Prevalence and Distribution of HPV Types in Female Sex Workers in Kenya
This study examines the prevalence, incidence, and genotype distribution of human papillomavirus (HPV) infections in female sex workers in Nairobi, Kenya. It compares the burden of HPV between HIV-positive and HIV-negative women, providing insights into the impact of HPV in this high-risk population.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
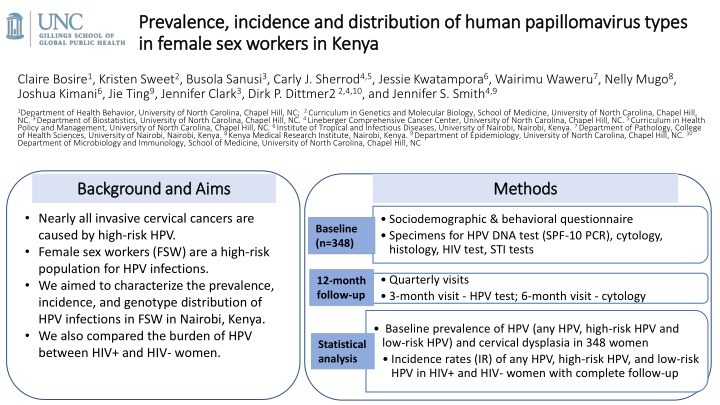
Prevalence, incidence and distribution of human papillomavirus types Prevalence, incidence and distribution of human papillomavirus types in female sex workers in Kenya in female sex workers in Kenya Claire Bosire1, Kristen Sweet2, Busola Sanusi3, Carly J. Sherrod4,5, Jessie Kwatampora6, Wairimu Waweru7, Nelly Mugo8, Joshua Kimani6, Jie Ting9, Jennifer Clark3, Dirk P. Dittmer22,4,10, and Jennifer S. Smith4,9 1Department of Health Behavior, University of North Carolina, Chapel Hill, NC; 2 Curriculum in Genetics and Molecular Biology, School of Medicine, University of North Carolina, Chapel Hill, NC. 3 Department of Biostatistics, University of North Carolina, Chapel Hill, NC. 4 Lineberger Comprehensive Cancer Center, University of North Carolina, Chapel Hill, NC. 5 Curriculum in Health Policy and Management, University of North Carolina, Chapel Hill, NC. 6 Institute of Tropical and Infectious Diseases, University of Nairobi, Nairobi, Kenya. 7 Department of Pathology, College of Health Sciences, University of Nairobi, Nairobi, Kenya. 8 Kenya Medical Research Institute, Nairobi, Kenya. 9 Department of Epidemiology, University of North Carolina, Chapel Hill, NC. 10 Department of Microbiology and Immunology, School of Medicine, University of North Carolina, Chapel Hill, NC Background and Aims Background and Aims Methods Methods Nearly all invasive cervical cancers are caused by high-risk HPV. Female sex workers (FSW) are a high-risk population for HPV infections. We aimed to characterize the prevalence, incidence, and genotype distribution of HPV infections in FSW in Nairobi, Kenya. We also compared the burden of HPV between HIV+ and HIV- women. Sociodemographic & behavioral questionnaire Specimens for HPV DNA test (SPF-10 PCR), cytology, histology, HIV test, STI tests Baseline (n=348) Quarterly visits 3-month visit - HPV test; 6-month visit - cytology 12-month follow-up Baseline prevalence of HPV (any HPV, high-risk HPV and low-risk HPV) and cervical dysplasia in 348 women Incidence rates (IR) of any HPV, high-risk HPV, and low-risk HPV in HIV+ and HIV- women with complete follow-up Statistical analysis
Quarter of participants were HIV + Prevalence of HPV infections was higher in HIV positive than in HIV negative women Prevalence of advanced lesions (HSIL/SCC) was higher in HIV positive compared to HIV negative women. Prevalence of histologic-confirmed CIN2+ was higher among HIV positive compared to HIV negative women Results: Baseline HPV and cervical dysplasia prevalence Baseline prevalence of HPV DNA infection and cervical dysplasia, stratified by HIV status in 348 female sex workers in Nairobi, Kenya Total n (%) HIV + HIV - Characteristic p-value Baseline distribution of HPV types in a cohort of 348 female sex workers in Nairobi, Kenya (n=348) (n=84) (n=264) Age (median, 0.40 28 (18-48) 32 (21-48) 27 (18-46) 0.05 range) 0.35 Any HPV 82 (23.6) 27 (32.1) 55 (20.8) 0.03 Proportion 0.30 HR HPV 71 (20.4) 23 (27.4) 48 (18.2) 0.56 0.25 LR HPV 11 (3.2) 4 (4.8) 7 (2.7) 0.31 0.20 Cytology 0.15 Normal 282 (81.0) 53 (63.1) 229 (86.7) <0.01 0.10 ASCUS/AGUS 14 (4.0) 4 (4.8) 10 (3.8) 0.75 0.05 LSIL 37 (10.6) 16 (19.1) 21 (8.0) <0.01 0.00 HSIL/SCC 15 (4.3) 11 (13.1) 4 (1.5) <0.01 6 68/73 11 33 58 45 18 16 31 52 44 54 70 66 74 39 56 53 35 51 Histology HPV type Negative 329 (94.5) 70 (83.3) 259 (98.1) <0.01 HIV- HIV+ HPV types in nonavalent vaccine 2 CIN 2+ 19 (5.5) 14 (16.7) 5 (1.9) <0.01
Results: Incident HPV infections Majority of incident infections were high- risk HPV Incidence rates of any HPV, high-risk HPV and low-risk HPV in 160 female sex workers in Nairobi, Kenya 50 IR any HPV: 31.4 (95% CI: 23.8-41.5) 45 Incidence Rate (per 1000 p-months) IR high-risk HPV: 24.2 (95% CI: 17.9-32.8) 40 Stratified by HIV status, IR any HPV higher in HIV positive women (IR: 46.7 95% CI: 28.2-77.5) than HIV negative women 35 30 25 (IR: 27.6 95% CI: 19.8-38.4) 20 15 High-risk HPV IR was higher in HIV positive (IR: 29.3 95% CI: 16.2-52.9) than in HIV negative women (IR: 22.8 95% CI:16.0-32.4). 10 5 0 hr HP V lr HP V HPV 52 was most common incident infection overall. An y 68 /73 16 18 31 33 35 39 45 51 52 56 58 66 6 11 44 53 54 70 74 HIV positive 47 29 7.2 1.8 5.6 0 3.7 0 0 1.8 8 0 0 1.8 0 20 0 5.3 1.7 1.7 7.7 0 0 HIV negative 28 23 2.1 0 3.8 1.1 1.6 0.5 2.7 3.9 5.4 1.1 1.1 1.1 0 11 2.1 0.5 0.5 0.5 5.7 0.5 1.1 HPV types 3
Conclusion Acknowledgement Higher prevalence and incidence of HPV and associated cervical disease observed in HIV- positive women compared to HIV-negative women highlights the need to prioritize strategies, including vaccination, screening, and treatment of precancerous lesions. This study was supported by PHS grants to the University of North Carolina Center for AIDS Research (CfAR) (# P30- AI50410060); UNC Lineberger Comprehensive Cancer Center (P30-CA016086 and P01-CA019014); Howard Hughes Medical Institute Translational medicine training grant and T32-GM007092 (K. Sweet); Cancer Health Disparities training grant # T32-CA128582-10 (C.Bosire) For more information, please contact: Claire Bosire ScD, MSPH, RD Postdoctoral Fellow, Cancer Health Disparities Program Gillings School of Global Public Health, University of North Carolina at Chapel Hill Email: cbosire@email.unc.edu 4