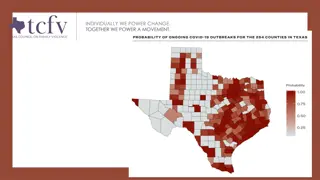
Public Benefits in Texas During the COVID-19 Pandemic
Learn about the public benefits available in Texas during the COVID-19 pandemic. Stay informed about the assistance programs and support offered through April 17, 2020, while understanding the potential for changes ahead.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Public Benefits in Texas During the COVID-19 Pandemic * PLEASE NOTE THE INFORMATION CONTAINED HEREIN IS ACCURATE THROUGH APRIL 17, 2020 AND SUBJECT TO CHANGE.
TESTING for COVID-19 Medicaid and CHIP will cover COVID-19 testing for Medicaid or CHIP clients. (Whether testing will be done will be determined by healthcare provider and local public health officials.) No prior authorization will be required on the COVID-19 lab test by Medicaid and CHIP health plans or by traditional Medicaid. Medicare Part B also covers testing at no charge when your doctor or other health care provider orders it. The Families First Coronavirus Response Act (Families First) and the Coronavirus Aid Relief and Economic Security (CARES) Act require comprehensive private health insurance plans to cover COVID-19 testing and related services without cost-sharing.
CHIP Co-payments are waived Office visit copayments for all CHIP members for services provided from March 13, 2020, through April 30, 2020 are waived. Co-payments are not required for covered services delivered via telemedicine or telehealth to CHIP members.
SNAP/TANF/MEDICAID RECERTIFICATIONS ARE EXTENDED 6 MONTHS Households with certification periods ending in: March 2020 are automatically extended through September 2020; April 2020 are automatically extended through October 2020; and May 2020 are automatically extended through November 2020. No action is needed to extend benefits. WORK REQUIREMENTS ARE WAIVED, all SNAP/TANF recipients will be treated as exempt.
SNAP Emergency Allotment Supplements Households who are approved for SNAP in April 2020 and May 2020 will automatically be issued emergency allotment (EA) supplements that will bring the household up to the maximum monthly allotment for the household s size. April EA benefits will be issued by April 15, 2020 May EA benefits will be issued by May 15, 2020. Note: SNAP households that already receive the maximum monthly allotment for their household size are not eligible for EA supplements.
Managed Care Face to Face Visits Face to face service coordination visits are suspended through the end of April 2020 for STAR Health, STAR Kids, STAR+PLUS Managed Care Organizations (MCOs), and Dual Demonstration Medicare- Medicaid Plans (MMPs). These are to be replaced with telephonic or telehealth outreach, if possible. Medically Dependent Children s Program (MDCP) and STAR+PLUS Home & Community Based Service (HCBS) assessments and reassessments, such as the SK-SAI and MN/LOC, may not be completed over the phone at this time . HHSC is extending enrollment in the Medically Dependent Children s Program (MDCP) and STAR+PLUS Home and Community Based Services (HCBS) for members with individual service plans (ISPs) expiring through April 2020. Dual Demonstration, STAR+PLUS, STAR Health and STAR Kids MCOs will: Extend enrollment for 90 days for members with ISPs expiring through April 2020. Assess the needs of these members within 90 days. Extend authorizations for waiver services for these members until the assessment occurs.
Medicaid Community Living Assistance and Support Services (CLASS) Therapies The following CLASS professional and specialized therapy services may be provided via telehealth through April 30: Physical therapy Occupational therapy Speech and language pathology Recreational therapy Music therapy Behavioral support Dietary services Cognitive rehabilitation therapy
Medicaid Appeals & Fair Hearings APPEALS now through the end of April 2020: Normally 60 days to request an Managed Care Organization (MCO) internal appeal, now 90 days. Normally 10 days to request continuation of benefits upon receipt of the adverse benefit determination, now 30 days. FAIR HEARING REQUESTS now through the end of April 2020 Normally 120 days to request a fair hearing after the internal MCO appeal, now 150 days. If the timeframe for a member to request a fair hearing would have expired in April 2020, they will have an extra 30 days from that expiration date to request a fair hearing.
MEDICAID/CHIP Prior Authorizations A prior authorization set to expire March 1, 2020 through the end of May 31, 2020, will be extended for 90 days. This extension does not apply to current authorizations for one-time services, new requests for authorization or pharmacy prior authorizations. For example, a single non-emergency ambulance trip would not be extended, but a recurring non-emergency ambulance authorization for dialysis would be extended.
Social Security Benefits & Supplement Security Income (SSI) PAYMENTS: regular monthly payments will continue to be paid either via direct deposit or mail. COVID-19 Economic Impact Payment: Social Security beneficiaries and Supplemental Security Income (SSI) Recipients who are not typically required to file tax returns will not need to file a tax return to receive an economic impact payment. * Note: SSA will not consider economic impact payments as income for SSI recipients, and the payments will be excluded from resources for 12 months. Medicaid will not consider economic impact payments as income for Medicaid recipients, and the payments will be excluded from resources for 12 months.
SSA Offices, Hearings & Deadlines All local Social Security offices are closed to the public for in-person service. Hearings will be conducted telephonically. A claimant may reject a telephonic hearing but it may be many months before that hearing can be rescheduled. SSA is extending deadlines wherever possible via their good cause policy to extend the time limits for submitting appeals and taking other actions during this pandemic. Still, claimants should contact SSA as soon as practically possible to request extensions.
SSA Continuing Disability Reviews & Overpayments SSA is not starting or completing any medical continuing disability reviews (CDRs), and has suspended processing and collecting most new overpayments. Some automated processes will still proceed because there are not enough SSA employees available to take the manual actions necessary to stop them. SSA will continue established collection activity for existing overpayments.
CONTACT INFO. MEDICAID/CHIP/SNAP/TANF Call 2-1-1 or go to www.YourTexasBenefits.com Note: SNAP and Medicaid: if you recently applied for SNAP or Medicaid or received a notice to call, you do not need to speak to anyone to complete your application. They will contact you if more information is needed. Social Security Administration (SSA) Online at www.ssa.gov Call 1-800-772-1213 (TTY 1-800-325-0778). Note: SSA has automated telephone services to get recorded information and conduct some business 24 hours a day. If you cannot handle your business through the automated services, you can speak to a Social Security representative between 8:00 am 5:30 pm. Monday through Friday.