Understanding of trial design and platelet administration according to randomised threshold o Team to be aware of patients randomised to T4P Can be added to receive automated randomisation notification emails Clinical team to send patient details and randomised threshold at randomisation www.icnarc.org o Some teams are able to: Place alert on transfusion system for T4P patients and their allocated threshold Transfusion team will query non-adherence to randomised threshold To act as a polite reminder Transfusion team involvement at your site? Site Initiation Visit 18
Agenda Background and trial design Governance Patient flow Support/resources www.icnarc.org Site Initiation Visit 19
Patient flow www.icnarc.org Screening Randomisation Safety monitoring Platelet transfusion threshold: Data collection <10x109/L <20x109/L <30x109/L <40x109/L <50x109/L Consent Follow-up Site Initiation Visit 20
Patient flow www.icnarc.org Screening Randomisation Safety monitoring Platelet transfusion threshold: Data collection <10x109/L <20x109/L <30x109/L <40x109/L <50x109/L Consent Follow-up Site Initiation Visit 21
Eligibility Inclusion criteria 1. Adult (aged 18 years) 2. Accepted for admission or admitted to a participating critical care unit 3. Platelet count <50x109/L 4. Planned to undergo a specified* low bleeding risk invasive procedure OR platelet transfusion being considered for an other procedure www.icnarc.org *Specified low bleeding risk invasive procedures include: o Central venous vascular catheter insertion (including vascular access for renal replacement therapy) o Paracentesis/superficial abdominal fluid collection drainage o Pleural aspiration Site Initiation Visit 22
Eligibility Other procedures may be included if the clinician deems these to be a low bleeding risk invasive procedure and a platelet transfusion is being considered for the procedure Arterial catheter insertion Arterial or central venous catheter removal Pleural drain Interventional Radiology Bronchoscopy with or without lavage Wound dressing changes Surgical procedures where the clinical team agree risk of bleeding is low, e.g. re-look laparotomy or wound closure Percutaneous tracheostomy www.icnarc.org Other list is not exhaustive Site Initiation Visit 23
Eligibility inclusion criterion 4 Planned to undergo a specified* low bleeding risk invasive procedure o The patient is planned for a specified low bleeding risk invasive procedure OR platelet transfusion being considered for an other procedure o The patient is planned for an invasive procedure imminently, that is considered low bleeding risk and a platelet transfusion is being considered for this procedure In both cases, you are randomising the patient for this procedure, and they must be randomised prior to the procedure www.icnarc.org Site Initiation Visit 24
Eligibility Exclusion criteria 1. Ongoing major haemorrhage requiring blood products and/or surgical/radiological intervention www.icnarc.org 2. Intracranial haemorrhage within prior 72 hours 3. Contra-indication to platelet transfusion (such as thrombotic microangiopathies; heparin-induced thrombocytopaenia; immune thrombocytopaenia; congenital platelet function defects) 4. Acute promyelocytic leukaemia (APML) 5. Known advance decision refusing blood/blood component transfusions (e.g. Jehovah s Witnesses) 6. Death perceived as imminent or admission for palliation. 7. Previously randomised into T4P 8. Fulfilled all the inclusion criteria and none of the other exclusion criteria 72 hours Criteria 1 & 2 are dynamic, and if resolved, the patient may be reconsidered for the trial Site Initiation Visit 25
Eligibility Fulfilled all the inclusion criteria and none of the other exclusion criteria 72 hours what does this mean? www.icnarc.org o Scenario 1 eligible on admission Meet eligibility 48 hours Admission 24 hours 72 hours 96 hours 120 hours 144 hours o Scenario 2 eligible during admission Meet eligibility 96 hours Admission 0 hours 48 hours 72 hours 24 hours Site Initiation Visit 26
See Study Manual Screening Screening begins at the point of the decision to admit to a critical care unit Screen all patients daily until; o Recruitment, i.e. they meet all inclusion and no exclusion criteria o Refusal o Critical care unit discharge Coverage for out-of-hours randomisations o Clinical staff training and engagement Training log to be completed for clinical staff undertaking screening and randomisation www.icnarc.org Thoughts on training and engagement of clinical staff for out-of-hours randomisations? Site Initiation Visit 27
See Study Manual Who can confirm eligibility A doctor, nurse, or clinical practitioner, as long as they are appropriately qualified, and have undergone study training as documented on the training log. Must still be overall oversight by a medically qualified doctor. o i.e., if the person confirming eligibility is not a doctor, they must receive agreement from the doctor responsible for the patient s care that the patient is suitable to be entered into the trial. Document this in the medical notes. The doctor responsible for the patient s care does not necessarily need to be trial trained. Note: If the doctor, nurse or clinical practitioner, is performing the eligibility/randomisation tasks ONLY, then they do not need to go on the delegation log. They can complete the training log once they have received trial training. www.icnarc.org Site Initiation Visit 28
See Study Manual & CRF Guidance Screening Log Entered onto T4P_SCREEN page on MACRO Record all patients with platelet count <50x109/L who are accepted/admitted to your critical care unit Each row represents a patient admission www.icnarc.org Site Initiation Visit 29
See Study Manual Enrolment Log Tab 1: Enrolment Log o Every randomised patient should be recorded on this log o Helps you keep track of actions required for each patient www.icnarc.org Tab 2: Screened Patients o Can be used as a key to identify your screened patients Please do not send this log as it contains patient identifiable information Site Initiation Visit 30
See Study Manual Screening tool (optional) Screening tool provided to help screen all patients admitted to critical care o Can use this to monitor those patients that are not initially eligible at admission to critical care, but later become eligible o This tool is purely for local use this does not need to be sent to ICNARC www.icnarc.org Site Initiation Visit 31
Co-enrolment Observational studies (including those collecting samples) o Permitted without prior agreement www.icnarc.org Interventional studies o Decided on a trial-by-trial basis o Co-enrolments with other ICNARC studies follow up will be combined where possible to reduce patient burden o Agreements in place with: MOSAICC PRONTO SHORTER SWiFT TARGET-UP Tight-K UK-ROX VAPX VITAL VitDALIZE FLO-ELA GenOMICC iRehab ISO-DRIVE MARCH A2B ABC ADAPT-SEPSIS BipPak2 EMERALD Site Initiation Visit 32
Patient flow www.icnarc.org Screening Randomisation Safety monitoring Platelet transfusion threshold: Data collection <10x109/L <20x109/L <30x109/L <40x109/L <50x109/L Consent Follow-up Site Initiation Visit 33
Patient flow www.icnarc.org Screening Randomisation Safety monitoring Platelet transfusion threshold: Data collection <10x109/L <20x109/L <30x109/L <40x109/L <50x109/L Consent Follow-up Site Initiation Visit 34
See Study See SOP 004 Manual Randomisation Dedicated 24/7 randomisation service o Sealed Envelope o Web randomisation Email T4P@icnarc.org to request an account Can use generic/group or individual email addresses www.icnarc.org Trial training required to randomise (documented on training log) o Appropriate clinical staff may be involved solely in the screening and randomisation of patients e.g. out-of-hours staff o GCP training not required to randomise Site Initiation Visit 35
See Study See SOP 004 Manual www.icnarc.org QR code to randomise on mobile device Details required by randomisation service Confirmation of inclusion/exclusion criteria Complete after confirmation of randomisation The person who confirmed eligibility (trial trained doctor, nurse or clinical practitioner) The doctor with medical oversight (doctor responsible for the patients care, does not need to be trial trained) The person who randomised the patient (anyone trial trained) Site Initiation Visit 36
See Study See SOP 004 Manual Randomisation Auto-generated randomisation notification emails o Email T4P@icnarc.org to add recipients www.icnarc.org Errors o Once randomised, patient is in trial and included in analysis consent and data collection must be carried out per protocol o If patient accidentally randomised twice use first randomisation Check email notification if unsure of the status of a randomisation (or contact local team/ICNARC CTU) Do not re-use the second randomisation details Site Initiation Visit 37
Patient flow www.icnarc.org Screening Randomisation Safety monitoring Platelet transfusion threshold: Data collection <10x109/L <20x109/L <30x109/L <40x109/L <50x109/L Consent Follow-up Site Initiation Visit 38
Patient flow www.icnarc.org Screening Randomisation Safety monitoring Platelet transfusion threshold: Data collection <10x109/L <20x109/L <30x109/L <40x109/L <50x109/L Consent Follow-up Site Initiation Visit 39
See Study See SOP 005 Manual Intervention Patients randomised to one of five equally-spaced platelet thresholds www.icnarc.org <10x109/L <20x109/L <30x109/L <40x109/L <50x109/L below which they would receive a single adult equivalent dose (AED) of platelet transfusion delivered before or during a procedure The randomised threshold is the intervention Site Initiation Visit 40
See Study Manual Intervention Example scenarios: www.icnarc.org Platelet count: 38x109/L Platelet count: 38x109/L Randomised threshold: <20x109/L Randomised threshold: <40x109/L Administer platelets prophylactically before/during a low bleeding risk invasive procedure Do not administer platelets prophylactically before/during a low bleeding risk invasive procedure Site Initiation Visit 41
See Study See SOP 005 Manual Intervention Treatment according to the randomly allocated platelet threshold begins immediately following randomisation o Applies immediately to first procedure (i.e. the procedure that deemed the patient eligible to be randomised) and continues until critical care unit discharge o Applies to all subsequent invasive procedures deemed low bleeding risk o Decision of whether a procedure is deemed low/high bleeding risk should be documented in medical notes If re-admitted to critical care unit during the index hospital stay within 90 days, treatment according to the randomly allocated threshold should be recommenced www.icnarc.org Site Initiation Visit 42
See Study See SOP 005 Manual Intervention Use most recent platelet count to inform intervention o These may change during course of critical care unit admission o Platelet counts may move across the allocated threshold for subsequent procedures, changing whether platelets are given/not given prophylactically www.icnarc.org Site Initiation Visit 43
See Study See SOP 005 Manual Intervention Co-interventions o Where a patient is receiving a low bleeding risk invasive procedure, platelet prophylaxis is only permitted according to allocated randomised threshold o However, platelet administration should follow local guidance: For high bleeding risk interventional procedures Where significant bleeding occurs during or after a low bleeding risk invasive procedure Platelets given outside of any procedure www.icnarc.org Site Initiation Visit 44
See Study See SOP 005 Manual Adherence to the intervention Non-adherence to the intervention will be defined as: o Receipt of platelet transfusion for low bleeding risk invasive procedure when platelet count is above randomised allocated threshold o Platelet transfusion not received for low bleeding risk invasive procedure when platelet count is below randomised allocated threshold www.icnarc.org Reasons for non-adherence should be documented locally Platelet administration deviation CRF to be completed Site Initiation Visit 45
See Study See SOP 005 Manual Training Ensure staff are aware of trial o They may be managing patients randomised to T4P o Awareness of randomised threshold and procedure inclusion o Discussion point at ward rounds o Bedside notices/posters/stickers provided by ICNARC CTU www.icnarc.org Site Initiation Visit 46
FAQs Use of TEG (thromboelastography) o Some units may routinely use TEG/ROTEM measurements to guide transfusion in stable critically ill patients, although this is not evidence based o For the trial use the most recent platelet count and adhere to the platelet threshold allocated on randomisation o If TEG has been used to guide platelet transfusion when platelet count is above the allocated threshold, then this will be a protocol deviation www.icnarc.org Site Initiation Visit 47
Patient flow www.icnarc.org Screening Randomisation Safety monitoring Platelet transfusion threshold: Data collection <10x109/L <20x109/L <30x109/L <40x109/L <50x109/L Consent Follow-up Site Initiation Visit 48
Patient flow www.icnarc.org Screening Randomisation Safety monitoring Platelet transfusion threshold: Data collection <10x109/L <20x109/L <30x109/L <40x109/L <50x109/L Consent Follow-up Site Initiation Visit 49
See Consent Guide Research Without Prior Consent Patients likely to lack capacity at time of randomisation Emergency waiver of consent granted by REC (Mental Capacity Act) www.icnarc.org After randomisation - once patient s medical situation is considered no longer an emergency, the consent procedures should begin o Consent sought after randomisation by GCP-trained delegated team member o Expected to be within 24-48 hours of randomisation Posters and leaflets available Recommended: NIHR Informed Consent with Adults Lacking Capacity course Site Initiation Visit 50