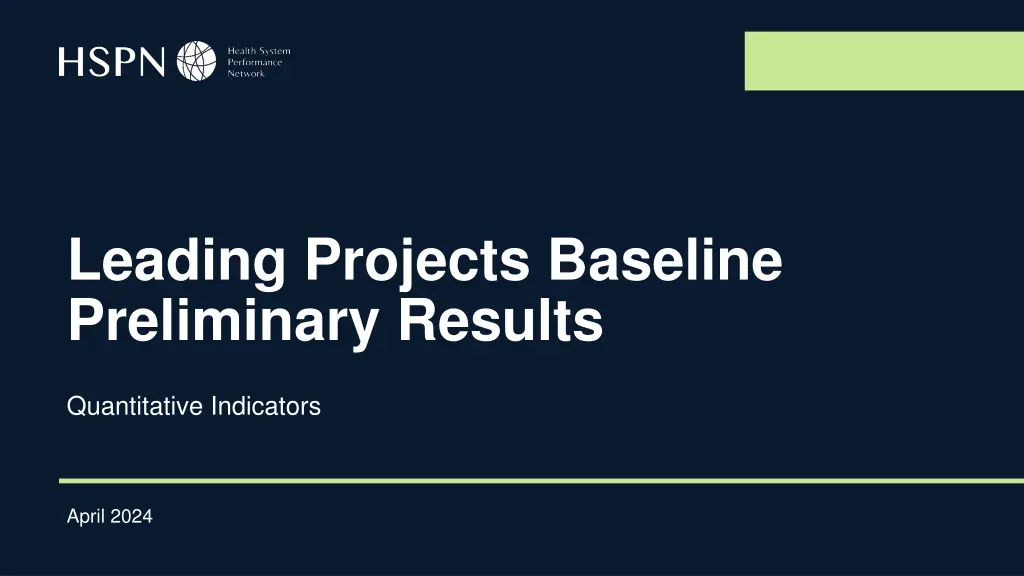
Quantitative Analysis of Leading Projects Baseline & Preliminary Results
Explore the preliminary results of leading projects, showcasing quantitative indicators for April 2024. Delve into population definitions, cross-project indicators, and palliative care indicators to assess program effectiveness and outcomes against expectations.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Leading Projects Baseline Preliminary Results Quantitative Indicators April 2024
Purpose of Preliminary Results Show calculated baseline results based on identifiable comparable eligible populations for each of the programs. Discuss validity of results compare to expectation or alternative sources. 2
Population definition General criteria: Individuals who received home care* and home care services in fiscal year 2022/23. Individuals receiving palliative care were included/excluded based on comprehensive definition, extending beyond home care. *Excluding Nipissing Wellness OHT, where individuals did not need to be receiving home care. 3
Cross Project Indicators Name General Definition Number of home care services provided per month in HC. Service volume Service unit-time for services provided per month in HC. Service time per patient-month Average length of home care enrollment per admission. Time receiving home care Proportion of admissions where the patient waited more than 3 days between referral and first HC service. Timeliness of service initiation (referral to first service within 3 days) Average number of days between referral and first HC service. Average wait time from referral to service Average number of days between assessment and first HC service Average wait time from assessment to service Change in MDSHSI score among home care clients that had two interRAIHC assessments in a 365-day period. Change in health status Average attributable total government health care spending per individual, per month alive. Total cost Average attributable government health care spending per individual, per month alive for homecare costs. Homecare costs ED visits for conditions best managed elsewhere Percentage of patients or clients who visited the emergency department (ED) for conditions best managed elsewhere". Percentage of home care clients who experienced an unplanned admission to hospital for medical reasons. Unplanned hospitalizations Proportion of days in acute inpatient care that were spent in alternate level of care (ALC). Alternate level care days Proportion of hospitalisations which had ALC days. Alternate level of care conversion Percentage of home care clients who reported that their primary informal caregiver expressed continued feelings of distress, anger or depression over a six-month period. Caregiver distress 4
Palliative Indicators Name General Definition The proportion of decedents that had one or more unplanned emergency department visits in their last 30 days of life. ED visits in the last 30 days of life The proportion of decedents that had one or more palliative home care services (excluding care management and placement services) in their last 90 days of life. Proportion of decedents receiving palliative home care in the last 90 days of life Average days at home (180 minus total days in hospital, emergency department, inpatient rehab and complex continuing care) in the last 6 months of life. Days spent at home in the last 6 months (180 days) of life The proportion of decedents that died in a hospital setting (defined as acute or psychiatric care institution, emergency department, inpatient rehab or complex continuing care. Deaths in hospital 5
Demographics Access to material resources (n=6,743) Age (n=6,772) Mean (SD): 75.6 (14) Median (IQR): 78 (68-86) Interpretation: Q1 would be living in neighbourhoods with the most access to material resources and Q5 with the least access. Sex (n=6,772) 6
Indicator: Service volume per patient-month 40 Average number of home care services received per patient- month in eligible reporting period. Average # of services per patient-month 30 29.6 24.7 Numerator: Total number of services in the reporting period. 20 19.8 17.1 15.2 Denominator: Total person- months in the reporting period. 10 11.2 9.6 0 Leading project (anonymized) 7
Indicator: Proportion of service volume by type 100% Reporting categories: 80% Physio or occupational therapy: Service = 5, 6 (visit) % of services volume Nursing: Service = 1 (visit), 2 (hours) Physio-occ Nursing Home-personal Case mgm Other 60% Personal services, homemaking, or both: 11, 12, 13 (hours) 40% Social work or case management: 8, 10, 14 (visit) Other: all other codes 20% 0% Leading project (anonymized) 8
Indicator: Service time per patient-month 35.0 30.0 31.3 25.0 Average service unit-time per month in home care. service unit-time 20.0 20.2 19.5 Visits without a recorded time have been counted as 1 hour. 15.0 13.9 12.2 10.0 10.8 8.8 5.0 0.0 Leading project (anonymized) 9
Indicator: Wait time of 3 days or less between referral and service Proportion of individuals who waited 3 days or less between referral and first HC service. 75% Numerator: Number of patients who waited no more than 3 days between referral* and first service. Patients must have been referred in reporting period. % waiting 3 days or less 56% 50% 45% 45% 43% 43% 33% 25% Denominator: Total number of patients referred in reporting period. 0% *If in hospital, start of count is date discharged. **Data suppressed Leading project (anonymized) 10
Indicator: Average wait time from referral to service 25.0 23.6 Average number of days between referral and first HC service. 20.0 Numerator: Number of days between referral and first service. Patients must have been referred in reporting period. 15.0 # of days 15.1 12.0 12.0 10.0 10.1 Denominator: Total number of patients referred in reporting period. 6.3 5.0 4.9 0.0 Leading project (anonymized) 11
Indicator: Average wait time from assessment to service 25.0 Average number of days between assessment and first HC service. 22.9 20.0 Numerator: Number of days between assessment and first service. Patients must have been referred in reporting period. 15.0 # of days 11.6 10.0 9.9 9.5 Denominator: Total number of patients referred in reporting period. 6.4 5.0 4.1 2.0 0.0 Leading project (anonymized) 12
Indicator: Change in health status Change in MDSHSI score among home care clients that had two interRAIHC assessments in a 365-day period. 0.05 Average change in health status 0.00 -0.02 Numerator: Total change in MDSHSI in eligible population. -0.03 -0.04 Denominator: Total population with an interRAIHC assessment in the observation period (index assessment) and a second interRAIHC assessment within 365d prior. -0.05 -0.09 -0.10 Leading project (anonymized) 13
Indicator: Monthly government spending $10,000 Average attributable government health care spending per individual, per month alive in FY22-23. $8,000 Average costs per patient-month $489 $1,883 $1,249 $6,000 Numerator: Total eligible patient costs. $4,000 $7,263 $6,335 Denominator: Total number of patient-months. $766 $638 $5,488 $1,111 $743 $2,000 $2,446 $2,440 $2,082 $1,951 $0 Other costs Home care costs Leading project (anonymized) 14
Indicator: Proportion of inpatient days that were ALC 30% Proportion of days in acute inpatient care that were spent in alternate level of care (ALC). 26.6% Proportion of inpatient days as ALC 21.6% 21.5% 20% Numerator: Total number of inpatient days designated as ALC in the reporting period. 18.2% 15.6% 14.4% Denominator: Total number of inpatient days in the reporting period. 10% 0% Leading project (anonymized) 15
Indicator: Proportion of hospitalisations with ALC days 100% Proportion of hospitalizations which became ALC. % of hospitalisations with ALC days 75% 76.5% Numerator: Total number of hospitalizations which became ALC. 50% Denominator: Total number of hospitalizations. 25% 21.9% 19.8% 16.9% 15.0% 9.8% 9.3% 0% Leading project (anonymized) 16
Indicator: Unplanned hospitalizations 75% Percentage of home care clients who experienced an unplanned admission to hospital for medical reasons. % of patients with unplanned hospitalisation 53.7% 50% Numerator: Total number of patients who had an unplanned hospitalization. 41.0% Denominator: Total number of patients in cohort. 25% 22.3% 18.2% 17.9% 16.8% 14.8% 0% Leading project (anonymized) 17
Indicator: ED visits for conditions best managed elsewhere 5% % with an ED visit best managed Percentage of patients or clients who visited the emergency department (ED) for conditions best managed elsewhere". 4% 3.4% 3% elsewhere 2.8% Numerator: Total number of patients who had an unplanned ED visit. 2% 2.2% 2.1% 1.7% 1.6% 1% Denominator: Total number of patients in cohort. 0% Leading project (anonymized) 18
Indicator: Caregiver distress 100% Percentage of clients who reported that their primary informal caregiver expressed continued feelings of distress, anger or depression over a six-month period. % with a caregiver experiencing distress 80% 76% 64% 60% Numerator: Total number of patients who reported that their primary informal caregiver expressed continued feelings of distress, anger or depression. 58% 55% 40% 40% 37% Denominator: Total population with an interRAI assessment in observation period that had a caregiver. 20% 0% Leading project (anonymized) 19
Palliative care indicators Palliative home care visit in last 90 days ED visits in last 30 days 80% 70% % of decedents with palliative visit in last 90 70% 65% 60% % of decedents with ED visit in last 30 68% 60% 50% 50% 40% days of life days 40% 30% 30% 20% 20% 10% 10% 0% 0% The percent of decedents receiving a palliative home care visit in the last 90 days of life. The percent of decedents with 1 or more emergency department visits in the last 30 days of life. 20
Palliative care indicators Deaths in hospital (alternate to deaths in location of choice) Days spent at home in last 6- months of life 180 50% Days spent at home in last 6 months of life 45% 160 161 Days spent at home in last 6 months of 44% 40% 140 35% 120 30% 100 25% life 80 20% 60 15% 40 10% 5% 20 0% 0 The percent of decedents that died in a hospital setting. Days spent at home in the last 6 months (180 days) of life. 21 21
Notes This research was supported by a grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC) to the Health System Performance Research Network. This study was supported by ICES, which is also funded by an annual grant from the MOHLTC. The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. Parts of this material are based on data and/or information compiled and provided by CIHI. However, the analyses, conclusions, opinions and statements expressed in the material are those of the author(s), and not necessarily those of CIHI. Parts of this material are based on data and information provided by Ontario Health (OH). The opinions, results, view, and conclusions reported in this paper are those of the authors and do not necessarily reflect those of OH. No endorsement by OH is intended or should be inferred. We thank the Toronto Community Health Profiles Partnership for providing access to the Ontario Marginalization Index. 22
Technical Appendix Technical Appendix 23