Prompt Recognition and Management of CNS Infections
Meningitis, a neurologic emergency, requires timely diagnosis and treatment to prevent severe outcomes. Bacterial meningitis, caused by various pathogens, poses significant risks, necessitating rapid medical intervention. Risk factors include recent exposures, immunosuppression, surgery, trauma, and noninfectious causes. Understanding these factors is crucial for effective management and prevention of CNS infections.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
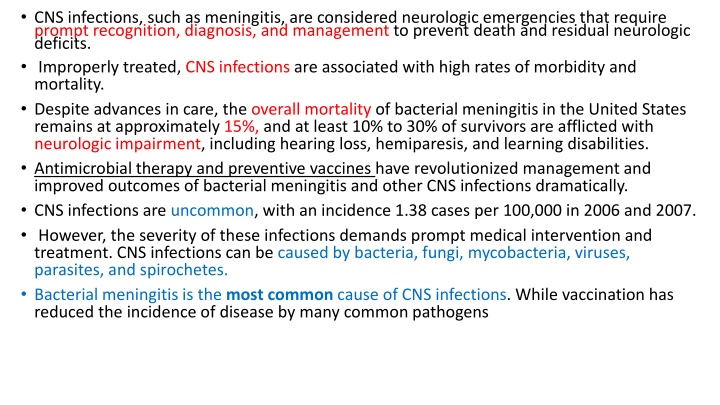
CNS infections, such as meningitis, are considered neurologic emergencies that require prompt recognition, diagnosis, and management to prevent death and residual neurologic deficits. Improperly treated, CNS infections are associated with high rates of morbidity and mortality. Despite advances in care, the overall mortality of bacterial meningitis in the United States remains at approximately 15%, and at least 10% to 30% of survivors are afflicted with neurologic impairment, including hearing loss, hemiparesis, and learning disabilities. Antimicrobial therapy and preventive vaccines have revolutionized management and improved outcomes of bacterial meningitis and other CNS infections dramatically. CNS infections are uncommon, with an incidence 1.38 cases per 100,000 in 2006 and 2007. However, the severity of these infections demands prompt medical intervention and treatment. CNS infections can be caused by bacteria, fungi, mycobacteria, viruses, parasites, and spirochetes. Bacterial meningitis is the most common cause of CNS infections. While vaccination has reduced the incidence of disease by many common pathogens
Streptococcus pneumoniae (pneumococcus) was the most common pathogen for bacterial meningitis (0.306 cases per 100,000), followed by Neisseria meningitidis (meningococcus, 0.123 cases per 100,000). Haemophilus influenza was a top causative pathogen; however, its incidence has declined to 0.058 cases per 100,000). Staphylococcal species and gram-negative bacteria account for 0.114 and 0.127 cases per 100,000 persons, respectively in the United States. Group B Streptococcus and Listeria monocytogenes remain important causes, but current data on their incidence are lacking. Neurosurgical procedures may place patients at risk for meningitis due to bacteria acquired at the time of surgery or in the postoperative period, including Staphylococcus aureus, coagulase-negative staphylococci, and gram-negative bacilli. In addition to bacteria, other pathogens may cause meningitis in at risk patients. Immunocompromised patients, such as solid-organ transplant patients and patients living with HIV infection, are at risk for fungal meningitis with Cryptococcus neoformans and encephalitis secondary to Toxoplasma gondii and JC virus. Tuberculosis can spread from pulmonary sites to cause clinical disease in the CNS. Life-threatening viral encephalitis and meningitis can occur in otherwise healthy, young individuals, as well as in patients immunocompromised by age or other factors.
Risk factors for CNS infections can be classified as follows: Environmental: Recent exposures (eg, close contact with meningitis or respiratory tract infection, contaminated foods), active or passive exposure to cigarette smoke, close living conditions Recent infection in the patient: Respiratory infection, otitis media, sinusitis, mastoiditis Immunosuppression: Anatomic or functional asplenia, sickle cell disease, alcoholism, cirrhosis, immunoglobulin or complement deficiency, cancer, HIV/AIDS, uncontrolled diabetes mellitus, debilitated state of health Surgery, trauma: Neurosurgery, head trauma, CSF shunt, cochlear implantt Noninfectious causes of meningitis include malignancy, medications (eg, sulfonamides, nonsteroidal antiinflammatory drugs [NSAIDs], IV immunoglobulin), autoimmune disease (eg, lupus), and trauma.
PATHOPHYSIOLOGY Meningitis is an inflammation of the membranes of the brain and spinal cord (meninges) and the CSF in contact with these membranes, whereas Contiguous spread occurs when infections in adjacent structures (eg, sinus cavities or the middle ear) invade directly through the blood brain barrier. Hematogenous seeding occurs when a remote infection causes bacteremia that seeds the CSF, such as pneumococcal pneumonia. Reactivation of latent infection results from dormant viral, fungal, or mycobacterial pathogens in the spine, brain, or nerve tracts. Direct inoculation of bacteria into the CNS is the result of trauma, congenital malformations, or complications of neurosurgery. Once through the blood brain barrier, pathogens replicate due to limited host defenses in the CNS. Neurologic tissue damage is the result of the host s immune reaction to bacterial cellular components, which trigger cytokine production, particularly tumor necrosis factor alpha (TNF- ) and interleukin 1 (IL-1), and other inflammatory mediators. Bacteriolysis resulting from antibiotic therapy further contributes to the inflammatory process. Cytokines increase permeability of the blood brain barrier, allowing influx of neutrophils and other host defense cells that contribute to the development of cerebral edema and increased intracranial pressure characteristic of meningitis. The increase in intracranial pressure is responsible for the hallmark clinical signs and symptoms of meningitis: headache, neck stiffness, altered mental status, photophobia, and seizures. Untreated, these pathophysiologic changes may result in cerebral ischemia and death. The CNS response to infection is cellular and chemical changes in the CSF. Ideally, LP to obtain CSF for direct examination and laboratory analysis, as well as blood cultures and other relevant cultures, should be obtained before initiation of antimicrobial therapy. However, initiation of antimicrobial therapy should not be delayed if a pretreatment LP cannot be performed. Normal CSF has a characteristic composition in terms of protein and glucose content, as well as cell count.
CLINICAL PRESENTATION AND DIAGNOSIS Signs and Symptoms 95% of patients with bacterial meningitis have two of the following: headache, fever, neck stiffness, and altered mental status Headache (87%) Nuchal rigidity (stiff neck) (83%) Fever (77%) Nausea (74%) Altered mental status (ie, confusion, lethargy, and obtundation) (69%) Focal neurologic defects (including positive Brudzinski sign and Kernig sign) (33%) Seizures Malaise, restlessness Photophobia Skin lesions (diffuse petechial rash observed in 50% of patients with meningococcal meningitis) Signs and symptoms in neonates, infants, and young children: nonspecific findings, such as altered feeding and sleep patterns, vomiting, irritability, lethargy, bulging fontanel, seizures, respiratory distress, and petechial/purpuric rash Predictors of an unfavorable outcome: seizures, focal neurologic findings, altered mental status, papilledema, hypotension, septic shock, and pneumococcal meningitis
Laboratory Tests CSF examination via lumbar puncture (LP, spinal tap);) Cloudy CSF Decreased glucose Elevated protein Elevated WBC (differential provides clues to offending pathogen) Gram stain (adequate for diagnosis in 60% 90% of patients with bacterial meningitis) Culture and sensitivity (positive in 70% 85% without prior antibiotic therapy, positive in less than 20% who have had prior therapy) If CSF Gram stain and/or culture is negative, rapid diagnostic tests (such as latex agglutination) may be useful; these tests are positive even if bacteria are dead Polymerase chain reaction (PCR; DNA amplification of the most common bacterial meningitis pathogens) may be useful to help exclude bacterial meningitis Elevated CSF lactate and C-reactive protein Blood cultures Other cultures should be obtained as clinically indicated (eg, sputum) WBC with differential Fungal meningitis: CSF culture, CSF and serum cryptococcal antigen titers, microscopic examination of CSF specimens Tuberculous meningitis: CSF culture, PCR evaluation (preferred), and acid-fast stain
Goals of Therapy The treatment goals for CNS infections are to prevent death and residual neurologic deficits, eradicate or control causative micro-organisms, ameliorate clinical signs and symptoms, and implement vaccination and suppressive measures to prevent future infections. Surgical debridement should be employed, if appropriate (as in postneurosurgical infections and brain abscess). Supportive care, consisting of hydration, electrolyte replacement, antipyretics, antiemetics, analgesics, antiepileptic drugs, and wound care (for surgical wounds), is an important adjunct to antimicrobial therapy, particularly early in the treatment course.
Treatment Principles Prompt initiation of IV high-dose bactericidal antimicrobial therapy directed at the most likely pathogen(s) is essential due to the high morbidity and mortality associated with CNS infections. a longer duration of symptoms and more advanced disease before treatment initiation increase the risk of a poor outcome. Initiation of antibiotic therapy as soon as possible after bacterial meningitis is suspected or proven (even before hospitalization) reduces mortality and neurologic sequelae. High-dose parenteral bactericidal antibiotic therapy is required to achieve CSF antibiotic concentrations adequate to rapidly sterilize the CSF and reduce the risk of complications. The presence of infection in the CSF reduces the activity of some classes of antibiotics. For example, the decreased pH of CSF associated with meningitis significantly reduces the activity of aminoglycoside antibiotics. Ability of antibiotics to reach and achieve effective concentrations at the infection site is the key to treatment success. The CSF penetration of most, but not all, antibiotics is enhanced by the presence of infection and inflammation. Sulfonamides, trimethoprim, chloramphenicol, rifampin, and most antitubercular drugs achieve therapeutic CSF levels even without meningeal inflammation Most -lactams and related antibiotics (ie, carbapenems and monobactams), vancomycin, quinolones, acyclovir, linezolid, daptomycin, and colistin achieve therapeutic CSF levels in the presence of meningeal inflammation. Aminoglycosides, first-generation cephalosporins, second-generation cephalosporins (except cefuroxime), clindamycin, and amphotericin do not achieve therapeutic CSF levels, even with inflammation, but clindamycin does achieve therapeutic brain tissue levels. An adequate duration of therapy is required to treat meningitis successfully. Parenteral (IV) therapy is administered for the full course of therapy for CNS infections to ensure adequate CSF penetration throughout the course of treatment. Antibiotic treatment (and dexamethasone, if used as a treatment adjunct) reduces the inflammation associated with meningitis, which, in turn, reduces the penetration of some antibiotics into the CSF, and parenteral therapy must be used throughout the entire treatment course to ensure adequate concentrations. Carefully selected patients who have close medical monitoring and follow-up may be able to receive a portion of their parenteral meningitis treatment on an outpatient basis.
Empirical Antimicrobial Therapy In most patients, a diagnostic LP will be performed before beginning antibiotics, but this never should delay initiation of antimicrobials. Empirical therapy should be directed at the most likely pathogen(s) . Empirical treatment regimens now include the combination of a third-generation cephalosporin plus vancomycin. Recognition of relative and high-level resistance to N. meningitidis in the laboratory, as well as in clinical treatment failures, has led to greater use of third-generation cephalosporins for empirical therapy of meningococcal meningitis. Treatment of suspected or proven -lactamase-mediated Hib meningitis also requires a third-generation cephalosporin. Increasing rates of methicillin-resistant S. aureus (about onethird of staphylococcal CSF isolates) and coagulase-negative staphylococci require the use of vancomycin for empirical therapy when these pathogens are suspected. Pathogen-Directed Antimicrobial Therapy Empirical antimicrobial therapy should be modified on the basis of laboratory data and clinical response. If cultures, CSF Gram stain, or antigen/antibody testing indicate a specific pathogen, therapy should be adjusted quickly as needed to ensure adequate coverage for the offending pathogen(s).
Neisseria Meningitidis Meningitis N. meningitidis CNS infections most commonly occur in children and young adults. From 11% to 19% of survivors of meningococcal meningitis experience long-term sequelae, including hearing loss, limb loss, and neurologic deficits. Nearly all meningococcal disease is caused by five serogroups: A, B, C, Y, and W-135. nearly 60% of cases occur in patients over 11 years of age. N. meningitidis colonizes the nasopharynx and usually is transmitted via inhaled respiratory droplets from patients or asymptomatic carriers. Meningococcal disease is often (approximately 50%) associated with a diffuse petechial rash, and patients may experience behavioral changes. Patients may develop fulminant meningococcal sepsis, characterized by shock, disseminated intravascular coagulation, and multiorgan failure. Meningococcal sepsis has a poor prognosis and carries a mortality rate of up to 80%, whereas the mortality rate with meningococcal meningitis alone is 13%. Patients with suspected meningococcal infection should be kept on respiratory isolation for the first 24 hours of treatment. Increasing penicillin resistance requires that third-generation cephalosporins now be used for empirical treatment until in vitro susceptibilities are known. Patients with a history of type I penicillin allergy or cephalosporin allergy may be treated with vancomycin. Treatment should be continued for 7 days, after which no further treatment is necessary.
Routine vaccination should be administered between ages 11 and 21 years , with quadrivalent vaccine that provides protection against serogroups A, C, Y, and W. In addition, individuals aged 2 through 54 years who are immunocompromised or those with recent disease exposure during community outbreaks should receive the quadrivalent vaccine. Additionally, children less than 2 years may also need quadrivalent vaccine, depending on risk factors. The quadrivalent conjugate meningococcal vaccine protects against four of the five serotypes causing invasive disease (A, C, Y, and W- 135). Meningococcal vaccines do not protect against serotype B, which causes more than 50% of the cases of meningococcal meningitis in children younger than 2 years. Meningococcal vaccines can be used in outbreak situations, with protective antibodies measurable within 7 to 10 days. Close contacts of patients with meningococcal infections should be evaluated for antimicrobial prophylaxis. Prophylactic antibiotics should be started as soon as possible, preferably within 24 hours of exposure and within 14 days. Recommended regimens, all of which are 90% to 95% effective, for adults include; rifampin 600 mg orally every 12 hours for 2 days, ciprofloxacin 500 mg orally for one dose, or ceftriaxone 250 mg intramuscularly for one dose. Regimens for children include rifampin 5 mg/kg orally every 12 hours for 2 days (less than 1 month of age), rifampin 10 mg/kg orally every 12 hours for 2 days (greater than 1 month of age), or ceftriaxone 125 mg intramuscularly for one dose (less than 12 years of age). It is not known whether close contacts who have been vaccinated will benefit from prophylaxis.
Streptococcus Pneumoniae Meningitis S. pneumoniae is the most common cause of meningitis in adults and in children younger than 2 years of age. Pneumococcus is associated with the highest mortality observed with bacterial meningitis in adults (14% 18%), and coma and seizures are more common in pneumococcal meningitis. Patients at high risk for pneumococcal meningitis include the elderly, alcoholics, splenectomized patients, patients with sickle cell disease, and patients with cochlear implants. At least 50% of pneumococcal meningitis cases are due to a primary infection of the ears, sinuses, or lungs. preferred empirical treatment now includes a third generation cephalosporin in combination with vancomycin. All CSF isolates should be tested for penicillin and cephalosporin resistance by methods endorsed by the CLSI. Once in vitro sensitivity results are known, therapy may be tailored (see Table 70 3). Patients with a history of type I penicillin or cephalosporin allergy may be treated with vancomycin. Treatment should be continued for 10 to 14 days, after which no further maintenance therapy is required. Antimicrobial prophylaxis is not indicated for close contacts. Administration of vaccines to high-risk individuals is a key strategy to reduce the risk of invasive pneumococcal disease. The 23-valent pneumococcal vaccine targets serotypes that account for more than 90% of invasive disease in high-risk patients. However, the 23-valent vaccine does not produce a reliable immunologic response in children younger than 2 years, nor does it reduce pneumococcal carriage. PCV13, a 13-valent vaccine introduced in 2010, confers protection against serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F, and 23F It is intended for use in children younger than 18 years in the same schedule as the 7-valent conjugate vaccine. PCV13 is specifically recommended for immunocompromised children aged 6 to 18 years.
Haemophilus Influenzae Meningitis Routine inoculation of pediatric patients against Hib has significantly reduced the incidence The Hib vaccine is also recommended for patients undergoing splenectomy. Hib meningeal disease is often associated with a parameningeal focus such as a sinus or middle ear infection. Due to -lactamase mediated resistance, the empirical treatment of choice is third-generation cephalosporins (eg, ceftriaxone and cefotaxime). Treatment should be continued for 7 days, after which no further maintenance therapy is required. Close contacts of patients with H. influenzae type B meningitis should be evaluated for antimicrobial prophylaxis. The risk of Hib meningitis in close contacts may be up to 200- to 1000-fold higher than in the general population. Rifampin (600 mg/day for adults; 20 mg/kg/day for children, maximum of 600 mg/day) is administered for 4 days. Rifampin prophylaxis is not necessary for individuals who have received the full Hib vaccine series. Exposed, unvaccinated children between 12 and 48 months of age should receive one dose of vaccine, and unvaccinated children 2 to 11 months of age should receive three doses of vaccine, as well as rifampin prophylaxis.
Listeria monocytogenes Meningitis L. monocytogenes is an intracellular gram-positive bacillus that contaminates foods, such as soft cheese, unpasteurized milk, raw meats and fish, processed meats, and raw vegetables. Bacteria from contaminated foods colonize the GI tract, pass into the bloodstream, and overcome natural cellular immune responses to cause infection. L. monocytogenes meningitis, usually observed in patients at extremes of age and in immunocompromised patients with depressed cellular immunity has an overall mortality rate of up to 30%. Only a limited number of antibiotics show bactericidal activity against Listeria. The combination of high-dose ampicillin or penicillin G and an aminoglycoside is synergistic and bactericidal against Listeria. A total treatment course of at least 3 weeks is required. Because of concerns about the risk of nephrotoxicity with an extended treatment course of aminoglycosides, patients are treated with combination therapy for 10 days and may finish out the remainder of their treatment with ampicillin or penicillin alone. In penicillin-allergic patients, trimethoprimsulfamethoxazole is the agent of choice due to documented in vitro bactericidal activity against Listeria, as well as good CNS penetration. Vancomycin and cephalosporins are not effective treatments for Listeria meningitis. Prophylaxis is not needed for close contacts, nor is suppressive therapy indicated. Patients with severe depression of cell-mediated immunity should be advised to avoid foods that may be contaminated with Listeria.
Group B Streptococcus Meningitis Infection with group B Streptococcus (eg, S. agalactiae) is the most common cause of neonatal sepsis and meningitis. Around 15% to 35% of pregnant women are a carrier of group B Streptococcus in the vagina or rectum. Group B streptococci can be acquired during childbirth after exposure to infected secretions from the mother s birth canal or rectum. Neonates born to women who are carriers are at very high risk (1 of every 100 200 babies) of developing invasive group B streptococcal disease. Neonatal meningitis is associated with significant morbidity and mortality. Synergistic treatment with penicillin or ampicillin, plus gentamicin, for 14 to 21 days is recommended for group B streptococcal meningitis. To reduce the risk of clinical group B streptococcal disease in neonates, pregnant women should be screened at 35 to 37 weeks gestation to determine whether they are carriers of group B streptococci. Intrapartum antibiotics (eg, penicillin or ampicillin) are recommended for pregnant women with the following characteristics: group B streptococcal carrier state detected at screening, history of group B streptococcal bacteriuria at any time during pregnancy, and history of delivery of infant with invasive group B streptococcal disease.
Gram-Negative Bacillary Meningitis Meningitis caused by enteric gram-negative bacilli is an important cause of morbidity and mortality in populations at risk, including : those with diabetes, malignancy, cirrhosis, immunosuppression, advanced age, and/or a defect allowing communication from skin to CNS (eg, neurosurgery, congenital defects, cranial trauma). The optimal treatment for gram-negative bacillary meningitis is not well defined. The introduction of extended-spectrum cephalosporins has improved patient outcomes significantly. Although the third-generation cephalosporins ceftriaxone and cefotaxime provide good coverage for most Enterobacteriaceae, these antibiotics are not active against P. aeruginosa. Ceftazidime, cefepime, and carbapenems are effective in pseudomonal meningitis. Addition of an aminoglycoside may improve treatment results; however, CNS penetration of aminoglycosides is extremely poor, even in the setting of inflamed meninges. Intrathecal or intraventricular administration of aminoglycosides may be useful, but intraventricular antibiotics have been associated with increased mortality in neonates. Intrathecal therapy is accomplished by administering the antibiotic into the CSF via LP, whereas intraventricular therapy is usually administered into a reservoir implanted in the ventricles of the brain. Initial therapy of suspected or documented pseudomonal meningitis should include an antipsuedomonal -lactam (eg, cefepime, meropenem) plus an aminoglycoside (eg tobramycin, amikacin). Although the carbapenem imipenem-cilastatin has similar activity to these -lactams, its use is not recommended in meningitis because of the risk of seizures. Aztreonam, high-dose ciprofloxacin, and colistin are alternative treatments for pseudomonal meningitis, although local susceptibility rates should be considered before initiating alternative therapy. Local therapy (ie, intrathecal or intraventricular therapy) may be indicated in patients with multidrug-resistant gram-negative bacillary meningitis or in patients who fail to improve on IV antibiotics alone. In cases of multidrug-resistant pathogens, alternative pharmacodynamic dosing strategies such as continuous or extended infusion of -lactam antimicrobials may be considered to optimize target attainment (time greater than minimum inhibitory concentration). Given the differences in local hospital resistance patterns, administration of pathogen-directed treatment is very important after microbiology results become available. Therapy for gram-negative bacillary meningitis should be continued for at least 21 days.
Viral Encephalitis and Meningitis Viral encephalitis and meningitis may mimic bacterial meningitis on clinical presentation but often can be differentiated by CSF findings The most common viral pathogens are enteroviruses, which cause approximately 85% of cases of viral CNS infections. Other viruses that may cause CNS infections include arboviruses, HSV, cytomegalovirus, varicella-zoster virus, rotavirus, coronavirus, influenza viruses A and B, West Nile virus, and Epstein-Barr virus. Viral CNS infections are acquired through hematogenous or neuronal spread. Most cases of enteroviral meningitis or encephalitis are self-limiting with supportive treatment. However, arbovirus, West Nile virus, and Eastern equine virus infections are associated with a less favorable prognosis. Without effective treatment, the mortality rate may be as high as 85%, and survivors often have significant residual neurologic deficits. In accordance with 2008 IDSA guidelines, high-dose IV acyclovir is the drug of choice, given for 2 to 3 weeks at a dose of 10 mg/kg IV every 8 hours in adults, based on ideal body weight, and for 3 weeks at a dose of 20 mg/ kg IV every 8 hours in neonates. Patients receiving acyclovir should maintain adequate hydration (consider continuous IV hydration) to help prevent acute kidney injury secondary to crystal nephropathy. Foscarnet 120 to 200 mg/kg/day divided every 8 to 12 hours for 2 to 3 weeks is the treatment of choice for acyclovir-resistant HSV
Opportunistic CNS Infections Cerebral Toxoplasmosis Across the globe, cerebral toxoplasmosis represents the most common focal brain infection in HIV infected patients. Infection rates in the United States vary but are reported to be approximately 15% among patients with AIDS. The majority of cases occur in patients with CD4+ cell counts less than 100 cells/mm3 (100 106 /L). Potent antiretroviral therapy and primary prophylaxis (first-line option is sulfamethoxazoletrimethoprim) in IgG-positive patients has greatly reduced the disease burden. First-line therapy in toxoplasmosis encephalitis is pyrimethamine plus sulfadiazine, given concomitantly with leucovorin to prevent severe hematologic adverse effects secondary to pyrimethamine. Clindamycin may be substituted for sulfadiazine in cases of contraindications to sulfa- based therapy. Sulfamethoxazole-trimethoprim may also be an option, specifically in patients unable to take oral therapy. Adjunctive corticosteroids and anticonvulsant therapy should be considered to reduce sequelae from the inflammatory process and control active seizures, respectively.
Cryptococcal Meningitis CNS disease secondary to Cryptococcus neoformans is primarily observed in severely immunocompromised hosts, such as those with HIV infection. Potent antiretroviral therapy has significantly reduced the disease burden from preantiretroviral therapy rates of 5% to 8% in developed countries. The majority of disease occurs in patients with CD4+ cell counts less than 50 cells/mm3 (50 106 /L). First-line therapy is considered amphotericin B deoxycholate 0.7 mg/kg IV daily plus flucytosine 100 mg/kg/day orally in four divided doses for a minimum of 2 weeks. Therapeutic drug monitoring may be considered for flucytosine to help reduce the risk of adverse effects. Development of renal dysfunction as a result of disease and/or drug toxicity should be closely monitored and may prompt dose reduction or possible switch to alternative lipid formulations of amphotericin, which may be less nephrotoxic. High-dose fluconazole is considered an alternative first-line therapy, especially in resource- limited areas. Secondary prophylaxis with fluconazole for an indefinite period is recommended following the completion of at least 2 weeks of induction therapy and 8 weeks of maintenance therapy with fluconazole.
Adjunctive Dexamethasone Therapy The adjunctive agent dexamethasone improves outcomes in selected patient populations with bacterial meningitis. Dexamethasone inhibits the release of proinflammatory cytokines and limits the CNS inflammatory response stimulated by infection and antibiotic therapy. Clinical benefit in reducing neurologic deficits (primarily by reducing hearing loss) has been observed in infants and children, if dexamethasone is initiated prior to antibiotic therapy. The American Academy of Pediatrics recommends dexamethasone (0.15 mg/kg IV every 6 hours for 2 to 4 days) for infants and children at least 6 weeks of age with Hib meningitis and consideration of dexamethasone in pneumococcal meningitis. In contrast to this recommendation, a large multicenter cohort study failed to show any mortality benefit of adjunctive dexamethasone therapy regardless of age or responsible pathogen (S. pneumoniae or N. meningitidis). Dexamethasone should be initiated 10 to 20 minutes before or no later than the time of initiation of antibiotic therapy; it is not recommended for infants and children who have already received antibiotic therapy because it is unlikely to improve treatment outcome in these patients. In adults, a significant benefit was observed with dexamethasone in reducing meningitis complications, including death, particularly in patients with pneumococcal meningitis. The IDSA recommends dexamethasone 0.15 mg/kg IV every 6 hours for 2 to 4 days (with the first dose administered 10 to 20 minutes before or with the first dose of antibiotics) in adults with suspected or proven pneumococcal meningitis. Dexamethasone is not recommended for adults who have already received antibiotic therapy. Some clinicians would administer dexamethasone to all adults with meningitis pending results of laboratory tests. There is controversy regarding the administration of dexamethasone to patients requiring vancomycin for pneumococcal meningitis. Animal models indicate that concurrent steroid use reduces vancomycin penetration into the CSF by 42% to 77% and delays CSF sterilization. A prospective evaluation in patients with pneumococcal meningitis receiving vancomycin and adjunctive dexamethasone demonstrated that adequate concentrations of vancomycin (nearly 30% of serum concentrations) were achievable in the CSF, provided appropriate vancomycin dosage was utilized. Treatment failures have been reported in adults with resistant pneumococcal meningitis who were treated with dexamethasone, but the risk benefit of using dexamethasone in these patients cannot be defined at this time.
OUTCOME EVALUATION Monitor patients with CNS infections continuously throughout their treatment course to evaluate their progress toward achieving treatment goals, including relief of symptoms, eradication of infection, and reduction of inflammation to prevent death and the development of neurologic deficits. These treatment goals are best achieved by appropriate parenteral antimicrobial therapy, including empirical therapy to cover the most likely pathogens, followed by directed therapy after culture and sensitivity results are known. Components of a monitoring plan to assess efficacy and safety of antimicrobial therapy of CNS infections include clinical signs and symptoms and laboratory data (eg, CSF findings, culture, sensitivity data). Monitoring of laboratory tests is important in patients receiving treatment for CNS infections. During the patient s treatment course, monitor clinical signs and symptoms at least three times daily. Trends are more important than one-time assessments. Expect fever, headache, nausea and vomiting, and malaise to begin to improve within 24 to 48 hours of initiation of antimicrobial therapy and supportive care. Evaluate the patient for such as altered mental status and nuchal rigidity, resolution of neurologic signs and symptoms, as the infection is eradicated and inflammation is reduced within the CNS. Expect improvement and subsequent resolution of signs and symptoms as the treatment course continues. At the time of hospital discharge, arrange outpatient follow-up for several weeks to months depending on the causative pathogen, clinical treatment course, and patient s underlying comorbidities.
Monitor CSF and blood cultures so that antimicrobial therapy can be tailored to the etiologic organisms. Follow-up cultures may be obtained to prove eradication of the organism(s) or treatment failure. Although repeat LP generally is not performed, consider repeat LP for patients who do not respond clinically after 48 hours of appropriate antimicrobial therapy, especially those with resistant pneumococcus who receive dexamethasone. Other candidates for repeat LP include those with infection with gram-negative bacilli, prolonged fever, and recurrent meningitis. Repeat the LP in neonates to determine the duration of therapy. Repeat LP also may be performed to relieve elevated intracranial pressure. Expect repeat blood cultures to become negative quickly during therapy and the serum WBC count to improve and normalize with appropriate antimicrobial therapy. Evaluate antimicrobial dosing regimens to ensure efficacy of the treatment regimen. Trough vancomycin concentrations of 15 to 20 mg/L (10 14 mol/L) are recommended for the treatment of CNS infections. Monitor patients for drug adverse effects, drug allergies, and drug interactions. The specific safety monitoring plan will depend on the antibiotic(s) used. Pay close attention to concomitant medications in patients on rifampin for treatment or prophylaxis. Rifampin is a potent inducer of hepatic metabolism and may reduce the efficacy of other drugs metabolized by the cytochrome P-450 enzyme pathway.
Patient Care Process Patient Assessment: Assess patient allergies, including severity of reactions Determine if patient has received recent antibiotics that may influence LP results or treatment decisions Determine from a medication history if any medicines may be associated with drug-induced aseptic meningitis Therapy Evaluation: Assess LP results, results of antigenic testing, and culture and susceptibility for additional data to help streamline therapy Monitor patient for any antimicrobial-related adverse events. Provide recommendations for necessary prophylaxis based on causative pathogen and exposure history Care Plan Development: Based on patient-specific factors and local susceptibility patterns, determine appropriate empirical antimicrobial treatment plan Collaborate with treatment team to ensure timely administration of antibiotic in relation to performing LP and obtaining blood cultures Collaborate with treatment team to determine appropriate administration of adjunctive corticosteroid therapy Follow-up Evaluation: Determine appropriate length of therapy for diagnosed CNS infection Provide recommendations for outpatient parenteral therapy as needed upon discharge from acute care facility
Thank you Thank you