Preventing Lower Respiratory Tract Infections
Lower respiratory tract infections are a common health concern, but with proper preventive measures, they can be minimized. This article discusses various strategies and practices to reduce the risk of lower respiratory tract infections, including hygiene tips, vaccination recommendations, and lifestyle adjustments. By implementing these preventive measures, individuals can protect themselves and others from these infections and promote overall respiratory health.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Prevention of Lower Respiratory Tract Infections
Learning objectives December 1, 2013 1. Explain the relevance of pneumonia in health care institutions. 2. Outline elements for defining HAI pneumonia. 3. Identify risk factors for pneumonia. 4. Describe the measures for prevention of pneumonia. 2
Time involved December 1, 2013 35-40 minutes 3
Key points December 1, 2013 Pneumonia causes morbidity and mortality and increased utilisation of resources Prevention is vital Prevention includes hand hygiene use of gloves daily assessment of weaning from a ventilator elevation of the bed head orotracheal intubation oral care with an antiseptic solution cleaning and disinfection of equipment 4
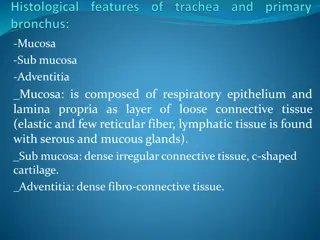
Introduction In healthy individuals the lower respiratory tract is sterile Cough reflex, respiratory mucosa, secretions, and immunity prevent microorganisms in the LRT Impaired conditions of patients and incorrect practices contribute to healthcare-associated pneumonia December 1, 2013 5
The problem Pneumonia accounts for 11% - 15% of HAI and 25% of infections in ICUs Highest mortality among HAIs Postoperative pneumonia - a common complication of surgery Ventilator associated pneumonia occurs in 8- 28% of patients Prolongs hospitalisation and antibiotic use Microorganisms often multidrug-resistant December 1, 2013 6
Healthcare-associated Pneumonia December 1, 2013 DEFINITION LRT infection that appears during hospitalisation in a patient who was not incubating the infection at admission 7
Diagnosis December 1, 2013 It is diagnosed by the following: rales or bronchial breath sounds fever purulent sputum, cough, dyspnoea, tachypnea relevant radiologic changes preferably, microbiological diagnosis from bronchial lavage, transtracheal aspirate, or protected brush culture 8
Categories* December 1, 2013 There are three pneumonia categories: PNU1 X-ray changes and clinical signs and symptoms laboratory findings PNU2 X-ray changes, clinical signs and symptoms, microbiological results PNU3 pneumonia in immuncompromised 9
Surveillance December 1, 2013 For surveillance purposes, many practitioners use the pneumonia definition published by the U.S. Centers for Disease Control and Prevention s National Healthcare Safety Network (NHSN) 10
Mechanical ventilation Impairs normal removal of mucus and microorganisms from the lower airway H2 blocking agents associated with colonisation of gastrointestinal tract and oropharynx December 1, 2013 11
Pathogenesis December 1, 2013 Microorganisms may be introduced into the LRT via contaminated equipment or staff hands 12
Risk Factors Severely ill, e.g., septic shock Surgery (chest/abdomen) injuries Age Cardiopulmonary disease Cerebrovascular accidents Lung disease Coma Heavy smoker Sedation General anaesthesia Tracheal intubation Tracheostomy Enteral feeding Mechanical ventilation Broad spectrum antibiotic H2 blockers Immunosuppressive and cytotoxic drugs December 1, 2013 Condition of patient Therapy 13
Time of onset December 1, 2013 Early-onset pneumonia Four days of admission (in ICUs or after surgery) Late-onset pneumonia More than 4 days after admission 14
Etiological agents December 1, 2013 Early-onset pneumonia Late-onset pneumonia Streptococcus pneumoniae Pseudomonas aeruginosa Haemophilus influenzae Acinetobacter spp. Moraxella catarrhalis Methicillin- sensitive Staphylocoocus aureus Enterobacter spp. Methicillin- resistant Staphylococcus aureus Influenza Respiratory syncytial or other respiratory viruses Multidrug - resistant organisms Candida spp. Aspergillus spp. 15
Considerations Many late-onset VAPs caused by multi-resistant microorganisms In immunocompromised patients microbes: Viruses (RSV, influenza) Fungi (Candida spp. and Aspergillus) Legionella from air conditioning or water supplies Pneumocystis carinii (AIDS patients) Mycobacteria December 1, 2013 16
NHSN survey -causes of VAP in USA December 1, 2013 Other 25% S. Aureus 25% Candida 3% Pseudomonas 17% E coli 5% Klebsiella 8% 17 Acinetobacter 9% Enterobacter 8%
Survey in 12 European countries 2008* December 1, 2013 S. Aureus 16% Other 30% Pseudomonas 18% Candida 8% E coli 9% Enterobacter 7% Klebsiella 8% Acinetobacter 4% 18 *European Centre for Disease Prevention and Control (ECDC)
Prevention December 1, 2013 Recommendations are designed to avoid the three mechanisms by which pneumonia develops: aspiration contamination of the aerodigestive tract contaminated equipment 19
Prevention of postoperative pneumonia Treat lung disease prior to surgery Elevate head of the bed Avoid unnecessary suctioning Provide regular oral cavity care Encourage deep breathing and coughing Provide pain therapy (non-sedative) Use percussion and postural drainage to stimulate coughing Encourage early mobilisation December 1, 2013 20
Prevention of VAP -1 December 1, 2013 Hand hygiene before and after contact with patient or respiratory secretions Gloves when handling secretions Sterile gloves for aspiration and tracheostomy care Sterile suction catheter Daily assessments of readiness to wean. Minimise the duration of ventilation and noninvasive whenever possible 21
Prevention of VAP -2 Elevate the head of the bed Avoid gastric over-distension Avoid unplanned extubation Orotracheal intubation Avoid H2 agents and proton pump inhibitors Regular oral care with an antiseptic solution Sterile water to rinse respiratory equipment. Remove condensate, keep the circuit closed Change ventilator circuit only when necessary December 1, 2013 22
Prevention of VAP -3 Store and disinfect respiratory equipment Surveillance for VAP Direct observation of compliance Educate healthcare personnel Establish antibiotic regimens in accordance with the local situation December 1, 2013 23
References -1 1. Tablan OC, Anderson LJ, Besser R, Bridges C, Hajjeh R. Guidelines for preventing health-care associated pneumonia, 2003: recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. MMWR Recom Rep 2004; 53:1-36. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr53 03a1.htm 2. American Thoracic Society; Infectious Disease Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Amer J Respir Crit Care Med 2005; 171:388-416. http://ajrccm.atsjournals.org/ cgi/reprint/171/4/388 December 1, 2013 24
References -2 1. Coffin S, Klompas M, Classen D et al. Strategies to prevent ventilator- associated pneumonia in acute care hospitals. Infect Control Hosp Epidemiol 2008; 29:S31-S40. 2. Kollef M. Prevention of hospital-associated pneumonia and ventilator associated pneumonia. Crit Care Med 2004; 32:1396-1405. December 1, 2013 25
Further reading December 1, 2013 1. Allegranz B, Nejad SB, Combescure C, Graafmans W, Attar H, Donaldson L, Pittet P. Burden of endemic health-care-associated infection in developing countries: systematic review and meta- analysis. Lancet 2011; 377: 228 241. 2. Ding J-G, Qing-Feng S, Li K-C, Zheng M-H, et al. Retrospective analysis of nosocomial infections in the intensive care unit of a tertiary hospital in China during 2003 and 2007. BMC Infect Dis 2009; 9:115. 26
Quiz 1. Most cases of hospital pneumonia are not preventable. T/F? The main strategy to prevent VAP is a) Treatment of respiratory diseases b) Routine culture of patients c) Minimise duration of mechanical ventilation d) Isolation of infected patients in ICU Regarding prevention of VAP, which is incorrect? a) Change circuits of mechanical ventilation only if is necessary b) Elevate head of the bed if not contraindicated c) Gloves when handling respiratory secretions d) Use of antimicrobial prophylaxis always in patients with mechanical ventilation December 1, 2013 2. 3. 27
International Federation of Infection Control IFIC s mission is to facilitate international networking in order to improve the prevention and control of healthcare associated infections worldwide. It is an umbrella organisation of societies and associations of healthcare professionals in infection control and related fields across the globe . The goal of IFIC is to minimise the risk of infection within healthcare settings through development of a network of infection control organisations for communication, consensus building, education and sharing expertise. For more information go to http://theific.org/ December 1, 2013 28