Predicting Renal Recurrence in IgA Vasculitis Nephritis
Preliminary results and analysis of histologic and immunologic markers to predict renal recurrence in IgA vasculitis nephritis, with comparison of patient groups based on clinical course.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Histologic and immunologic markers to predict renal recurrence in IgA vasculitis nephritis Preliminary results K Abukasm, AL Lapeyraque, H Mathieu, N Patey, A Cambier Karma Abukasm Pediatric Nephrology Fellow CHU Sainte-Justine April 25th, 2023
Introduction (1) IgA vasculitis (formerly Henoch-Schonlein Purpura, IgAV) is the most common vasculitis in children (incidence rate of 3 to 26.7 cases/100 000 children1) Diagnosis based on EULAR/PRINTO/PRES criteria2 Renal involvement estimated in 30-50% of cases at 4-6 weeks following the initial presentation3 Chronic/end-stage kidney disease estimated in about 1-7% of cases Suggested poor outcome predictors of IgAV nephritis (IgAVN) 4: older age, renal function impairment, nephrotic syndrome or mixed nephrotic/nephritic syndrome at presentation, presence of glomerular crescents 1 Piram et Maher, 2013 ; 2 Ozen et al., 2010 ; 3 Narchi, 2005; 4 Shi et al., 2019
Introduction (2) Immunologic and pathologic similarities between IgAVN and IgA nephropathy (IgAN) 5,6,7,8 : Galactose deficient IgA1 (Gd-IgA1) IgG targeting Gd-IgA (anti-Gd-IgA1) Serum soluble CD89-IgA complex (sCD89-IgA) C5b9 membrane attack complex (MAC) Uncertain role of renal biopsy in the prognostic evaluation of patients with IgAVN (compared to IgAN) 9 5 Suzuki et al., 2009; 6 Vuong et al., 2010 ; 7 Dumont et al., 2020 ; 8 Cambier et al., 2022 ; 9 Tudorache et al., 2015
Main objectives 1. Compare clinical, biochemical and histological characteristics of three groups of patients with IgAVN classified based on their clinical course; 2. Analyze and compare intrarenal immunological deposits (IgA, C3, C4d, CD89 et MAC) in histology samples in all three groups ; 3. Compare circulating immune complex levels (sCD89-IgA, Gd-IgA, IgG- IgA, sCD89) in plasma and renal biopsies in all three groups. Renal relapsing disease (IgAN type) Renal and purpuric relapsing disease Monophasic disease
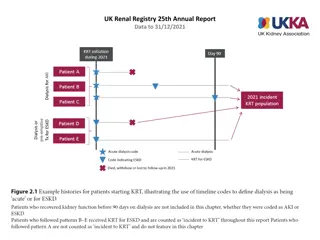
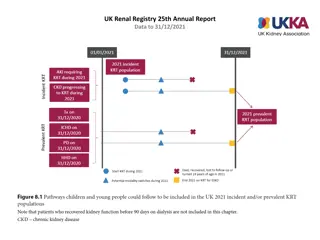
Methods Retrospective cohort study in pediatric patients diagnosed with IgAVN and followed-up in CHU Sainte-Justine nephrology clinic between July 2014 and February 2023 Minimally one kidney biopsy Incomplete files excluded Data collection through record review Biopsy samples reviewed with nephropathologist in order to complete missing data (Oxford scoring) and immunofluorescence staining Statistical analysis completed with SPSS (p value < 0.05 considered statistically significant) Nominal data : Fisher s Exact Test Continuous data : One-way ANOVA
Results Table 1. Initial presentation of IgAV classified based on IgAVN clinical evolution Renal relapsing disease (IgAN type) 5/7 (71.4) Renal and purpuric relapsing disease 4/5 (80.0) p-value Monophasic disease Female sex, n (%) Age at IgAV diagnosis, mean (median) Involvement at initial presentation Digestive, n (%) Articular, n (%) Renal, n (%) Need for hospitalization at initial presentation, n (%) Treatment received at initial presentation, n (%) Corticosteroids, n (%) NSAID, n (%) IVIg, n (%) ACE inhibitors, n (%) MMF, n (%) ACE : Angiotensin-converting-enzyme ; IVIg : Intravenous immunoglobulin ; MMF : Mycophenolate Mofetil ; NSAID : Non-steroidal anti-inflammatory drugs Fisher s Exact Test 9/24 (37.5) 0.158 10.2 (8.1) 9.3 (12.0) 8.5 (9.2) 0.987 12/23 (52.2) 20/23 (87.0) 6/23 (26.1) 6/7 (85.7) 4/7 (57.1) 3/7 (42.9) 3/5 (60.0) 2/5 (40.0) 0/5 0.342 0.360 0.372 9/22 (40.9) 3/7 (42.9) 0/4 0.364 12/17 (70.6) 3/6 (50.0) 1/2 (50.0) 0.528 9/13 (69.2) 10/12 (83.3) 1/12 (8.3) 0/12 1/12 (8.3) 3/3 (100.0) 1/3 (33.3) 0/3 1/3 (33.3) 0/3 1/2 (50.0) 0/1 0/1 0/1 0/1 NA NA NA NA NA
Table 2. Clinical and biochemical presentation at first nephrology visit for IgAVN classified based on IgAVN clinical evolution Renal relapsing disease (IgAN type) Renal and purpuric relapsing disease p-value Monophasic disease Time from initial IgAV presentation in days, mean (median) Motive for referral Isolated proteinuria, n (%) Proteinuria and hematuria, n (%) Gross hematuria, n (%) Microscopic hematuria, n (%) Nephrotic syndrome, n (%) Nephritic syndrome, n (%) Acute kidney injury, n (%) Hematuria at time of visit None, n (%) Gross, n (%) Microscopic, n (%) Presence of proteinuria on urinalysis, n (%) Nephrotic proteinuria on urinary spot (> 0.2 g/mmol) Proteinuria on 24-hour urine collection (g/day), mean (median) Hypertension present at initial nephrology visit, n (%) Bloodwork results Urea, mean (median) Creatinine, mean (median) Albumin, mean (median) Serum IgA, mean (median) Fisher s Exact Test 50.5 (22) 483.5 (34) 143.5 (139) 0.160 9/24 (23.7) 10/24 (26.3) 4/24 (10.5) 0/24 0/24 1/24 (2.6) 0/24 0/7 2/5 (40.0) 3/5 (60.0) 0/5 0/5 0/5 0/5 0/5 6/7 (85.7) 0/7 1/7 (14.3) 0/7 0/7 0/7 1.000 3/24 (12.5) 5/24 (20.8) 15/24 (62.5) 23/23 (100.0) 13/19 (68.4) 0/7 0/5 2/7 (28.6) 5/7 (71.4) 6/7 (85.7) 1/6 (16.7) 1/5 (20.0) 4/5 (80.0) 4/4 (100.0) 3/5 (60.0) 0.324 0.178 1.6 (1.3) 1.4 (0.87) 1.6 (1.6) 4/24 (16.7) 1/7 (14.3) 0/4 0.307 4.7 (4.5) 53.5 (50.5) 33.2 (33) 2.6 (2.5) 3.9 (3.8) 54.9 (55) 34 (35) 3.5 (3.6) 4.1 (4.5) 51 (46) 37.3 (37.5) 2.95 (2.95) 0.226 0.917 0.460 0.470
Table 3. Clinical and biochemical presentation at first renal biopsy classified based on IgAVN clinical evolution Renal relapsing disease (IgAN type) 2.5 3/7 (42.9) 3/7 (42.9) 0/7 1/7 (14.3) Renal and purpuric relapsing disease 2.7 1/5 (20.0) 2/5 (40.0) 2/5 (40.0) 0/5 p-value Monophasic disease Number of biopsies performed, mean 1, n (%) 2, n (%) 3, n (%) 4, n (%) Reason for renal biopsy Gross hematuria, n (%) Persistent proteinuria, n (%) Nephrotic syndrome, n (%) Nephritic syndrome, n (%) Nephrotic proteinuria recurrence, n (%) Acute kidney injury, n (%) Age at first kidney biopsy, mean (median) Time from initial IgAV presentation in days, mean (median) Presence of proteinuria on urinalysis, n (%) Nephrotic proteinuria on urinary spot (> 0.2 g/mmol) Presence of hematuria, n (%) Bloodwork results Urea, mean (median) Creatinine, mean (median) Albumin, mean (median) Serum IgA, mean (median) Fisher s Exact Test 2.12 0.070 20/24 (83.3) 3/24 (12.5) 1/24 (4.2) 0/24 0.645 2/24 (8.3) 18/24 (75.0) 1/24 (4.2) 2/24 (8.3) 0/24 1/24 (4.2) 10.4 (8.3) 1/7 (14.3) 4/7 (57.1) 1/7 (14.3) 0/7 1/7 (14.3) 0/7 10.9 (13.5) 0/5 5/5 (100.0) 0/5 0/5 0/5 0/5 9.0 (9.4) 80.0 (62.0) 658.7 (150.0) 192.2 (139.0) 0.713 23/23 (100.0) 12/18 (66.7) 22/23 (95.7) 6/6 (100.0) 3/7 (42.9) 6/6 (100.0) 5/5 (100.0) 2/5 (40.0) 5/5 (100.0) 1.000 0.156 1.000 4.8 (4.6) 54.8 (51.5) 31.5 (33.0) 2.4 (2.4) 3.8 (4.1) 52.7 (56) 33.7 (34) 2.27 (2.27) 4.4 (4.5) 50.4 (46) 37 (39) 2.95 (2.95) 0.306 0.810 0.121 NA
Table 4. MEST-C score (Oxford score) on initial renal biopsy classified based on IgAVN clinical evolution Renal relapsing disease (IgAN type) 1 3/7 (42.9) 4/7 (57.1) 0 5/7 (71.4) 2/7 (28.6) 0 4/7 (57.1) 3/7 (42.9) 0 6/7 (85.7) 1/7 (14.3) 0/7 1 3/7 (42.9) 4/7 (57.1) 0/7 Renal and purpuric relapsing disease 1 2/4 (50.0) 2/4 (50.0) 1 1/4 (25.0) 3/4 (75.0) 1 2/4 (50.0) 2/4 (50.0) 0 3/4 (75.0) 1/4 (25.0) 0/4 1 0/4 4/4 (100.0) 0/4 p-value Monophasic disease M, mode 1 0.808 M0, n (%) M1, n (%) 9/24 (37.5) 15/24 (62.5) 1 7/24 (29.2) 15/24 (62.5) 0 15/24 (62.5) 9/24 (37.5) 0 22/24 (91.7) 1/24 (4.2) 1/24 (4.2) 0 10/23 (43.5) 8/23 (34.8) 5/23 (21.7) E, mode 0.322 E0, n (%) E1, n (%) S, mode 1.000 S0, n (%) S1, n (%) T, mode 0.478 T0, n (%) T1, n (%) T2, n (%) C, mode 0.164 C0, n (%) C1, n (%) C2, n (%) M : Mesangial score (M0, M1) ; E : endocapillary hypercellularity (E0, E1) ; S : segmental glomerulosclerosis (S0, S1) ; T : tubular atrophy (T0, T1, T2) ; C : cellular/fibrocellular crescents
Table 5. Immunofluorescence staining on initial renal biopsy classified based on IgAVN clinical evolution Renal relapsing disease (IgAN type) Renal and purpuric relapsing disease p-value Monophasic disease IgA 1.000 Negative, n (%) (+/-) , n (%) Positive, n (%) 0/21 0/7 0/7 0/5 0/5 1/21 (4.8) 20/21 (95.2) 7/7 (100.0) 5/5 (100.0) C3 0.804 Negative, n (%) (+/-) , n (%) Positive, n (%) 5/20 (25.0) 2/20 (10.0) 13/20 (65.0) 1/7 (14.3) 1/7 (14.3) 5/7 (71.5) 0/5 0/5 5/5 (100.0) MAC 0.642 Negative, n (%) (+/-) , n (%) Positive, n (%) Presence of necrosis, n (%) MAC : Macrophage activation complex 9/24 (37.5) 5/24 (20.8) 10/24 (41.7) 2/7 (28.6) 1/7 (14.3) 4/7 (57.1) 2/3 (66.7) 1/3 (33.3) 0/3 3/22 (13.6) 1/7 (14.3) 1/5 (20.0)
Table 6. Treatment throughout follow-up for IgAVN classified based on IgAVN clinical evolution Renal relapsing disease (IgAN type) 6/7 (85.7) Renal and purpuric relapsing disease 5/5 (100.0) Monophasic disease p-value Treatment received, n (%) Treatment choice High dose corticosteroids (pulses), n (%) Oral corticosteroids, n (%) ACE inhibitor, n (%) MMF, n (%) Hydroxychloroquine, n (%) Cyclophosphamide, n (%) Other**, n (%) 21/24 (87.5) 1.000 12/21 (57.1) 18/21 (85.7) 16/21 (76.2) 0/21 2/21 (9.5) 2/21 (9.5) 2/21 (9.5) 6/6 (100.0) 6/6 (100.0) 6/6 (100.0) 2/6 (33.3) 3/6 (50.0) 0/7 1/7 (14.3) 2/5 (40.0) 4/5 (80.0) 5/5 (100.0) 0/5 1/5 (20.0) 0/5 2/5 (40.0) 0.069 0.778 0.475 0.050* 0.068 1.000 ACE : Angiotensin-converting-enzyme ; MMF : Mycophenolate Mofetil **Other : Furosemide (1), amlodipine (1) Non renal indication : colchicine (2), IVIg (2), rituximab (1)
Conclusion Inital presentation of IgAV Female sex predominance in both renal (IgAN type) and renal/purpuric recurrent disease type More articular involvement in monophasic disease ; more digestive involvement in renal recurrent disease (IgAN type) More treatment at initial presentation in monophasic disease Renal presentation More nephrotic proteinuria and lower serum albumin levels in monophasic disease Serum IgA levels elevated in most patients (19/25 ; 76%) Renal biopsy and pathology More renal biopsies performed in patients with recurrent disease No difference on immunofluorescence staining and MEST-C scores between the three groups Treatment Most patients treated throughout disease course More aggressive treatment in renal recurrent disease (IgAN type) more corticosteroid pulses (p = 0.069), hydroxychloroquine (p = 0.068) and MMF (p = 0.050)
Anticipated next steps Extended intrarenal immune deposits analysis (C4d, CD89) and comparison of IgAVN findings to IgAN patients Analysis of circulating immune complex levels (sCD89-IgA, Gd-IgA, IgG-IgA, sCD89), which are likely involved in physiopathological processes of IgAVN (mirroring IgAN literature) Integration of clinical and immunopathological findings to inform decision making in regards to evolution and prognosis of IgAVN
Merci! karma.abukasm@umontreal.ca
References Piram M, Mahr A. Epidemiology of immunoglobulin A vasculitis (Henoch-Sch nlein): current state of knowledge. Curr Opin Rheumatol. 2013;25(2):171-8. Ozen S, Pistorio A, Iusan SM, Bakkaloglu A, Herlin T, Brik R, et al. EULAR/PRINTO/PRES criteria for Henoch- Schonlein purpura, childhood polyarteritis nodosa, childhood Wegener granulomatosis and childhood Takayasu arteritis: Ankara 2008. Part II: Final classification criteria. Annals of the Rheumatic Diseases. 2010;69(5):798-806. Narchi H. Risk of long term renal impairment and duration of follow up recommended for Henoch-Schonlein purpura with normal or minimal urinary findings: a systematic review. Arch Dis Child. 2005;90(9):916-20. Shi D, Chan H, Yang X, Zhang G, Yang H, Wang M, et al. Risk factors associated with IgA vasculitis with nephritis (Henoch-Sch nlein purpura nephritis) progressing to unfavorable outcomes: A meta-analysis. PLoS One. 2019;14(10):e0223218. Suzuki H, Fan R, Zhang Z, Brown R, Hall S, Julian BA, et al. Aberrantly glycosylated IgA1 in IgA nephropathy patients is recognized by IgG antibodies with restricted heterogeneity. Journal of Clinical Investigation. 2009. Vuong MT, Hahn-Zoric M, Lundberg S, Gunnarsson I, Van Kooten C, Wramner L, et al. Association of soluble CD89 levels with disease progression but not susceptibility in IgA nephropathy. Kidney International. 2010;78(12):1281-7. Dumont C, M rouani A, Ducruet T, Benoit G, Clermont MJ, Lapeyraque AL, et al. Clinical relevance of membrane attack complex deposition in children with IgA nephropathy and Henoch-Sch nlein purpura. Pediatr Nephrol. 2020;35(5):843-50. Cambier A, Gleeson PJ, Abbad L, Canesi F, da Silva J, Bex-Coudrat J, et al. Soluble CD89 is a critical factor for mesangial proliferation in childhood IgA nephropathy. Kidney Int. 2022;101(2):274-87. Tudorache E, Azema C, Hogan J, Wannous H, Aoun B, Decramer S, et al. Even mild cases of paediatric Henoch- Sch nlein purpura nephritis show significant long-term proteinuria. Acta Paediatrica. 2015;104(8):843-8.