Pulmonary Edema: Causes, Risk Factors & More
Explore the causes, incidence, and risk factors of pulmonary edema, a condition characterized by fluid accumulation in the lungs. Learn about cardiogenic and non-cardiogenic origins, potential triggers, and associated risks.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Pulmonary oedema Pulmonary oedema (wet lung) (wet lung) Presenter DeviNanjappan Principal [FACULTY OF NURSING]
Definition Definition Pulmonary edema is fluid accumulation in the tissue and air spaces of the lungs. It leads to impaired gas exchange and may cause respiratory failure. It is due to either failure of the left ventricle of the heart to remove blood adequately from the pulmonary circulation (cardiogenic pulmonary edema), or an injury to the lung tissue or blood vessels of the lung (non-cardiogenic pulmonary edema). Pulmonary edema is usually caused by a heart condition. Other causes include pneumonia, exposure to certain toxins and drugs, and being at high elevations.
Incidence Incidence The prevalence of pulmonary edema was estimated to be 75000-83000 cases per 100,000 individuals among heart failure patients with reduced ejection fraction. Pulmonary edema commonly affects individuals older than 65 years of age. Males are more commonly affected by pulmonary edema than woman.
Defining .... Defining ....
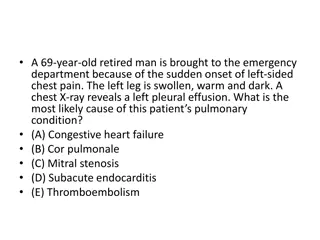
Causes Causes Cardiogenic Pulmonary edema is often caused by congestive heart failure. When the heart is not able to pump efficiently, blood can back up into the veins that take blood through the lungs. As the pressure in these blood vessels increases, fluid is pushed into the air spaces (alveoli) in the lungs. This fluid reduces normal oxygen movement through the lungs. These two factors combine to cause shortness of breath. Congestive heart failure that leads to pulmonary edema may be caused by: Heart attack, or any disease of the heart that weakens or stiffens the heart muscle (cardiomyopathy) Leaking or narrowed heart valves (mitral or aortic valves) Sudden, severe high blood pressure (hypertension)
Causes contd.......... Causes contd.......... Pulmonary edema may also be caused by(Non-Cardiogenic) Certain medicines High altitude exposure Kidney failure Narrowed arteries that bring blood to the kidneys Lung damage caused by poisonous gas or severe infection Major injury
Risk factor Risk factor history of pulmonary edema history of lung disease, such as tuberculosis or chronic obstructive pulmonary disorder (COPD) vascular (blood) disorders
Prevention Prevention the best way to try and prevent pulmonary edema is by taking good care of your health: Get a pneumonia vaccine. Get the flu vaccine, especially if you have heart problems or if you are an older adult. Remain on diuretics after an episode of pulmonary edema to prevent a reoccurrence. You can also decrease your risk for heart failure, the most common cause of pulmonary edema with the following steps: Visit your doctor regularly. Don t smoke or use recreational drugs. Get regular exercise. Eat healthy foods. Maintain a normal weight. Outlook for pulmon
PE Pathophysiology Cardiogenic pulmonary edema (CPE) is defined as pulmonary edema due to increased capillary hydrostatic pressure secondary to elevated pulmonary venous pressure. CPE reflects the accumulation of fluid with a low-protein content in the lung interstitium and alveoli as a result of cardiac dysfunction Non-cardiogenic pulmonary edema pulmonary edema can develop in patients without any known cardiac disease as well with any underlying pathology. The etiology of this clinical condition is governed by starling's law (the relationship between stroke volume and end diastolic volume.
PE Pathophysiology Neurogenic pulmonary edema The clinical manifestations in this of pulmonary edema can be attributed to disturbed autonomic nervous system with resultant exaggerated sympathetic discharge thereby raising the pulmonary capillary pressure and extravasations of fluid into pulmonary tissues Anaphylaxis causing pulmonary edema This type of clinical entity is very difficult to diagnose as majority of times the patient seems to be exposed to multiple known and unknown etiological factors. The accumulation of fluid in the pulmonary tissues is mainly an end result of allergic reaction during the peri-operative period Negative pressure pulmonary edema(NPPE) NPPE is a Pathophysiological syndrome which results due to acute development of negative intrathoracic pressure generated during spontaneous respiratory efforts against an obstructed upper airway.
Clinical S/S The symptoms for long-term pulmonary edema include: shortness of breath when being physically active difficulty breathing when lying down wheezing waking up at night with a breathless feeling that goes away when you sit up rapid weight gain, especially in the legs swelling in the lower part of the body fatigue
Clinical S/S High-altitude pulmonary edema Pulmonary edema due to altitude sickness, or not getting enough oxygen in the air, will have symptoms that include: headaches irregular, rapid heartbeat shortness of breath after exertion and during rest coughing fever difficulty walking uphill and on flat surfaces
Diagnosis PE an increased heart rate rapid breathing a crackling sound from your lungs any abnormal heart sounds tests used in diagnosing pulmonary edema include: complete blood count echocardiogram, or an ultrasound, to check for abnormal heart activity chest X-ray to see fluid blood tests to check oxygen levels electrocardiogram (ECG) to look for heart rhythm problems or signs of a heart attack
Treatment Preload reducers. These help decrease pressures from the fluid going into your heart and lungs. Diuretics also help reduce this pressure by making you urinate, which eliminates fluid .Afterload reducers. These medications dilate your blood vessels and take pressure off your heart. Nitroprusside (Nitropress) Heart medications. These will control your pulse, reduce high blood pressure, and relieve pressure in arteries and veins. Morphine. This narcotic is used to relieve anxiety and shortness of breath. But fewer doctors today use morphine due to the risks. CPAP(Continuous positive airway pressure )
Treatment Treatments for high-altitude pulmonary edema (HAPE) also include: Immediately descending to a lower elevation. If you're climbing or traveling at high altitudes and have mild symptoms of HAPE, descend 1,000 to 3,000 feet (about 300 to 1,000 meters) as quickly as you can, within reason. Depending on the severity of your condition, you may need rescue assistance to get off the mountain. Stop exercising and stay warm. Physical activity and cold can make pulmonary edema worse. Medication. Some climbers take prescription medications such as acetazolamide or nifedipine (Adalat CC, Procardia) to help treat or prevent symptoms of HAPE. To prevent HAPE, medication is started at least one day before ascent.
Presenter DeviNanjappan Principal [FACULTY OF NURSING]
Definition Definition Shock is the state of insufficient blood flow to the tissues of the body as a result of problems with the circulatory system. Shock is defined as a state of cellular and tissue hypoxia due to either reduced oxygen delivery, increased oxygen consumption, inadequate oxygen utilization, or a combination of these processes
Incidence Incidence This most commonly occurs when there is circulatory failure manifested as hypotension (ie, reduced tissue perfusion); It is crucial to recognize that a patient in shock can present hypertensive, normotensive, or hypotensive. Shock is initially reversible, It must be recognized and treated immediately to prevent progression to irreversible organ dysfunction.
Causes Causes Shock is a common end point of many medical conditions. Shock itself is a life-threatening condition as a result of compromised body circulation Type Cause Low volume Fluid loss such as bleeding or diarrhea Heart Ineffective pumping due to heart damage Obstructive Blood flow to or from the heart is blocked Distributive Due to abnormal flow within the small blood vessels
Risk factors Risk factors Risk factors Are older. Have a history of heart failure or heart attack. Have blockages (coronary artery disease) in several of your heart's main arteries. Have diabetes or high blood pressure. Are female.
Prevention Prevention Prevention of Shock: Shock can be prevented by reducing the incidence of the causes, such as heart failure, injuries, dehydration
Types of shock Types of shock Septic shock results from bacteria multiplying in the blood and releasing toxins. Common causes of this are pneumonia, urinary tract infections, skin infections (cellulitis), intra-abdominal infections (such as a ruptured appendix), and meningitis. Anaphylactic shock is a type of severe hypersensitivity or allergic reaction. Causes include allergy to insect stings, medicines, or foods (nuts, berries, seafood), etc. Cardiogenic shock happens when the heart is damaged and unable to supply sufficient blood to the body. This can be the end result of a heart attack or congestive heart failure. Hypovolemic shock is caused by severe blood and fluid loss, such as from traumatic bodily injury, which makes the heart unable to pump enough blood to the body, or severe anemia where there is not enough blood to carry oxygen through the body. Neurogenic shock is caused by spinal cord injury, usually as a result of a traumatic accident or injury.
Pathophysiology Pathophysiology