Provider Adherence to Oral Chemotherapy Dose Adjustment Guidelines
The team led by Amy Fowler, MD, is exploring provider adherence to oral chemotherapy dose adjustment guidelines for childhood acute lymphoblastic leukemia (ALL). They emphasize the clinical importance of following dosing guidelines, including dose escalations based on specific criteria to optimize treatment effectiveness while minimizing risks. Non-adherence can lead to interruptions in therapy and inferior outcomes, highlighting the critical role of healthcare providers in managing ALL treatment.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Provider Adherence to Oral Chemotherapy Dose Adjustment Guidelines UT Clinical Safety & Effectiveness Conference San Antonio, TX October 27-28, 2011 Amy Fowler, MD Alexis Kennedy, CPNP Naomi Winick, MD
The Team Team Members CS&E Participants Amy Fowler, MD, Project Leader Alexis Kennedy, CPNP, Project Champion Team Members Naomi Winick, MD, Physician Champion Gretchen Hirschey, RN, Nursing Champion Jessica Rajian, RN, EPIC Champion Christian Tellinghuisen, Database support All the pediatric hematology/oncology fellows Facilitator - Pat Griffith, BS, MT, MBA
Childhood Acute Lymphoblastic Leukemia (ALL) Most common malignancy of childhood 50-60 new cases annually in Dallas About 150 children treated for ALL at any given time Current survival rates vastly improved Oral chemotherapy Important component of therapy 6-mercaptopurine (6MP) and methotrexate (MTX) Given daily, at home, for ~ 2-3 years Dosed based on degree of bone marrow suppression Published dosing guidelines for providers Specific rules for when to hold doses or dose escalate Target absolute neutrophil count (ANC): 500 1,500/ L
Clinical importance of dosing guidelines Degree of bone marrow suppression Lower ANC Improved survival Dose intensity of oral chemotherapy Greater dose intensity Improved survival Problem with excessive neutropenia (ANC <500) Risk of serious infections increases Results in held doses (chemo interruptions) Decreases dose intensity due to breaks in therapy Dose interruptions Greater dose interruptions Inferior survival Provider adherence impacts all of the above
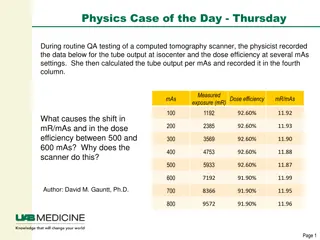
Dose Adjustment Guidelines Dose Escalations Dose escalation when current dose is 100% When ANC > 1,500 on 3 CBC over 6 weeks OR 2 successive monthly CBCs Alternate 6MP/MTX, and increase by 25% each time Dose escalation when current dose is <100% When ANC remains > 750 and platelets > 75K Increase doses by 25% every 2-4 weeks May increase both drugs simultaneously
Dose Adjustment Guidelines Holding for Neutropenia When ANC < 500 or platelets < 50K Hold doses of both 6MP & MTX Restart both 6MP & MTX After 1st drop Resume when ANC > 500 and platelets > 50K Restart at 100% prior dose After 2nd drop Resume when ANC >750 and platelets >75K Restart at 50% most recent dose 6
Background Data Overall ANC results from retrospective review 2006-2010 Average ANC Target ANC 7
Background Data Percentage of time providers adherent to indicated dose increases Adherence 39% Non- adherence 61% 8
Aim Statement Improve percentage of time that providers modify chemotherapy doses as indicated by protocol guidelines in children with ALL from 39% to over 75% From January 1, 2011 to May 31, 2011.
Measures of Success Provider adherence Proportion of times dose escalation made when indicated by the guidelines. Followed specific rules based on guidelines Used consistent and trained set of providers to make decision on appropriateness of dose escalations Goal to minimize variation in interpretation Goal to improve from 39% to >75% 10
Pareto Chart - Provider Survey Results Most common reason why providers neglect indicated dose escalations
Targets for Intervention Provider and nursing education Awareness of the clinical importance Review of guideline content Created flow-sheet Easy access to pertinent labs and dosing Posters with guidelines placed in provider work areas Change in process of clinic flow Timing of lab draws Results return prior to patient leaving clinic
Quality Improvement Timeline
Percent adherence per month compared to pre-intervention 100% 90% 80% Percent Adherence 70% 60% 50% Pre-intervention adherence = 39% 40% 30% 20% Baseline Jan-11 Feb-11 Mar-11 Apr-11 May-11 Jun-11
Absolute neutrophil count 2,400 2,200 2,000 Average ANC 1,800 1,600 1,400 1,200 1,000 Baseline Jan-11 Feb-11 Mar-11 Apr-11 May-11 Jun-11 Episodes of neutropenia per patient per month 0.4 Episodes of Neutropenia 0.35 per patient per month 0.3 0.25 0.2 0.15 0.1 0.05 0 Baseline 11-Jan 11-Feb 11-Mar 11-Apr 11-May 11-Jun
Conclusions Exceeded goal with 90% adherence Increased bone marrow suppression (ANC) No change in frequency of neutropenic episodes May increase length of dose interruptions Longer dose interruptions Theoretical risk of negative influence on survival rates Must weigh risks and benefits of improved adherence Universal buy-in Nursing staff Families Administration Providers (Mid-level and physician)
Challenges Data collection Very labor and time intensive Complex spreadsheets Clinical expertise needed for data evaluation Commitment from providers set in their ways Guidelines leaving room for interpretation Difficult to put $$ value on results
Next Steps Clinic to continue the interventions Continued monitoring Quarterly chart audits Introduce into EMR system Build reminders and flow sheets electronically Large scale, multi-institution collaborative Need to look at effect on survival rates Publish results Influence the Children s Oncology Group, organization creating new versions of guidelines